Published online Jul 6, 2020. doi: 10.12998/wjcc.v8.i13.2862
Peer-review started: January 17, 2020
First decision: March 27, 2020
Revised: May 24, 2020
Accepted: June 20, 2020
Article in press: June 20, 2020
Published online: July 6, 2020
Processing time: 171 Days and 20.3 Hours
Vascular injury is a rare complication of femoral shaft fractures, and rupture of the deep femoral artery is more difficult to diagnose because of its anatomical location and symptoms. Despite its low incidence, deep femoral artery rupture can lead to life-threatening outcomes, such as compartment syndrome, making early identification and diagnosis critical.
A 45-year-old male patient was admitted to our hospital due to right lower limb trauma in a car accident, with complaints of severe pain and swelling on his right thigh. X-ray demonstrated a right femoral shaft fracture. During preparation for emergency surgery, his blood pressure and blood oxygen saturation dropped, and sensorimotor function was lost. Computed tomography angiography was performed immediately to confirm the diagnosis of rupture of the deep femoral artery and compartment syndrome, so fasciotomy and vacuum-assisted closure were performed. Rhabdomyolysis took place after the operation and the patient was treated with appropriate electrolyte correction and diuretic therapy. Twenty days after the fasciotomy, treatment with the Hoffman Type II External Fixation System was planned, but it was unable to be immobilized internally based on a new esophageal cancer diagnosis. We kept the external fixation for 1 year, and 3 years of follow-up showed improvement of the patient’s overall conditions and muscle strength.
For patients with thigh swelling, pain, anemia, and unstable vital signs, anterior femoral artery injury should be highly suspected. Once diagnosed, surgical treatment should be performed immediately and complications of artery rupture must be suspected and addressed in time.
Core tip: We present a case of deep femoral artery injury in a patient with femoral fracture, which was very surprising considering the anatomical position of the deep artery, with the lower position of the femoral shaft fracture being compared to the hip fracture. In addition, for doctors, the possibility of diagnosing arterial rupture based on the non-specific symptoms of arterial rupture is much greater, which tends to cause a missed diagnosis. In addition, this case also introduces the treatment of life-threatening complications and feasible surgical techniques after arterial rupture.
- Citation: Ge J, Kong KY, Cheng XQ, Li P, Hu XX, Yang HL, Shen MJ. Missed diagnosis of femoral deep artery rupture after femoral shaft fracture: A case report. World J Clin Cases 2020; 8(13): 2862-2869
- URL: https://www.wjgnet.com/2307-8960/full/v8/i13/2862.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i13.2862
High-energy trauma is the most common reason for femoral shaft fracture. Vascular injury after femoral shaft fractures is a rare but life-threatening complication. Femoral artery injury occurs in 2% of patients with femoral shaft fractures[1]. Usually, patients experience symptoms such as low temperature in the lower limbs and no ankle pulsations[2]. Here, we present a case of a patient who suffered from atypical symptoms after closed femoral shaft fracture with femoral perforating artery rupture.
A 45-year-old male patient was admitted to our hospital due to right lower limb trauma in a car accident, complaining of severe pain and swelling on his right thigh.
His personal and family history contained nothing of note. There was no family history of related inherent diseases.
Severe pain and swelling were found on the patient’s right thigh. Peripheral circulation was in good condition, with both the femoral artery pulse and ankle pulsations detected. When preparing for surgery about 4 h after admission, the patient reported that the right ankle joint could not be twisted, and the right lower limb was numb, especially the lateral calf, top foot, and plantar numbness, but ankle pulsations could still be detected.
When preparing for emergency surgery about 4 h after the admission, the blood pressure and pulse oxygen of the patient sharply dropped to 83/58 mmHg and 70%, respectively.
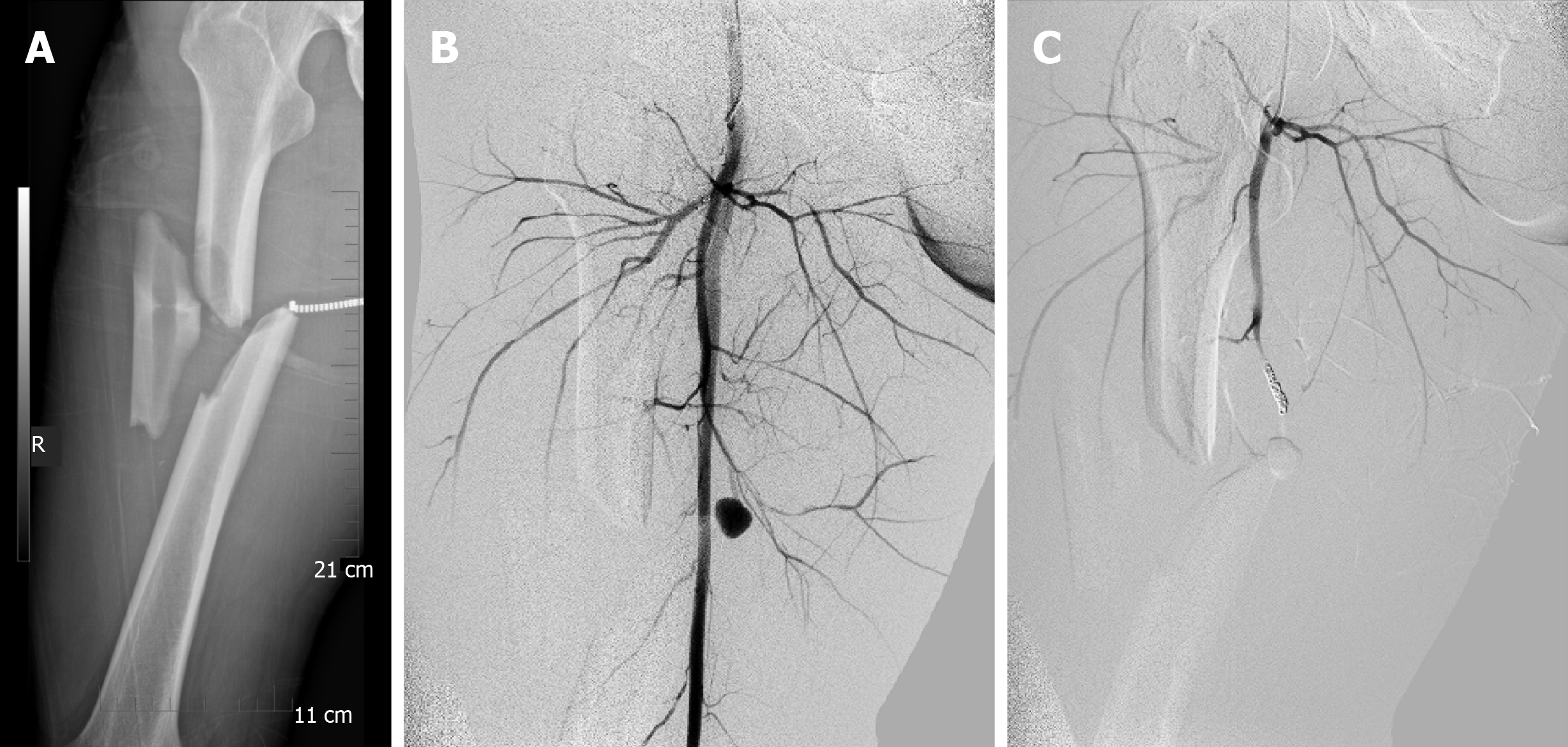
Upon admission, X-ray demonstrated a right femoral shaft fracture (Figure 1A). Upon the decrease in blood pressure and oxygen saturation, computed tomography angiography (referred to as CTA) was done immediately to confirm the diagnosis of deep femoral artery injury (Figure 1B). Contrast media accumulated at the femoral artery perforation, suggesting rupture of the blood vessel. The vessel was embodied at once by the interventional operation (Figure 1C).
The patient was finally diagnosed with femoral shaft fracture and injury of the deep femoral artery. Considering numbness and swelling, the patient also suffered from chamber syndrome, a complication of deep femoral artery rupture.
A fasciotomy between sartorius, rectus femoris, and vastus medialis was performed and vacuum-assisted closure was used for compartment syndrome.
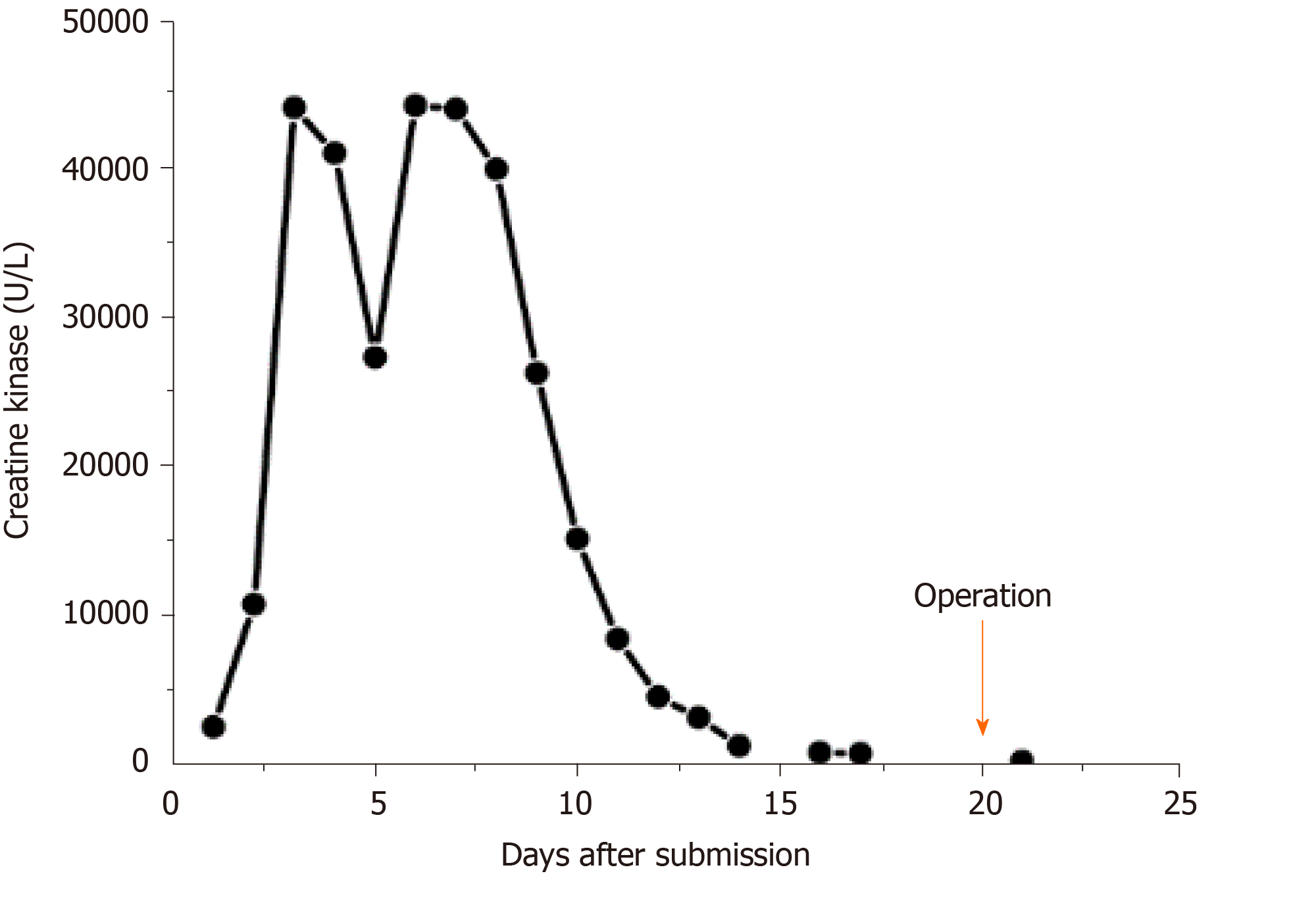
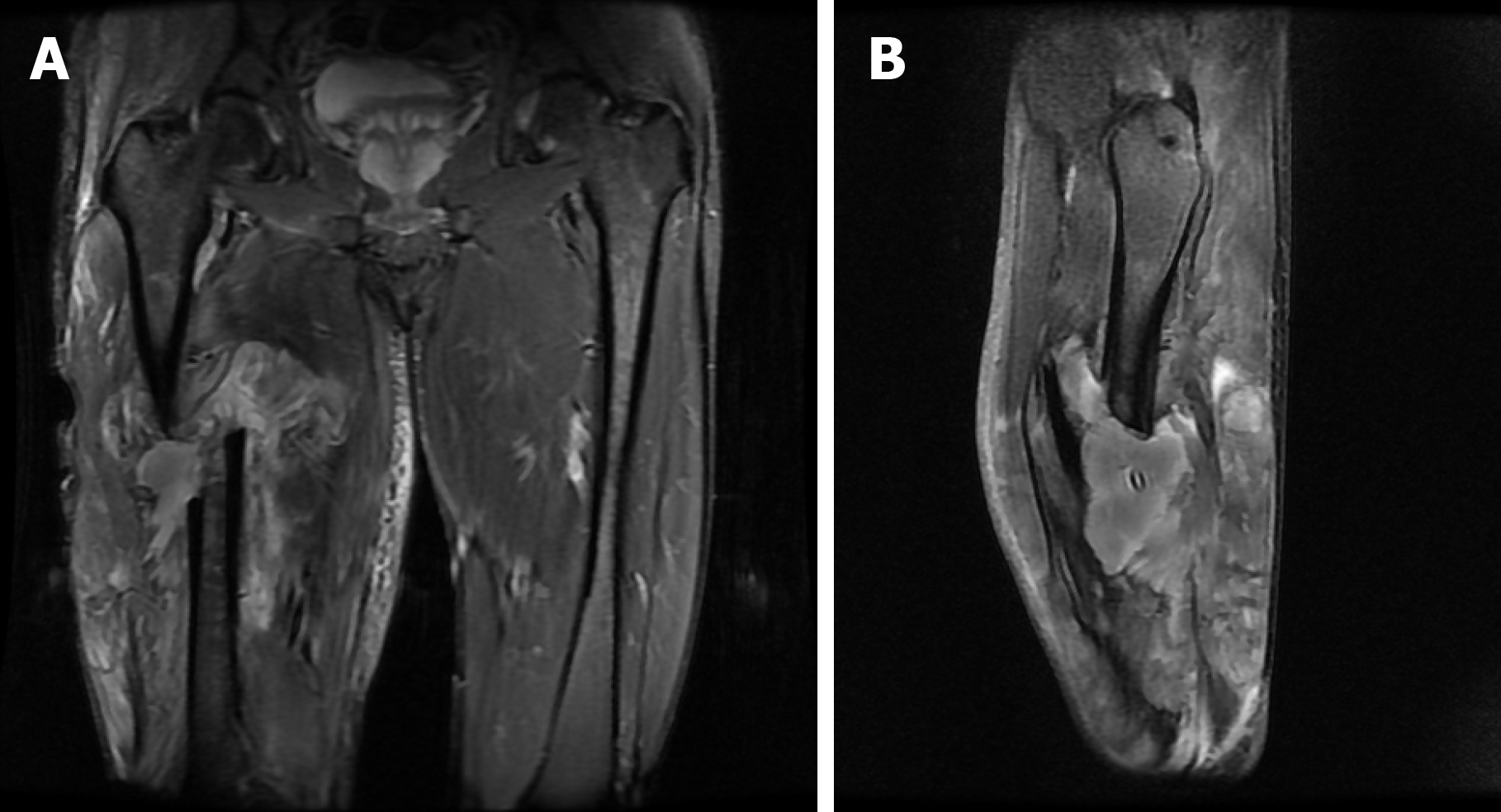
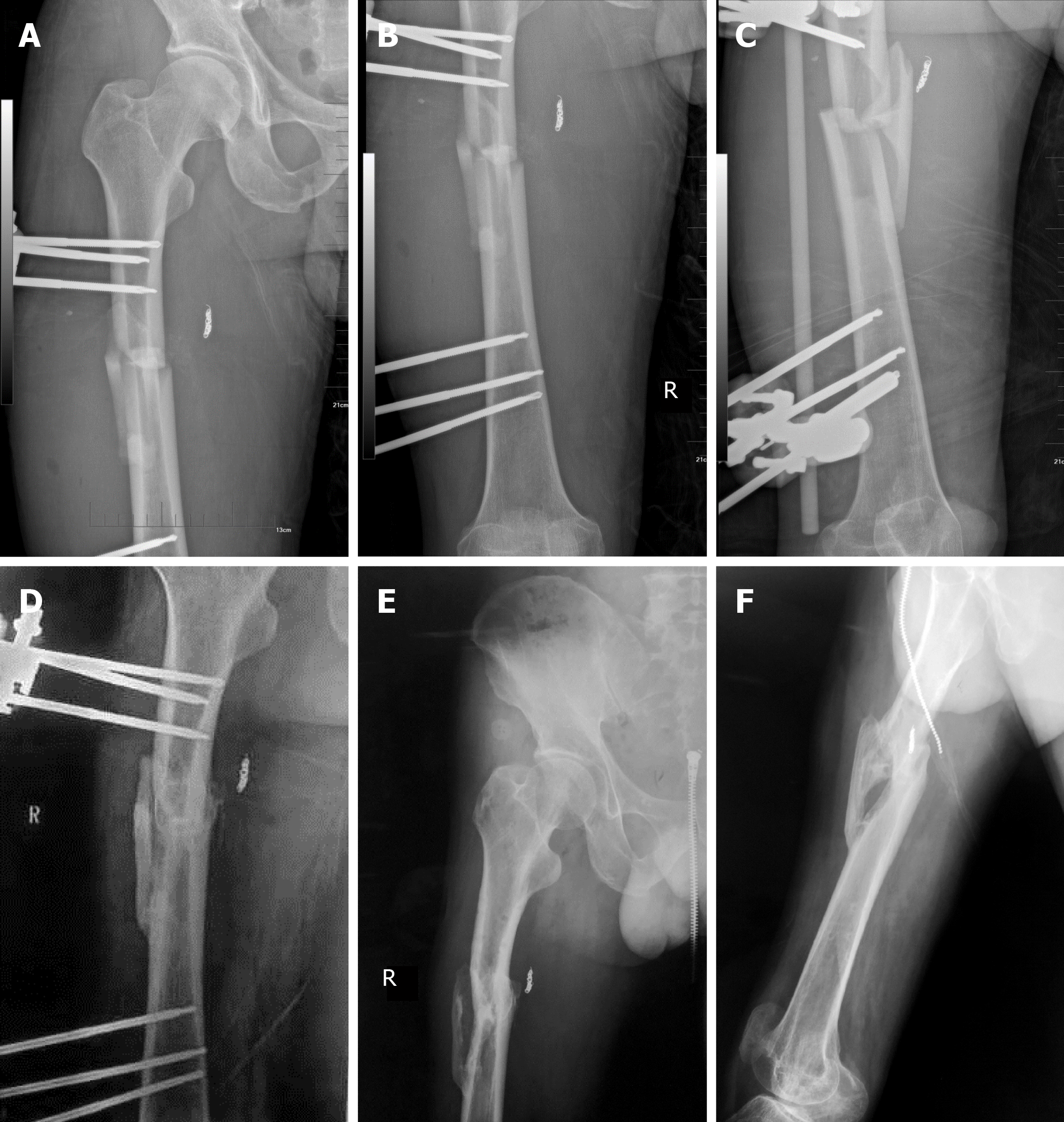
One day after the operation (day 3 in the hospital), there was a sharp decrease in the amount of urine output from the patient, with the color of the urine being dark tea-like in color. Furosemide was utilized and the symptom was relieved. Anemia was found in the patient. Two days after the operation (day 4 in the hospital), laboratory values revealed low hemoglobin (63 g/L), high aspartate amino transferase (1049.6 U/L), and high creatinine kinase (CK) (44205.2 U/L), indicating extensive muscle injury (Figure 2). Magnetic resonance imaging short TI reverse recovery sequences showed discontinuities in the right mid femoral shaft, dislocation of the stump, and swelling of the surrounding muscles (Figure 3A and 3B). Thus, the patient was definitely diagnosed with rhabdomyolysis. Hemodialysis treatment was not given due to the normal renal function. The patient was treated with the appropriate electrolyte correction, pH correction, and diuretic therapy. Laboratory tests were repeated daily. CK decreased from 44205.2 U/L to 26202.8 U/L on day 5 after admission, then rose again and gradually decreased to normal in the following days (Figure 2). Seven days after the operation, the right thigh was still swollen. Vacuum-assisted closure was removed after subcutaneous drainage. The condition improved after continuous subcutaneous drainage. The visual analogue score dropped from 8 to 4, with the swelling of the right thigh significantly reduced. Continuous traction of tibial nodules was offered. He was treated for a femoral fracture 20 d after the fasciotomy. A Hoffman II external fixator was offered (Stryker Trauma AG, Seizach, Switzerland; Figure 4A to 4C).
Originally, we intended to perform secondary internal fixation after external fixation. Unfortunately, after 1 wk of external fixation, the patient suddenly had difficulty swallowing. He was immediately transferred to the Thoracic Surgery Department and was diagnosed with esophageal cancer (poorly differentiated squamous cell carcinoma). The esophageal fistula made the patient miss the best time to replace the internal fixation 2 mo after the operation.
The 3-mo follow-up radiography showed that the callus had formed instead of the disappearing fracture line, indicating that the fracture had been healing. After careful consideration, we finally decided to keep the external fixator.
The 1-year follow-up of the patient at the local hospital showed that the fracture line had been blurred with mass formation of callus at the fracture site (Figure 4D). However, the function of the lower limbs of the patient had not fully recovered. The right quadriceps and biceps femoris muscle strength was grade III. While the muscle strength of right tibialis anterior, gastrocnemius, and extensor hallux are Grade 0. Electromyography showed the patient’s right tibial nerve, common peroneal nerve, superficial peroneal nerve, and sural nerve showed a negative reaction. Then the external fixation was removed. The 3-year-follow-up radiography revealed union of the fracture (Figure 4E and 4F). The patient's muscle strength has partially recovered. The strength of the right quadriceps and biceps femoris muscles is Grade 4. His right tibialis anterior, gastrocnemius, and extensor hallux muscle strength has improved to Grade 2. The patient is able to walk and is independent in self-care.
Blood supply to the femur is mostly provided by the femoral artery, branching into the deep femoral and the superficial femoral artery. Special attention should be paid to fractures at the junction of the middle and distal thirds of the femoral shaft, as the femoral artery in the adductor canal can be damaged[3]. The femoral artery is the main blood supply vessel of the lower extremity, and its damage is the most serious. The symptoms are more obvious than the branches and it is easy to diagnose. Rupture of the superficial femoral artery often causes bruising of the surrounding soft tissue and low skin temperature, so doctors find it easier to detect[4,5].
The deep femoral artery travels down the thigh close to the femur than the femoral artery, running between the pectineus and the adductor longus, and running on the posterior side of adductor longus. Because these muscles and tubular structures are surrounded, the deep femoral artery is not vulnerable. Due to these special anatomical structures, the rupture of femoral deep artery usually comes with non-specific clinical features like pain, hematoma, swelling, fever and anemia[6]. These non-specific clinical features might not alert doctors of ruptured arteries, often leading to delayed diagnosis. Although the incidence of deep femoral arteries and their branches is extremely low, there have been reports of such iatrogenic injuries by physicians[7], secondary to artery aneurysm[8,9], or bone spikes in hip fracture, especially in intertrochanteric fracture[10-12]. The rupture is rarely caused by direct blunt trauma[13]. However, no cases about femoral shaft fracture and causing injury to the deep femoral artery and its branches have been reported.
Considering the anatomical position of the deep artery, and the lower position of the femoral shaft fracture compared to the hip fracture, the injury of the deep artery and its branches by femoral shaft fracture is very surprising. In previous reports, the superficial femoral artery rupture had little effect on the femoral artery, with peripheral pulsations being still detected, including the femoral, ankle, and dorsal femoral arteries[4]. Similarly, peripheral vascular pulses disappearance was never mentioned in the previous reports of rupture of the deep artery and its branches. It is difficult for doctors to initially consider arterial rupture, which can easily lead to missed diagnosis. The delayed diagnosis resulted in unsatisfying prognosis.
Perforating arteries are branches of the deep artery, which are located deeper and are more difficult to injure. Perforating arteries are closed to femoral shaft anatomically. Recently, a three-dimensional reconstruction analysis based on CTA by Sun et al[14] showed that the mid-femoral level is the most dangerous level to damage the deep femoral artery and perforate the femoral artery. Thus surgeons should drill and screw insertion around the mid-shaft level for prevention of iatrogenic vascular injury. In addition, this study also revealed the possibility of vascular injury caused by femoral shaft fractures. Despite the low incidence in perforating artery rupture, as the direct supply for femur, the outcome of the rupture would be severe. And it is this artery that is damaged in this case. On the one hand, continuous bleeding can cause symptoms such as shock. On the other hand, bleeding can cause in situ massive hemorrhage[5] and pseudo-aneurysm formation[15]. Compression can have side effects. In addition, nonunion fractures are found due to insufficient blood supply[16].
About 1%-2% patients with femur fracture have compartment syndrome[3]. Despite the low incidence, about 44% of patients with acute compartment syndrome of the thigh suffer from persistent long-term functional deficits[17], and the mortality rate is as high as 47%[18]. Nervous system defects, infections, claudication, deep venous thrombosis, renal failure, and muscle necrosis are common complications of this rare disease. Among the complications, rhabdomyolysis and compartment syndrome complement each other[19]. Treatments for rhabdomyolysis focus on treating the cause, preventing renal failure, and managing life- or limb-threatening complications[20,21], while the potential mechanisms of compartment syndrome are vascular injuries[22-24]. The symptom is caused by the oppression of hematoma. Fasciotomy is a safe, effective, and economical treatment for fascial compartment syndrome. Although the choice of incision for fasciotomy is still controversial, the core principle of treatment is that all muscle chambers of the affected limb must be released[25]. For the etiological factor, since first described by Owers et al[26], transcatheter treatment has become the routine method for deep vascular injuries[22]. Early diagnosis and treatment of vascular involvement contribute to better functional outcomes[24]. Management of traumatic artery injury with direct artery repair greatly reduces the incidence of amputations. Considering the complex situation of the patient, in this case, we strictly followed the AO trauma management principles[27]. First, we performed fasciotomy for the compartment syndrome. Due to extensive soft tissue injury (extremely high CK and persistent swelling), we performed a secondary fracture reduction and fixation 20 d after fasciotomy. Although missed diagnosis affects the prognosis, timely treatment saves the patient from amputation. In the 3rd year after the operation, the patient was finally able to walk.
To treat femoral shaft fractures, there are three types of clinical surgical treatment: external fixation, titanium plate, and intramedullary nail. External fixation is not used as a conventional treatment for femoral shaft fractures, and it is generally used for multiple compound injuries of femoral shaft, as well as open infectious fractures[28]. Such injuries usually require timely and stable fixation. In this case, we performed external fixation for the patient to temporarily fix the femoral shaft fracture. After the condition was stable, we planned to replace the intramedullary nail. However, he was diagnosed with esophageal cancer after the external fixation surgery. The patient was immediately transferred to thoracic surgery department for operation. Unfortunately, postoperative esophageal fistulas occurred and we failed to replace the external fixation with intramedullary nails in a timely manner. Therefore, we finally decided to keep the external fixation.
First, we obtained satisfactory results in the X-ray examination after a 3-mo follow-up, that the poroma has formed instead of the disappearing fracture line, indicating that the fracture has been healing. Second, patients with long-term esophageal fistula could not tolerate further surgery. Third, patients were urged to receive chemotherapy and radiotherapy as soon as possible. Last but not the least, the right lower limb has lost most of its function due to the nerve damage. The right lower limb can only support his body. To summarize, we decided to retain the external fixation and follow-up regularly to ensure that the position of the external fixation does not shift. In the treatment of femoral shaft fractures, intramedullary nails are still the first choice for treatment, but external fixation still has its advantages. Compared with plate fixation, external fixation has less surgical trauma[29], especially less dissection of soft tissues such as muscle and vessels. Because of its unique advantages, intramedullary nails are the first choice. The central fixation of the intramedullary nail, with a high healing rate and a low infection rate, is better than the eccentric fixation of the plate. It contributes to increasing load on the poroma, bone healing and bone plasticity[30]. In this case, although the external fixation was not changed to intramedullary nail due to the incorrect timing, the fracture healing effect was good. A 3-year follow-up showed that in the long term, external fixation can heal fractures. The patient finally backs to walk. Considering the low muscle strength of the diseased limb, the healing condition of the fracture could meet the demand of the patient. Generally speaking, in the special cases, external fixation could be a surgical procedure choice for long-term fracture fixation.
The rupture of the deep femoral artery and its branches does not affect the peripheral circulation and is mainly manifested as non-specific symptoms. These characters might prevent physicians from thinking about the rupture of the blood vessels, leading to missed diagnosis. Missed diagnosis of the disease will cause severe complications. Peripheral circulation would be inaccurate in deep vascular injury. In the case of blunt trauma to the thigh, a decrease in blood pressure or sensory motor dysfunction should be noticed by the surgeon.
From the current case, we present some important guidelines based on our experiences. (1) Even for closed femoral shaft fractures, blood pressure and other vital signs of patients should always be closely monitored. (2) A thorough understanding of the femoral arterial route should be established for surgeons. If the direction of the femoral artery is lateral, attention should be paid to the rupture of the lateral femoral artery. While if the bone pike is medial oriented, rupture of the femoral artery and the deep artery is highly possible. If the barracuda is forward-looking, attention should be paid to the rupture of the deep arterial branch. (3) Injury of the prefemoral artery should be highly suspected when the injured side of the thigh is swollen, painful, anemic and with unstable vital signs. (4) Peripheral blood circulation signs cannot be used to diagnose the rupture of the prefemoral artery and its branches. CTA is the gold standard of diagnosis. And (5) Once the rupture of the artery is found, surgical treatment should be conducted as soon as possible. Decompression should be done as soon as possible to avoid complications such as compartment syndrome and rhabdomyolysis.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Vyshka G S-Editor: Liu M L-Editor: Filipodia E-Editor: Xing YX
| 1. | Barr H, Santer GJ, Stevenson IM. Occult femoral artery injury in relation to fracture of the femoral shaft. J Cardiovasc Surg (Torino). 1987;28:193-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 38] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Kirkup JR. Major arterial injury complicating fracture of the femoral shaft. J Bone Joint Surg Br. 1963;45-B:337-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Neumann MV, Südkamp NP, Strohm PC. Management of femoral shaft fractures. Acta Chir Orthop Traumatol Cech. 2015;82:22-32. [PubMed] |
| 4. | Siani A, Flaishman I, Napoli F, Schioppa A, Zaccaria A. Rupture of an isolated true superficial femoral artery aneurysm: case report. G Chir. 2005;26:215-217. [PubMed] [DOI] [Full Text] |
| 5. | Grimaldi M, Courvoisier A, Tonetti J, Vouaillat H, Merloz P. Superficial femoral artery injury resulting from intertrochanteric hip fracture fixation by a locked intramedullary nail. Orthop Traumatol Surg Res. 2009;95:380-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 6. | Tiwary SK, Kumar S, Khanna R, Khanna AK. Iatrogenic femoral artery aneurysms in orthopaedic practice. ANZ J Surg. 2007;77:899-901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Roy KD, Aggarwal RA, Purohit S, Bandagi G, Marathe N. Iatrogenic Pseudo-aneurysm of Profunda Femoris Artery Following Fixation of Intertrochanteric Femur Fracture - A Case Report and Review of Literature. J Clin Diagn Res. 2016;10:RD01-RD03. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (1)] |
| 8. | el Nakadi BE, Bertrand S, Farran M. Deep femoral artery aneurysm rupture. A case report. J Cardiovasc Surg (Torino). 1996;37:353-354. [PubMed] |
| 9. | Dulić G, Požgain Z, Pinotić K, Šego K, Selthofer R, Rončević I. Rare Case of Multiple Aneurysms with Rupture of the Deep Femoral Artery Aneurysm. Ann Vasc Surg. 2015;29:1663.e5-1663.e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Murphy PG, Geoghegan JG, Austin O, More-O'Ferrall R, Quinlan WR, Keaveny TV. Pseudoaneurysm of the profunda femoris artery due to intertrochanteric fracture of the hip. Arch Orthop Trauma Surg. 1999;119:117-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 36] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Dorrucci V, Spinamano L, Petralia G, Griselli F, Cibi N, Adornetto RJEE. Endovascular Repair of a Large Deep Femoral Artery Branch Pseudoaneurysm Following a Femur Fracture: A Case Report. EJVES. 2008;3:21-23. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Zhang BF, Cong YX, Wang PF, Huang H, Wang H, Zhuang Y. Deep femoral artery branch pseudoaneurysm formation and injury after hip fracture surgery: A case series and a literature review. Medicine (Baltimore). 2018;97:e9872. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Mueller DK, Greenberg JJ, Marshall WJ, Maull KI. Rupture of the deep femoral artery from blunt trauma. J Trauma. 1995;39:1010-1011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Sun Q, Fan G, Li X, Gong J, Ge W, Cai M. Relationship Between Femur and Femoral Arteries for Identifying Risk Factors for Vascular Injury. Med Sci Monit. 2017;23:1733-1740. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 15. | Sarwar CM, Riaz S, Lukhadwala RH. Postfixation pseudoaneurysm of the superficial femoral artery in femoral shaft fracture. J Coll Physicians Surg Pak. 2004;14:687-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Valli F, Teli MG, Innocenti M, Vercelli R, Prestamburgo D. Profunda femoris artery pseudoaneurysm following revision for femoral shaft fracture nonunion. World J Orthop. 2013;4:154-156. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Mithoefer K, Lhowe DW, Vrahas MS, Altman DT, Erens V, Altman GT. Functional outcome after acute compartment syndrome of the thigh. J Bone Joint Surg Am. 2006;88:729-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | Schwartz JT, Brumback RJ, Lakatos R, Poka A, Bathon GH, Burgess AR. Acute compartment syndrome of the thigh. A spectrum of injury. J Bone Joint Surg Am. 1989;71:392-400. [PubMed] |
| 19. | Parekh R, Care DA, Tainter CR. Rhabdomyolysis: advances in diagnosis and treatment. Emerg Med Pract. 2012;14:1-15; quiz 15. [PubMed] |
| 20. | Mouzopoulos G, Lasanianos N, Mouzopoulos D, Batanis G, Tzurbakis M, Georgilas I. Acute renal failure due to rhabdomyolysis after proximal humerus fracture associated with axillary artery rupture. Int Urol Nephrol. 2008;40:855-858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | Hammon K, Assael LA, Buchbinder D. Rhabdomyolysis in a patient with a mandibular fracture. J Oral Maxillofac Surg. 1987;45:627-630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 22. | Zuchelli D, Divaris N, McCormack JE, Huang EC, Chaudhary ND, Vosswinkel JA, Jawa RS. Extremity compartment syndrome following blunt trauma: a level I trauma center's 5-year experience. J Surg Res. 2017;217:131-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 23. | Ojike NI, Alla SR, Battista CT, Roberts CS. A single volar incision fasciotomy will decompress all three forearm compartments: a cadaver study. Injury. 2012;43:1949-1952. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Davaine JM, Lintz F, Cappelli M, Chaillou P, Gouin F, Patra P, Gouëffic Y. Acute compartment syndrome of the thigh secondary to isolated common femoral vessel injury: an unusual etiology. Ann Vasc Surg. 2013;27:802.e1-802.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Matsen FA, Winquist RA, Krugmire RB. Diagnosis and management of compartmental syndromes. J Bone Joint Surg Am. 1980;62:286-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 26. | Owers KL, Blewitt N, Morse MH. Arterial injury complicating femoral shaft fracture: control of primary and secondary profunda femoral bleeding by transcatheter embolisation. Injury. 1999;30:305-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 27. | Peter JL, Jebson. AO principles of fracture management. JAMA. 2018;20:2432-2433. [DOI] [Full Text] |
| 28. | Stojiljković P, Golubović Z, Mladenović D, Micić I, Karalejić S, Stojiljković D. [External skeletal fixation of femoral shaft fractures in polytrauma patients]. Med Pregl. 2008;61:497-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 29. | Testa G, Aloj D, Ghirri A, Petruccelli E, Pavone V, Massé A. Treatment of femoral shaft fractures with monoaxial external fixation in polytrauma patients. F1000Res. 2017;6:1333. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 30. | Paul MA, Patka P, van Heuzen EP, Koomen AR, Rauwerda J. Vascular injury from external fixation: case reports. J Trauma. 1992;33:917-920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 0.9] [Reference Citation Analysis (0)] |