Published online Jul 26, 2020. doi: 10.12998/wjcc.v8.i14.3074
Peer-review started: January 15, 2020
First decision: April 21, 2020
Revised: June 23, 2020
Accepted: June 30, 2020
Article in press: June 30, 2020
Published online: July 26, 2020
Processing time: 187 Days and 5.3 Hours
Intra-abdominal hemorrhage during pregnancy is a rare and dangerous complication of pregnancy. In this article, we report 4 cases of intra-abdominal hemorrhage during pregnancy, including the spontaneous rupture of uterine veins, spontaneous rupture of liver, rupture of external iliac vessel branch, and rupture of right renal hamartoma.
The clinical manifestations of three patients lacked specificity, and the localization of the bleeding was not clear prior to surgery. All 4 pregnant women were successfully treated, while only one full-term infant survived.
There are diverse causes of intra-abdominal hemorrhage during pregnancy in clinic, and it is clinically characterized by acute abdominal pain during pregnancy. Clear diagnosis before surgery is rather difficult. Early diagnosis, timely and appropriate treatment and surgery, and multidisciplinary cooperation are key to saving pregnant females’ lives and improving the outcomes of perinatal infants.
Core tip: Intra-abdominal hemorrhage during pregnancy is clinically rare, which is dangerous. The disease is characterized by high perinatal mortality, and delayed treatment can even lead to maternal death. Thus, obstetricians need to be vigilant in clinical work, especially for patients with high-risk factors, such as HELLP (hemolysis, elevated liver enzymes, low platelet count) syndrome, endometriosis, and multiple abdominal surgery history. Early diagnosis, timely surgery, and multidisciplinary cooperation are the keys to save maternal life and improve perinatal outcomes.
- Citation: Yang L, Liu N, Long Y. Intra-abdominal hemorrhage during pregnancy: Four case reports. World J Clin Cases 2020; 8(14): 3074-3081
- URL: https://www.wjgnet.com/2307-8960/full/v8/i14/3074.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i14.3074
Intra-abdominal hemorrhage during pregnancy is a rare and dangerous complication of pregnancy. It is characterized by high perinatal mortality, and delay in treatment may even lead to maternal death. Common obstetric causes mainly include the rupture of uterine scars, aberrant placental implantation, and rupture of rudimentary uterine horn of pregnancy. On the other hand, rarely seen causes include rupture of subserosal uterine vessels, pelvic and abdominal vascular rupture, rupture of parenchymal organs (such as liver, spleen, and kidney), and idiopathic intra-abdominal hemorrhage[1-7]. In this article, 4 cases of intra-abdominal hemorrhage during pregnancy due to rare causes who were admitted to our hospital from January 2013 to November 2019 are reported.
Demographic data, diagnosis, management, and complications of the 4 cases are shown in Table 1.
| Case | Bleeding site | Onset of pregnancy wk | High-risk factors | Clinical manifestation | Preoperative hemoglobin, g/L | Ultrasonography | Celiac/posterior fornix puncture | Fetal outcome | Preoperative diagnosis | Intra-abdominal bleeding, mL |
| 1 | Uterine vein | 29 + 1 | Uterine malformation | Lower abdominal pain, nausea, dizziness, palpitations, and anal bloating | 88 | Intraperitoneal bleeding | Posterior fornix puncture | Fetal death | Uterine rupture | 1900 |
| 2 | Liver | 36 + 6 | Chronic hypertension | Lower abdominal pain, and dizziness | 95 | Intraperitoneal bleeding | Ultrasound-guided abdominal puncture | Fetal death | Rupture of subserosal vessel | 2000 |
| 3 | Right external iliac vessel branch | 18 + 1 | Uterine adenoma, twin pregnancy | Diffuse abdominal pain, nausea, and vomiting | 101 | Intraperitoneal bleeding | Ultrasound-guided abdominal puncture | Termination of pregnancy | Uterine rupture | 2300 |
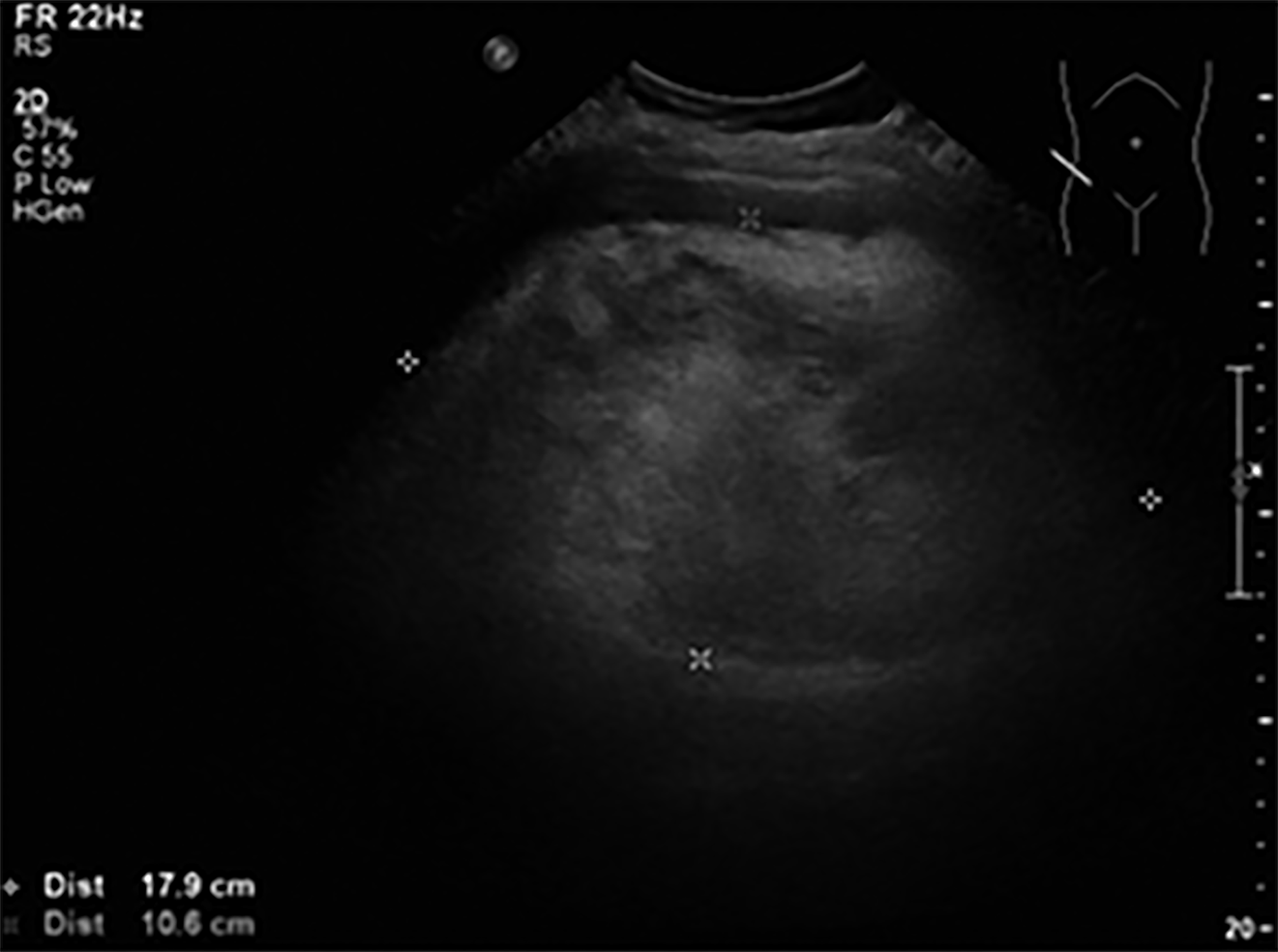
| 4 | Right kidney hamartoma | 38 + 5 | None | Right back pain | 105 | High echo in right kidney area (17.9 cm × 10.9 cm × 11.0 cm), liquid dark area behind uterus | None | Survived | Rupture of right kidney hamartoma | 1300 (300 mL abdominal hemorrhage, and 1000 mL retroperitoneal hemorrhage) |
Chief complaints: A 23-year-old primigravida at 29 + 1 wk' gestation presented with sudden lower abdominal pain of 7 h' duration accompanied by nausea, vomiting, dizziness, and anal straining feeling.
History of present and past illness: She had a smooth antenatal course with no recent history of trauma or intercourse. She had a free previous medical history.
Physical examination: Blood pressure 90/60 mmHg; pulse 90 beats/min; pale face; uterine fundus at three fingers above the umbilicus; fetal heart rate 60 beats/min; no contractions. She had lower abdominal direct and rebound tenderness and cervical motion tenderness with bulging posterior fornix.
Laboratory examinations: Her hemoglobin level was 88 g/L, and hematocrit was 26%.
Imaging examinations: Urgent ultrasound examination revealed uterine didelphus malformations with the pregnancy in the right uterus and fetal bradycardia down to 81 beats/min. A large amount of fluid was seen in the pelvis and abdominal cavity.
Further diagnostic work-up: Posterior culdocentesis yielded non-coagulable blood.
Primary diagnosis: Accordingly, rupture of rudimentary uterine horn of pregnancy was considered.
Chief complaints: A 33-year-old primigravida at 36 + 6 wk' gestation was admitted with lower abdominal pain of 6 h' duration accompanied with dizziness and fatigue.
History of present and past illness: She denied any history of chronic disease or surgery, with no recent intercourse or trauma and no preeclampsia nor HELLP (hemolysis, elevated liver enzymes, low platelet count) syndrome. Her blood pressure fluctuated over the range of 130-140/70-90 mmHg at 17 wk of pregnancy.
Physical examination: Blood pressure 102/62 mmHg; pulse 80 beats/min; pale face; no obvious direct or rebound tenderness over the abdomen. Uterine contraction was noted every 2-3 min with absent fetal heart rate.
Laboratory examinations: Her hemoglobin level was 95 g/L, and her hematocrit was 28.9%.
Imaging examinations: Urgent bedside ultrasound indicated intrauterine fetal death, with no abnormalities in the placenta. Plenty of fluid was found in the abdominal cavity.
Further diagnostic work-up: Ultrasound-guided paracentesis showed old blood.
Primary diagnosis: Accordingly, the rupture of subserosal vessel was considered.
Chief complaints: A 39-year-old primigravida, product of in vitro fertilization and twin gestation, presented to the hospital at 18 + 1 wk' gestation with abdominal pain of 9 h' duration accompanied by nausea and vomiting.
History of present and past illness: The patient had previous history of myomectomy 5 years prior to admission followed 4 years later by laparoscopic adhesiolysis plus left salpingectomy. Trauma and recent intercourse were denied.
Physical examination: Examination revealed a body temperature of 36.5 °C; blood pressure of 120/71 mmHg; and pulse rate of 100 beats/min. There was diffuse direct and rebound abdominal tenderness. The uterine fundus was at the umbilicus with no contractions and normal fetal heart rates.
Laboratory examinations: The hemoglobin level was 101 g/L, and the hematocrit was 28.7%.
Imaging examinations: Urgent bedside ultrasound indicated that both fetuses were normal, and the placenta covered the cervical ostium, with a large amount of fluid in the lower abdomen (left and right), liver and spleen areas, and upper abdominal cavity, which was confirmed to be blood on ultrasound-guided paracentesis.
Primary diagnosis: In view of previous history of myomectomy, uterine rupture was considered.
Chief complaints: A 30-year-old gravida 2, para 0 was admitted to the hospital at 38 + 5 wk' gestation with paroxysmal right back pain of 3 h' duration with no vomiting or dizziness.
History of present and past illness: No history of chronic disease, previous surgery, or renal tumors or stones was elicited. The patient had smooth pregnancy, during which no abdominal ultrasound was performed.
Physical examination: The blood pressure was 100/70 mmHg; the pulse rate was 90 beats/min; and there was obvious throbbing pain in right kidney area, without abdominal tenderness or rebound pain. There were irregular contractions, with normal fetal heart.
Laboratory examinations: Hemoglobin level was 105 g/L, and hematocrit was 34.3%.
Imaging examinations: Urgent urology ultrasound showed a hyperechoic space occupying lesion (17.9 cm × 10.9 cm × 11.0 cm) in the right renal region (Figure 1), which is suggestive of right kidney hamartoma rupture. Obstetric ultrasound showed normal fetal heart and normal placenta.
Primary diagnosis: Kidney stone was first considered.
The final diagnosis of the presented case was spontaneous rupture of subserosal vein on the posterior uterine wall.
The final diagnosis of the presented case was spontaneous rupture of liver.
The final diagnosis of the presented case was spontaneous rupture of right external iliac vessel branch.
The final diagnosis of the presented case was rupture of right kidney hamartoma.
The patient underwent an exploratory laparotomy under epidural anesthesia. Intra-operatively, 1900 mL of fresh and clotted blood was retrieved from the abdominal cavity. The didelphic uterus was confirmed, but the right uterine horn harboring the pregnancy was intact. Clots were observed on the posterior surface of the uterus. Due to the obstructed view by the gravid uterus, the patient was subjected to the low segment cesarean section and gave birth to a stillborn female infant, weighing 1200 g. After completion of the cesarean delivery, the cause of bleeding was identified to be a ruptured subserosal vein on the posterior uterine wall. Bleeding was controlled. No adhesions that could have caused avulsion of the vessel were detected throughout the pelvic cavity. The patient was transfused with six units of packed red-blood cells intra-operatively.
Exploratory laparotomy was performed under general anesthesia and 2000 mL blood was retrieved from the abdominal cavity. A low segment cesarean section was done, and she gave birth to a stillborn weighing 3150 g. After suturing the uterus, the source of bleeding was localized to the upper abdominal liver area. The liver had fatty changes, and there was massive bleeding from the visceral and parietal surfaces of the right lobe of the liver, with large blood clots stuck to the liver surface. Intermittent mattress suturing and gauze compression were used to stop the bleeding. The patient lost a total of 4000 mL blood, and she was transfused with eight units of packed red-blood cells and 1200 mL plasma, with 900 mL autologous blood transfusion.
The patient was subjected to an immediate exploratory laparotomy, and 2300 mL of blood was cleared from the abdominal cavity. No bleeding was detected in the hepatosplenic region, omentum, or mesentery. The posterior uterine wall was densely adherent to the rectum, and the double-layered broad ligament was extensively adherent to the pelvic sidewalls. The peritoneum of the right pelvic wall was partially lacking, and the right external iliac vessel branch was ruptured and bleeding, which was sutured to stop bleeding. During the operation, eight units of red-blood cells, 600 mL plasma, and 1000 mL autologous blood were transfused.
The emergency physician gave the patient 20 mg progesterone intramuscularly to promote stone excretion and relieve renal colic pain[8]. Urology ultrasound suggested right kidney hamartoma rupture. Exploratory laparotomy was done, and 300 mL free blood in the abdominal cavity was retrieved. Lower uterine cesarean section was performed, and a baby boy was delivered, weighing 2750 g with 6-9 and 10 Apgar scores. After the uterus was sutured, the right kidney was noted by the urologist to have a dark-red surface, and hematomas in peri-renal fat and about 1000 mL blood clots were removed. Right nephrectomy with tumor resection was done, and the final pathology was angiomyolipoma. During the operation, eight units of packed red-blood cells and 800 mL plasma were transfused.
The outcome of the pregnancy was stillbirth. The patient had an uneventful postoperative clinical course while hospitalized. The patient was discharged 7 d after surgery when the wound healed. The patient was subjected to the postoperative review after returning to her place of residence.
The outcome of the pregnancy was stillbirth. After surgery, the patient was kept in the intensive care unit, and the hepatic gauze pads were removed at 6 d post-operatively. A drain was left in the abdomen that drained 2000 mL of peritoneal fluid with no recurrent bleeding. The patient was discharged 45 d after surgery.
On post-operative day 3 the patient suffered from massive vaginal bleeding, and an urgent cesarean section was performed. Due to the difficulty in controlling postpartum hemorrhage, total hysterectomy was performed with estimated blood loss of 4000 mL. The outcome of the pregnancy was stillbirth. The patient was discharged 7 d after surgery.
The outcome of the pregnancy was fetal survival. The patient recovered and was discharged 12 d after the operation.
Intra-abdominal hemorrhage is a very rare but extremely dangerous complication of pregnancy. The perinatal mortality rate is as high as 31% to 36%. Due to improvements in surgical technique, the maternal mortality rate has decreased significantly[9,10]. The etiology of the 4 patients reported herein mainly involved spontaneous rupture of uterine veins, spontaneous liver rupture, rupture of external iliac vessels, and rupture of right renal hamartoma. These 4 cases are rarely seen, the onset of which might coincide with pregnancy, delivery, and postpartum, but mostly during the late pregnancy[3,11-13].
The etiology and mechanism of subserosal uterine vessel rupture are still not clear. The related high-risk factors may be the increased uterine blood supply during pregnancy. The pregnant uterus compresses the inferior vena cava and increases the pressure on the uterine vein. Shallow and thin vascular walls (without venous valve) of subserosal vein and para uterine vein would lead to rupture and bleeding with increased intra-abdominal pressure, as occurs with cough, defecation, and intercourse. The risk would be increased in the presence of uterine or vascular malformations[14]. In this article, the patient with posterior uterine wall vessel rupture suffered from uterine anomaly. Endometriosis is also a main high-risk factor for spontaneous rupture of uterine or pelvic vessels during pregnancy. The bleeding might be due to the spontaneous rupture of uterine ovary/pelvic vessels or bleeding from endometriotic implants[14-16]. The mechanisms of endometriosis leading to spontaneous rupture of uterine ovary/pelvic vessels may include chronic inflammation caused by endometriosis, which can increase the fragility of pelvic vessels or pelvic adhesions where the enlarging pregnancy pulls the pelvic blood vessels, thus leading to blood vessel rupture and subsequent bleeding[15]. A third mechanism may be invasion of the decidualized pelvic endometriosis lesions and penetration of the pelvic blood vessels causing bleeding. In a previous retrospective study, the sites of spontaneous vascular rupture were mostly located in the posterior wall of the uterus and the uterine tissue, and 52% of patients were accompanied by endometriosis[17]. In case 3, the ruptured branch of the external pelvic iliac vessel was associated with the extensive pelvic adhesions with concealed bleeding sites, which increased the difficulty of surgery and prolonged the time needed to find the bleeding site.
Rupture of parenchymal organs can be caused by trauma[18]. Spontaneous liver rupture is commonly seen in patients with severe preeclampsia and HELLP syndrome but can also be observed in women with normal pregnancy[1,19]. Our patient with spontaneous liver rupture (case 2) still had stable blood pressure during pregnancy, and there was no manifestation of preeclampsia or HELLP syndrome. During the operation, the liver showed obvious fat-like changes. However, there was no pathological examination result, and the specific etiology and mechanism were unclear. Spontaneous splenic rupture in pregnancy has been reported more often than spontaneous renal rupture. Spontaneous rupture of normal spleen during pregnancy may be caused by increased physiological circulating blood volume. An enlarged pregnant uterus would reduce the volume of the pelvic and abdominal cavity, increasing the spleen tissue fragility. In addition, the increased estrogen and progesterone levels during pregnancy represent high-risk factors for spleen rupture during pregnancy[20,21]. Therefore, spontaneous splenic rupture during pregnancy is more common in multiple pregnancies and late pregnancy. Pregnancy might be associated with pelvic and abdominal tumors. Under strict monitoring during pregnancy, changes in the tumor can be detected in time. Early intervention can effectively reduce the risk of spontaneous rupture of the tumor. In our case of renal hamartoma rupture (case 4), the renal tumor was undiagnosed before and during pregnancy.
Abdominal hemorrhage during pregnancy is characterized by acute abdomen syndrome[1]. Some patients might not have any instigating factor such as trauma and increased abdominal pressure. The accompanying symptoms may include nausea, vomiting, dizziness, fatigue, and anal bloating as well as hypovolemic shock in some severe cases. Signs on examination include varying degrees of tenderness, rebound pain and muscle tone, as well as shifting dullness. The site of the patient’s abdominal pain might be uncertain, often with lower or total abdominal pain. Therefore, the location of abdominal pain might not contribute to the identification of the bleeding site. If the kidney is ruptured, the bleeding is often limited to the retroperitoneum, and the patient’s pain would be limited to the kidney area with percussive pain, which would help identify the origin organ. Due to the increased blood volume during pregnancy, shock symptoms might not be obvious in the early stages. However, due to the redistribution of blood flow in various organs, uterine placental blood supply would be reduced, and fetal distress often occurs before maternal hemodynamic changes. Obstetric ultrasound would detect the fetal intrauterine condition and exclude the causes of uterine scar rupture, placental implantation, and placental abruption. Abdominal ultrasound can detect pelvic and abdominal tumors. However, for the spontaneous rupture of blood vessels or parenchymal organs, the bleeding site would be often unclear, which needs to be comprehensively analyzed, in combination with the patient’s risk factors.
In this study, ultrasound-guided abdominal puncture or culdocentesis were used as indications for laparotomy in three pregnant cases. Ultrasound-guided abdominal puncture or culdocentesis could contribute to a quick and clear diagnosis. More evidence and indications are needed for laparotomy, especially for pregnant women. However, when ultrasound examination at the bedside combined with the patient’s manifestations of hemoglobin decline and hemorrhagic shock suggest the diagnosis of intra-abdominal bleeding, an exploratory laparotomy can be immediately performed to gain time for rescue without puncture. Due to the low diagnostic value of the etiology and the potential for delaying the diagnosis, most patients do not need to undergo further computed tomography or magnetic resonance imaging examinations.
Intraperitoneal hemorrhage is an indication for emergency laparotomy. Once confirmed, regardless of the fetal condition, surgery should be performed at the same time as the anti-shock therapy, mainly to save the life of the pregnant woman. However, if the patient is identified early and rescued in time, the fetus could be salvaged. The longitudinal incision of the lower abdomen was our first choice in all our cases for better exposure. During the operation, a comprehensive pelvic and abdominal survey should be performed to find the bleeding site, and the incision could be extended to the upper abdomen if deemed necessary. According to the surgical experience of the cases reported herein, the bleeding site was often located at the place where the clot aggregated, which can help orient the surgeon to the site of bleeding.
Whether to perform cesarean section of the lower uterus at the same time during the operation needs to be considered based on whether the fetus is alive before surgery, gestational week, maternal condition, and intra-operative investigation. In case of intrauterine fetal death or previable pregnancy, the main purpose of the operation would be to stop the bleeding and the postoperative induction of labor. On the other hand, if the fetus is alive, pregnancy can be followed expectantly, and the delivery method should be evaluated when the fetus matures. There are reports concerning the cases of term or near-term natural delivery of subjects who were operated on in mid pregnancy[22,23]. If the bleeding site could not be identified due to obstructed view by the enlarged pregnant uterus, then delivery by cesarean section would be needed. If the fetus is mature or full term, a cesarean section should be performed at the same time with the operation. If the bleeding site can be identified immediately and the bleeding effectively stopped, a cesarean section should be performed first to rescue the fetus before hemodynamic instability from subsequent surgery that might cause deterioration in maternal and fetal conditions.
In summary, intra-abdominal hemorrhage during pregnancy is a rarely encountered dangerous complication, and obstetricians need to be vigilant in attempting to identify the source of bleeding specifically in pregnancies with high-risk factors, such as HELLP syndrome, endometriosis, and history of multiple abdominal surgeries. Early diagnosis, timely surgery, and multidisciplinary cooperation are the keys to maternal life and improving perinatal outcome.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tarazov PG, Usta IM S-Editor: Dou Y L-Editor: Filipodia E-Editor: Xing YX
| 1. | Ara I, Kundu MR, Islam S. Pregnancy induced hypertension caused spontaneous liver rupture. Mymensingh Med J. 2005;14:91-92. [PubMed] |
| 2. | Butorac D, Djaković I, Košec V, Kopjar M, Kuna K. Spontaneous Rupture of Internal Iliac Artery in Pregnancy: Case Report. Acta Clin Croat. 2018;57:157-160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Hamadeh S, Addas B, Hamadeh N, Rahman J. Spontaneous intraperitoneal hemorrhage in the third trimester of pregnancy: Clinical suspicion made the difference. J Obstet Gynaecol Res. 2018;44:161-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Hwang SS, Park YH, Lee CB, Jung YJ. Spontaneous rupture of hydronephrotic kidney during pregnancy: value of serial sonography. J Clin Ultrasound. 2000;28:358-360. [PubMed] [DOI] [Full Text] |
| 5. | Koifman A, Weintraub AY, Segal D. Idiopathic spontaneous hemoperitoneum during pregnancy. Arch Gynecol Obstet. 2007;276:269-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Maya ET, Srofenyoh EK, Buntugu KA, Lamptey M. Idiopathic spontaneous haemoperitoneum in the third trimester of pregnancy. Ghana Med J. 2012;46:258-260. [PubMed] |
| 7. | Wang C, Tu X, Li S, Luo G, Norwitz ER. Spontaneous rupture of the spleen: a rare but serious case of acute abdominal pain in pregnancy. J Emerg Med. 2011;41:503-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Low RK, Kogan BA, Stoller ML. Intraluminal wire retrieval of a proximally migrated pediatric Double-J ureteral stent. J Urol. 1995;154:223-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Doger E, Cakiroglu Y, Yildirim Kopuk S, Akar B, Caliskan E, Yucesoy G. Spontaneous rupture of uterine vein in twin pregnancy. Case Rep Obstet Gynecol. 2013;2013:596707. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Ginsburg KA, Valdes C, Schnider G. Spontaneous utero-ovarian vessel rupture during pregnancy: three case reports and a review of the literature. Obstet Gynecol. 1987;69:474-476. [PubMed] |
| 11. | Banaś T, Boryczko M, Durzyńska-Urbaniec J. Intraperitoneal hemorrhage due to the rupture of right ovarian artery in the second day of puerperium. Ginekol Pol. 2004;75:729-732. [PubMed] |
| 12. | Londero F, Cociancich G. Spontaneous rupture of the spleen in labor. Am J Obstet Gynecol. 2000;183:782-783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Sutton BC, Dunn ST, Landrum J, Mielke G. Fatal postpartum spontaneous liver rupture: case report and literature review. J Forensic Sci. 2008;53:472-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Naeh A, Bruchim I, Hallak M, Gabbay-Benziv R. Endometriosis-related Hemoperitoneum in Late Pregnancy. Isr Med Assoc J. 2019;21:557-559. [PubMed] |
| 15. | Cozzolino M, Corioni S, Maggio L, Sorbi F, Guaschino S, Fambrini M. Endometriosis-Related Hemoperitoneum in Pregnancy: A Diagnosis to Keep in Mind. Ochsner J. 2015;15:262-264. [PubMed] |
| 16. | Passos F, Calhaz-Jorge C, Graça LM. Endometriosis is a possible risk factor for spontaneous hemoperitoneum in the third trimester of pregnancy. Fertil Steril. 2008;89:251-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Brosens IA, Fusi L, Brosens JJ. Endometriosis is a risk factor for spontaneous hemoperitoneum during pregnancy. Fertil Steril. 2009;92:1243-1245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 77] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 18. | Icely S, Chez RA. Traumatic liver rupture in pregnancy. Am J Obstet Gynecol. 1999;180:1030-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Matsuda Y, Maeda T, Hatae M. Spontaneous rupture of the liver in an uncomplicated pregnancy. J Obstet Gynaecol Res. 1997;23:449-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Di Vella G, Arpaio A, Marzullo A, Colonna M. Rupture of the spleen or splenic vessels (splenic emergency syndrome) in late pregnancy: a report of two autopsy cases. Forensic Sci Int. 2008;176:e1-e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Maymon R, Zimerman AL, Strauss S, Gayer G. Maternal spleen size throughout normal pregnancy. Semin Ultrasound CT MR. 2007;28:64-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Roger N, Chitrit Y, Souhaid A, Rezig K, Saint-Leger S. Intraperitoneal hemorrhage from rupture of uterine varicose vein during pregnancy: case report and review of the literature. J Gynecol Obstet Biol Reprod (Paris). 2005;34:497-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | González Rosales R, Cerón Saldaña MA, Ayala Leal I, Cerda López JA. Uterine vessels spontaneous rupture during pregnancy: case report and literature review. Ginecol Obstet Mex. 2008;76:221-223. [PubMed] |