Published online Jul 6, 2020. doi: 10.12998/wjcc.v8.i13.2885
Peer-review started: February 2, 2020
First decision: May 21, 2020
Revised: May 23, 2020
Accepted: June 4, 2020
Article in press: June 4, 2020
Published online: July 6, 2020
Processing time: 155 Days and 12.4 Hours
Multiple intraoral dermoid cysts of large magnitude generally appear in the second or third decade of life. They are rare in infants and are usually solitary. In this case, a large mass was identified in utero during prenatal exams.
We introduce a rare case on multiple dermoid cysts in the floor of the mouth of an infant who underwent two surgeries for this. Preoperative magnetic resonance imaging confirmed a large well-circumscribed cystic lesion that originated at the former midline region in the floor of the mouth in which a suspicious lesion of minute size was likely compressed by the bulkier mass and overlooked. Therefore, the infant underwent two surgeries by an intraoral approach within 9 mo. At 5 mo after the second operation, a routine follow-up ultrasound showed evidence of an additional cyst. No further surgery was planned because the tumor had no immediate effect.
This report demonstrates the importance of carefully analyzing preoperative imaging to avoid multiple operations for a seemingly isolated oral cyst.
Core tip: Herein, we describe an infant subjected to surgery on two occasions for multiple dermoid cysts within the floor of the mouth and perform a systematic review of the literature. The multiple lesions were squeezed so much that they are ignored, which lead to two sequential surgeries.
- Citation: Liu NN, Zhang XY, Tang YY, Wang ZM. Two sequential surgeries in infant with multiple floor of the mouth dermoid cysts: A case report. World J Clin Cases 2020; 8(13): 2885-2892
- URL: https://www.wjgnet.com/2307-8960/full/v8/i13/2885.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i13.2885
Multiple dermoid cysts in the floor of mouth are atypical and rare. In head and neck locations, such growths are usually solitary and most often involve orbital regions[1]. They generally appear in the second or third decade of life, given the heightened degree of epithelial activity during this period. Although rare in infants, these cysts may develop at any age[2]. A majority are congenital, slow-growing and benign, attributable to mesenchymal entrapment of first and second branchial arch cells during weeks 3-4 of embryonic life. Their gradual enlargement may displace or elevate the tongue, causing dysphagia, dysphonia or even dyspnea[3]. Acquired cysts are secondarily inflicted via accidental or surgical implantation of epithelial cells[4].
Dermoid cysts are largely treated by surgical resection. The approach is dictated by location of tumor relative to mylohyoid muscle: intraoral (supramylohyoid) vs extraoral (inframylohyoid)[5]. Despite the cosmetic advantage of intraoral incisions, boosting its popularity, inherent anatomic complexities have hampered its standardization to date. The safety/efficacy of transoral excision also remains to be proven in this setting[6]. Herein, we report a rare instance of two surgical interventions in an infant with multiple dermoid cysts arising from the floor of the mouth.
A 1-mo-old female infant presented with a large swelling in the floor of the mouth followed by dysphagia since birth.
At week 24 of pregnancy, this lesion had been detected in utero (1.9 cm × 1.8 cm) during a routine prenatal examination. It further enlarged to 2.0 cm × 3.0 cm by week 34. Postnatally, there was visible upward displacement of the infant’s tongue by a mass that nearly filled the oral cavity, gradually interfering with swallowing and breathing. At 28 d of age, the newborn was referred to our hospital for treatment.
At admission, her medical history was otherwise unremarkable.
The patient had no personal or family history of other diseases.
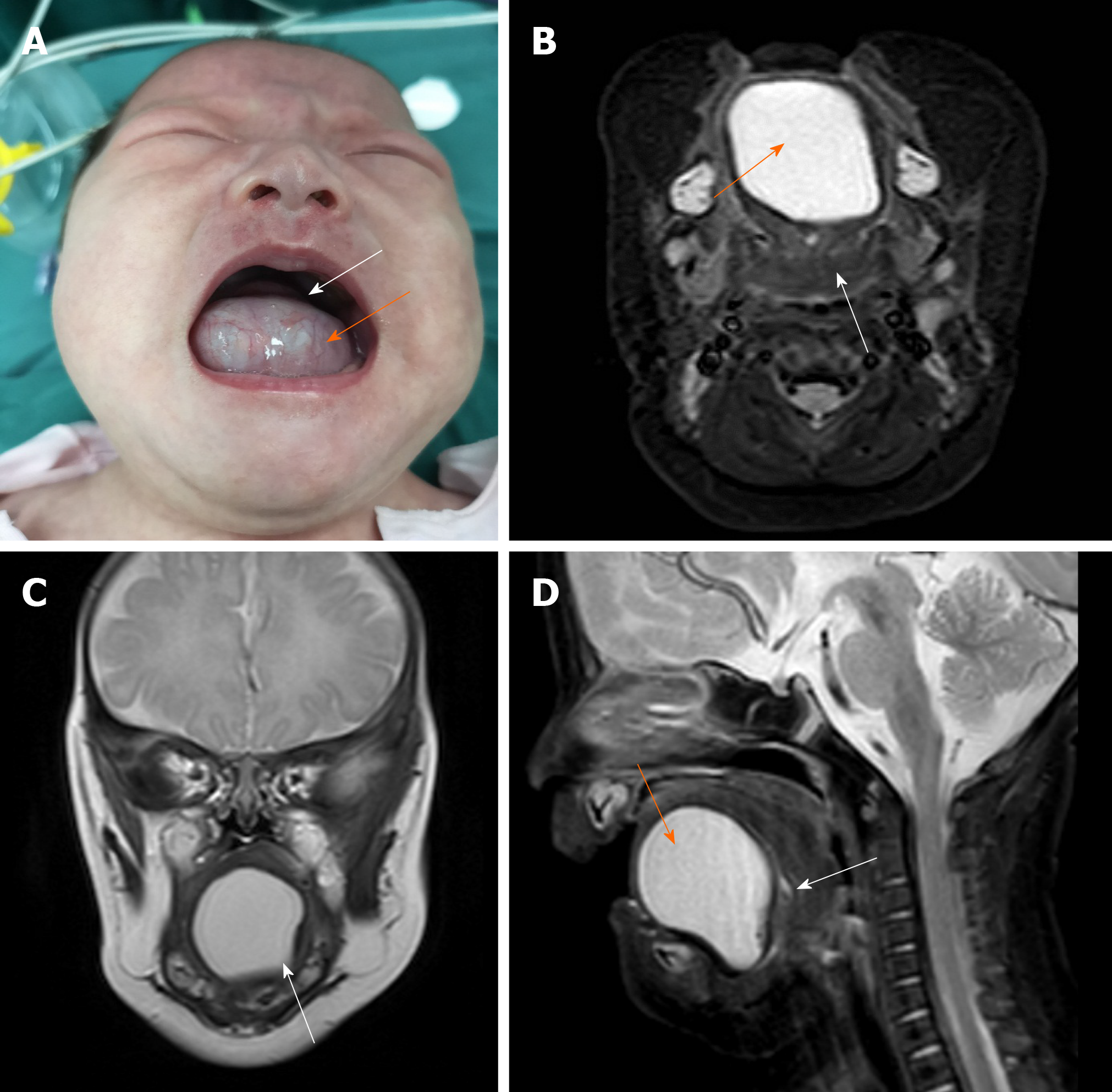
Physical examination revealed a large-sized cystic mass protruding from the floor of the mouth. Upon bimanual palpation, the soft and non-tender growth expanded to roughly 3.0 cm × 3.0 cm (Figure 1). Mouth closure was not feasible. The infant’s tongue was forced backwards and upwards in the oral cavity. The parents acknowledged swallowing difficulties but denied difficulty in breathing or signs of hypoxia during the previous month.
Laboratory results including complete blood count, electrolytes and coagulation panels were within normal limits with a white blood count of 7.8 × 109/L, red blood cell count of 4.0 × 1012/L and hemoglobin of 150 g/L.
Preoperative magnetic resonance imaging (MRI) confirmed a well-circumscribed cystic lesion (3.3 cm × 2.8 cm × 2.9 cm) of high signal intensity that originated at the former midline region in the floor of the mouth pushing the root of the tongue backwards (Figure 1).
The final diagnosis of the presented case is multiple dermoid cysts of the floor of the mouth.
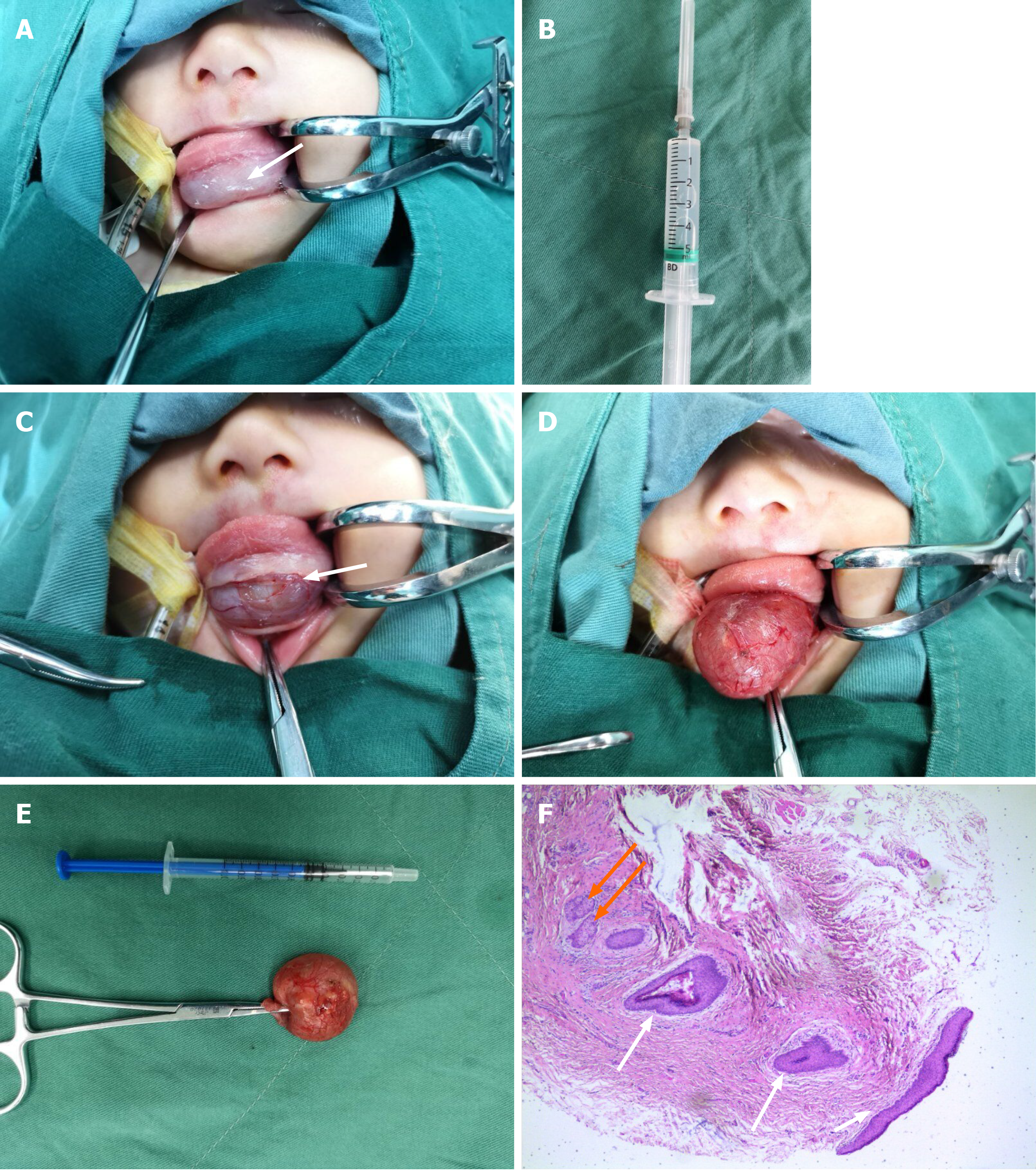
The infant was subjected to surgery on July 3, 2018. Given a predominantly supramylohyoid location, we elected an intraoral approach. However, the bulky cyst prevented direct oral intubation, calling for puncture (5 mL syringe) and withdrawal of clear fluid (about 10 mL). Oral intubation was smoothly executed thereafter (Figure 2), and general anesthesia was satisfactorily achieved. A horizontal incision was then made across the protuberance parallel to the dental arch above the caruncula and orifice of submandibular gland duct. The cyst was seated just beneath the mucous membrane. Its wall was dissected bluntly from surrounding tissues, carefully guarding submandibular gland duct, lingual nerve, hypoglossal nerve and other vital anatomic structures against injury. The resected lesion measured 2.0 cm × 2.0 cm (emptied of liquid content). It remained intact with some whitish keratin inside (Figure 2). To prevent postoperative complications (i.e. hemorrhage and floor of the mouth edema) that may cause upper respiratory tract obstruction, hemostasis was ensured, and drainage strips were placed before closing the incision. After surgery, patient monitoring was conducted in the pediatric intensive care unit.
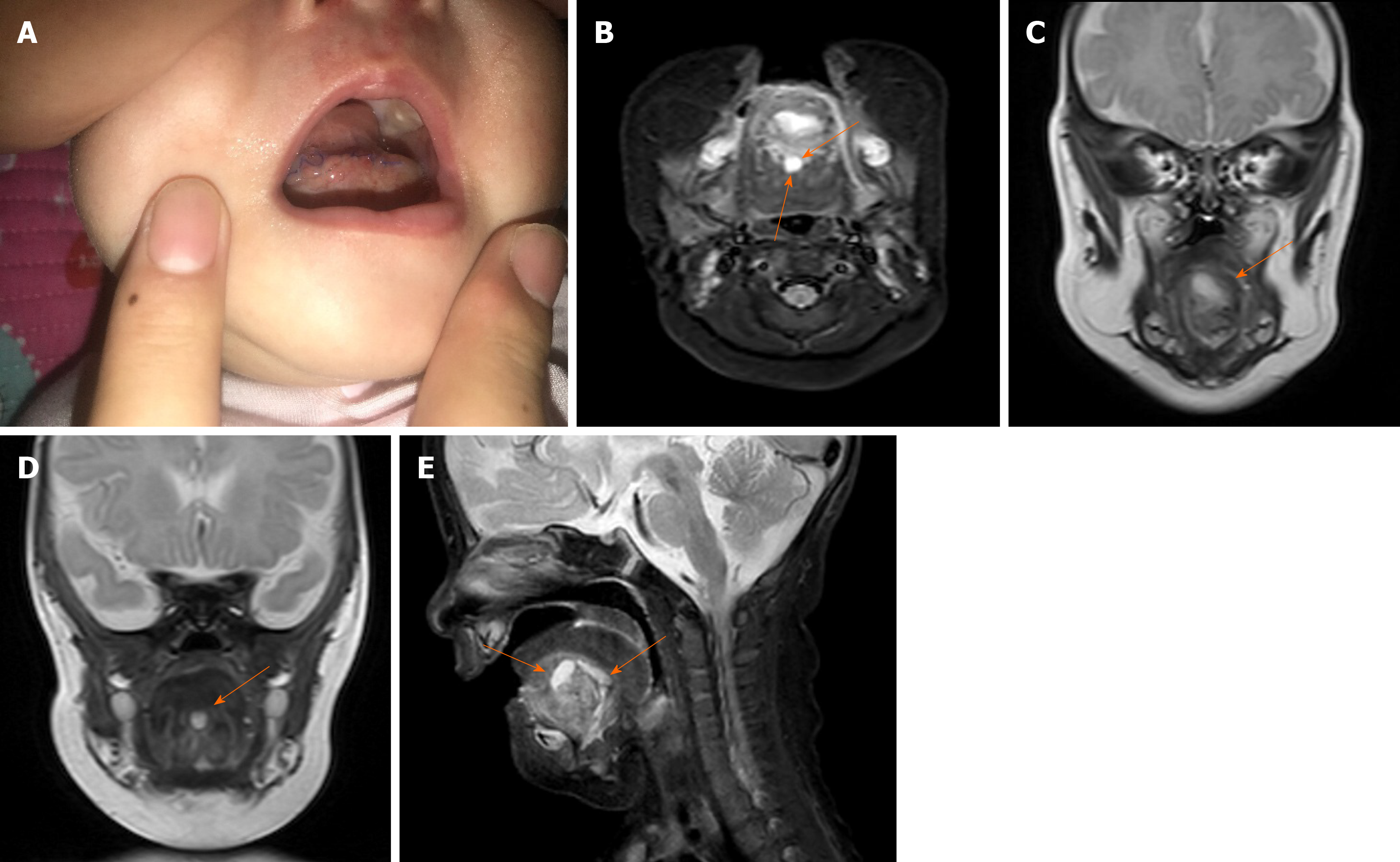
On postoperative day 2, the infant’s vital signs were stable, and there was no obvious hemorrhage or edema at the floor of the mouth, which allowed her to return to our ward. However, mild edema developed at the incision site on postoperative day 3 (Figure 3) and persisted, failing to subside appreciably after 3 d of dexamethasone treatment. An MRI study of the tongue obtained 1 wk later in follow-up showed two small cystic lesions beneath the tongue, approximately 0.8 cm × 1.0 cm × 0.5 cm and 1.2 cm × 0.5 cm × 0.5 cm (Figure 3). In reviewing the preoperative MRI, we identified a suspicious lesion of minute size (white arrow, Figures 1B and 1D), which was likely compressed by the bulkier mass and overlooked. Once the sizeable cyst was removed, the other rapidly enlarged. On postoperative day 9, the patient was discharged for further observation. Histologic sections revealed a keratinizing stratified squamous epithelial lining complete with sebaceous adnexa, confirming a dermoid cyst at the floor of the mouth (Figure 2).
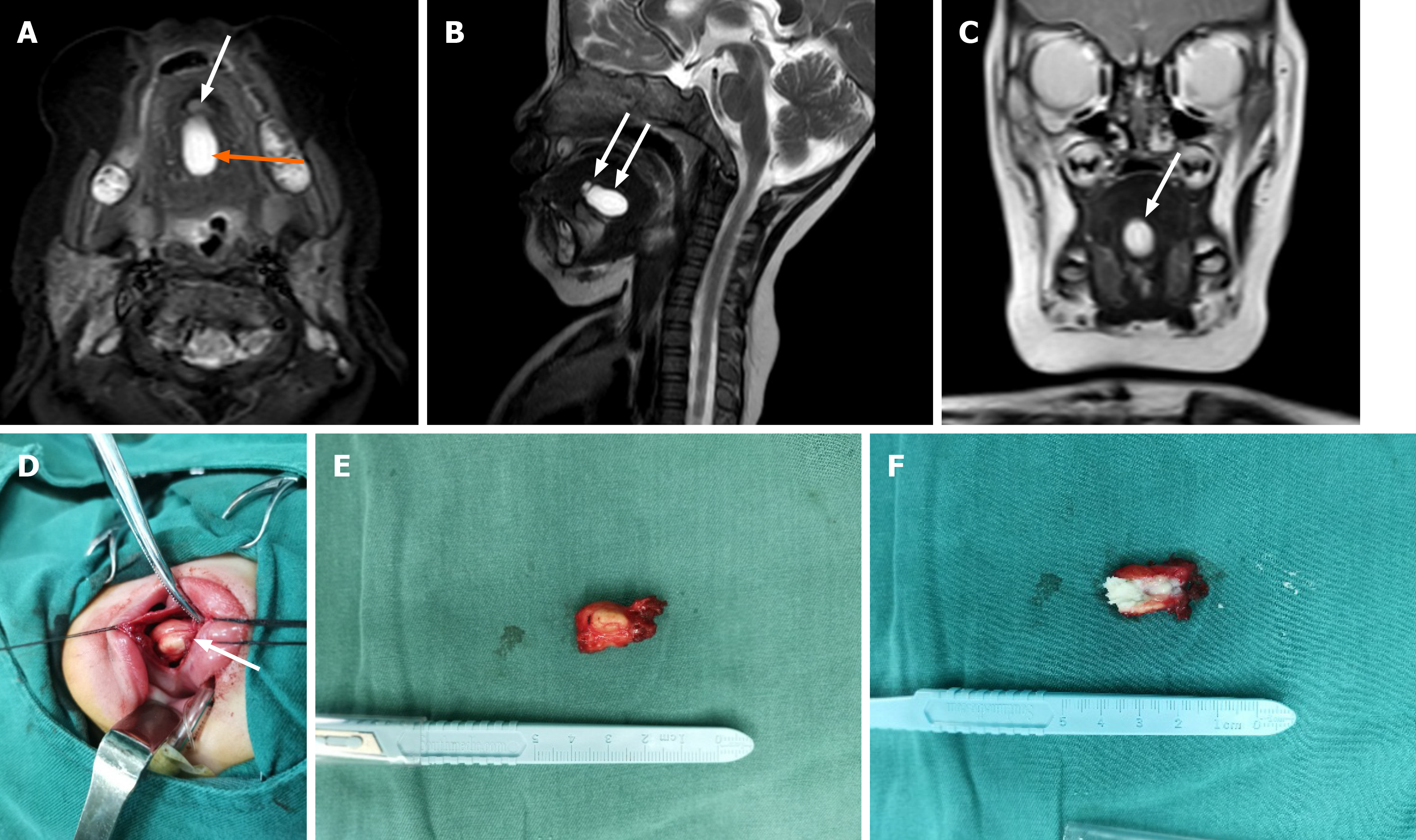
At 9 mo later, the parents and child revisited our department. Physical examination of the infant revealed a normal mouth opening with slight tongue elevation. A mass (2.0 cm × 2.0 cm) was palpable bimanually, present within the tongue muscle near the midline in the floor of the mouth. This lesion was less resilient with poor mobility. MRI in advance of a second surgery showed another lesion of high signal intensity (1.8 cm × 1.0 cm × 2.1 cm) present beneath the tongue muscle at midline (Figure 4). On February 14, 2019, surgery was again performed, reproducing the incision used earlier. A second cyst was found, deeply embedded in the mylohyoid muscle at the floor of the mouth requiring careful separation. We similarly withdrew some clear fluid to reduce its size. The fully excised lesion measured 1.5 cm × 1.0 cm including the capsule. Cross sections indicated that the content was sebum (Figure 4). The final pathologic diagnosis was also dermoid cyst.
At 5 mo after the second operation, the third cyst (1.5 cm × 0.9 cm × 1.0 cm) was found in the same location. However, this lesion had not impacted the child's eating, swallowing or breathing. Other than follow-up monitoring, no further operations have been planned.
There are three major theories at present to explain the origins of dermoid cysts[7]. The first (as in this infant) is a congenital basis. Indeed, this condition was initially detected during the mother’s routine prenatal examinations. At an early stage of embryonic development, the first and second branchial arches bilaterally join at midline. Epithelial remnants may become entrapped in doing so, or remnants of odd nodules forming the body of tongue and floor of mouth floor may persist giving rise to dermoid cysts[8]. The second theory accounts for acquired lesions, which are linked to traumatic or iatrogenic events or occlusion of a sebaceous gland duct[9]. The third theory is the rather remote possibility that such midline cervical growths represent cystic thyroglossal duct variants[7].
Dermoid cysts may occur in any region of the body, especially in the midline, where fusion of embryonic elements takes place. Ovarian and sacral regions are the most common locations for these growths, which seldom involve the head and neck (< 0.01%). On the other hand, the oral cavity and the lateral one-third of eyebrows are likely sites of head and neck development[10].
Cysts found at midline in the floor of the mouth are generally categorized in two ways. Based on histopathologic features, there is a spectrum of cystic teratomas, including epidermoid, dermoid and teratoid cysts, which are all closely related[11]. However, epidermoid and teratoid lesions are actually histologic variants of dermoid cysts[5]. The walls of true dermoid cysts are keratinizing and perhaps hair-bearing, harboring visible follicles and sebaceous or sweat glands, whereas epidermoid cysts have stratified squamous epithelial linings (usually cornified) devoid of cutaneous appendages. In both dermoid and epidermoid cysts, the content is typically a mix of keratin and oily sebaceous material. The walls of teratoid cysts and teratomas are often lined by stratified squamous and ciliated respiratory epithelia and incorporate a variety of ectodermal, endodermal and mesodermal elements[12]. This infant presented with true dermoid cysts, each having demonstrable sebaceous glands within the wall.
On an anatomic basis, midline cysts are classifiable as supramylohyoid, transmylohyoid (also known as perimylohyoid) and inframylohyoid, according to the topographic relation between cyst and muscle. The mylohyoid muscle separates sublingual spaces from submental and submandibular compartments[13]; supramylohyoid cysts may be further classified as above geniohyoid or between geniohyoid and mylohyoid[14]. The first cyst removed from this infant occurred at the supramylohyoid level, whereas the second was deep within the muscle itself. It is thus understandable that the small, compressed second and third cysts were so easily overlooked.
Imaging often plays an important role in surgical planning. In terms of soft tissue pathology, MRI is reportedly superior to other imaging modalities because there is good contrast between normal and diseased constituents, and no radiation exposure is entailed[15,16]. This is especially important in children, which prompted our use of MRI to delineate locations and magnitudes of cysts in this pediatric patient. Prior to the first surgery, the MRI study revealed a noticeable, bulky and well-defined cyst of hyperintense signal in T2-weighted phase, as well as a minute but suspect lesion of moderate signal intensity at the floor of the mouth (see white arrows, Figures 1B and 1D). Unfortunately, the more glaring findings on imaging sometimes overshadow other features or serve as distractions. We thus focused solely on the sizeable cyst, never suspecting that the minor lesion might be related or represent an independent threat. In resecting the large lesion, we felt that all adjacent tissues had been removed.
Faced with unanticipated postoperative edema, a follow-up MRI indicated two small, equal-sized cysts at the same surgical site. We then carefully reviewed the preoperative MRI, locating a tiny lesion (behind the large cyst) that was apparently left behind. A second preoperative MRI also showed two lesions, one large and one small. The small cyst sat in front of the large cyst, both closely aligned as possible arms of a single lesion. Had our resection been more thorough, such a recurrence may not have taken place. However, we found and resected one lesion only during the second surgery, encountering no other. At 5 mo later, a follow-up ultrasonic tomography confirmed the persistence of another small lesion. Consequently, it seems likely that the small cysts were compressed by the sizeable mass first resected, making it difficult to locate the other lesions in MRI studies or intraoperatively.
Nasotracheal intubation during the first operation and use of a tongue stitch for retraction during the second procedure proved helpful in our patient. These maneuvers generally provide clearer operative fields in the small mouths of pediatric patients[17]. The choice of surgical approach (intraoral vs extraoral) for tumors at the floor of the mouth is made individually, based on size and anatomic location of each lesion[18].
Surgical excision is an effective treatment for dermoid cysts[19], although care must be taken to limit trauma during procedures and ensure hemostasis at completion by placing drainage strips at that time. Intravenous dexamethasone injection may also relieve edema in the first 48 hours, and close observation of the respiratory tract is essential for 6-48 hours postoperatively. If swelling at the floor of the mouth is sudden and rapidly worsens, immediate operative exploration is mandatory to halt potential bleeding and prevent asphyxia.
Many authors have found marsupialization through transoral incision to be sufficient for large dermoid cysts, thus reducing operative time and minimizing damage to vital structures[20]. However, recurrence rates vary greatly when using this strategy. Marsupialization is in fact usually reserved for ranulas, which (unlike dermoid cysts) have no true epithelial linings[21].
Recurrence or malignant transformation (to squamous cell carcinoma) is exceedingly rare in this setting, and postoperative infections are unlikely[22]. Recurrent dermoid cysts are linked to cyst remnants on genial tubercle or hyoid bone, and malignant degeneration has only been reported in sporadic instances of teratoids[23]. The two recurrences herein to some extent reflect an inability to locate multiple lesions intraoperatively. It is worth considering whether a large dermoid cyst shares multiple lesions that may be compressed, warranting greater attention before and during surgery. Our patient will be followed regularly, checking for enlargement or signs of aggressive (i.e. malignant) behavior.
On the whole, dermoid cysts usually occur as a solitary mass. It is rare to find the condition identified during routine prenatal examinations like this case. Even more remarkable is the presence of multiple cysts in this infant’s floor of mouth. Unfortunately, the largest lesion compressed two smaller ones, making them difficult to locate by imaging or during surgery. Therefore, it is of great importance to analyze preoperative imaging carefully and to consider the potential for multiplicity in a seemingly isolated midline cyst of oral cavity.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Aydin M, Galiatsatos A S-Editor: Dou Y L-Editor: Filipodia E-Editor: Xing YX
| 1. | Voss JO, Buehling S, Thieme N, Doll C, Hauptmann K, Heiland M, Adolphs N, Raguse JD. Sublingual cysts of different entities in an infant - A case report and literature review. Int J Pediatr Otorhinolaryngol. 2018;113:260-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Ueno T, Takayama R, Osada SI, Saeki H. Epidermoid Cyst Arising on the Body of the Tongue: Case Report and Literature Review. J Nippon Med Sch. 2018;85:343-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Schwanke TW, Oomen KP, April MM, Ward RF, Modi VK. Floor of mouth masses in children: proposal of a new algorithm. Int J Pediatr Otorhinolaryngol. 2013;77:1489-1494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | MacNeil SD, Moxham JP. Review of floor of mouth dysontogenic cysts. Ann Otol Rhinol Laryngol. 2010;119:165-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | El-Hakim IE, Alyamani A. Alternative surgical approaches for excision of dermoid cyst of the floor of mouth. Int J Oral Maxillofac Surg. 2008;37:497-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Kim JP, Lee DK, Moon JH, Park JJ, Woo SH. Transoral Dermoid Cyst Excision: A Multicenter Prospective Observational Study. Otolaryngol Head Neck Surg. 2018;159:981-986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Dutta M, Saha J, Biswas G, Chattopadhyay S, Sen I, Sinha R. Epidermoid cysts in head and neck: our experiences, with review of literature. Indian J Otolaryngol Head Neck Surg. 2013;65:14-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Teszler CB, El-Naaj IA, Emodi O, Luntz M, Peled M. Dermoid cysts of the lateral floor of the mouth: A comprehensive anatomo-surgical classification of cysts of the oral floor. J Oral Maxillofac Surg. 2007;65:327-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Ramanathan M, Balasundharam S, Christabel A, Murali P, Pandem S. Simultaneous Occurrence of a Midline Sublingual Dermoid Cyst with Respiratory Epithelium and Submental Dermoid Cyst in a Paediatric Patient: A Case Report and Review of Literature. J Maxillofac Oral Surg. 2018;17:188-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Lenghel LM, Băciuţ G, Băciuţ M, Rotaru H, Bran S, Dinu C, Botar-Jid C, Gersak M, Dudea SM. The ultrasonographic diagnosis of cystic cervical lesions: a pictorial essay. Med Ultrason. 2016;18:240-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Lin HW, Silver AL, Cunnane ME, Sadow PM, Kieff DA. Lateral dermoid cyst of the floor of mouth: unusual radiologic and pathologic findings. Auris Nasus Larynx. 2011;38:650-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Kumar NG, Arora SS, Kumar I, Pandher PK, Balwan R. Dermoid Cysts of the Maxillofacial Region: Case Series. J Maxillofac Oral Surg. 2019;18:238-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Regis DM, Cunha JLS, Sánchez-Romero C, da Cruz Ramos MAC, de Albuquerque RLC, Bezerra BT. Diagnosis, management, and follow-up of extensive dermoid cyst of the submental region. Autops Case Rep. 2019;9:e2019095. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Kusuyama Y, Takeuchi N, Wakabayashi K, Yura Y. Dermoid Cyst of the Lateral Neck Included Within the Submandibular Gland. J Craniofac Surg. 2016;27:e33-e34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Edwards RM, Chapman T, Horn DL, Paladin AM, Iyer RS. Imaging of pediatric floor of mouth lesions. Pediatr Radiol. 2013;43:523-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 16. | La'porte SJ, Juttla JK, Lingam RK. Imaging the floor of the mouth and the sublingual space. Radiographics. 2011;31:1215-1230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 74] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 17. | Shashidhar A, Sadashiva N, Prabhuraj AR, Narasingha Rao K, Tiwari S, Saini J, Shukla D, Devi BI. Ruptured intracranial dermoid cysts: A retrospective institutional review. J Clin Neurosci. 2019;67:172-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Findik Y, Topal O, Senturk MF, Baykul T. Extraoral approach of the surgical treatment of sublingual epidermoid cyst: A case report. J Pak Med Assoc. 2017;67:796-798. [PubMed] |
| 19. | Hills SE, Maddalozzo J. Congenital lesions of epithelial origin. Otolaryngol Clin North Am. 2015;48:209-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Longo F, Maremonti P, Mangone GM, De Maria G, Califano L. Midline (dermoid) cysts of the floor of the mouth: report of 16 cases and review of surgical techniques. Plast Reconstr Surg. 2003;112:1560-1565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 97] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 21. | Puricelli E, Barreiro BOB, Quevedo AS, Ponzoni D. Occurrence of dermoid cyst in the floor of the mouth: the importance of differential diagnosis in pediatric patients. J Appl Oral Sci. 2017;25:341-345. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 22. | Dillon JR, Avillo AJ, Nelson BL. Dermoid Cyst of the Floor of the Mouth. Head Neck Pathol. 2015;9:376-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Zielinski R, Zakrzewska A. Submental epidermoid cysts in children. Open Med (Wars). 2015;10:77-81. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |