Published online Jul 6, 2020. doi: 10.12998/wjcc.v8.i13.2855
Peer-review started: March 12, 2020
First decision: April 22, 2020
Revised: May 1, 2020
Accepted: June 18, 2020
Article in press: June 18, 2020
Published online: July 6, 2020
Processing time: 110 Days and 21.9 Hours
With the increasing trend of vaginal birth after caesarean delivery (VBAC), evaluation of the feasibility and safety of a second VBAC with grand multiparity is worth considering. Intrapartum uterine rupture is diagnosed in approximately one-fifth of all VBAC cases following successful vaginal delivery. To our knowledge, no report is available on the application of laparoscopy to repair postpartum uterine rupture after a successful second VBAC in China.
A 31-year-old woman (gravida 5, para 2) at 39 wk and 5 d of gestation was admitted to the hospital in labour. After a successful VBAC and observation for approximately 13 h, the patient complained of progressive abdominal pain. Given the symptoms, signs, and auxiliary examination results, intraperitoneal bleeding was considered. Because the patient was stable and ultrasound imaging was the only method available to assess the possibility of rupture, we recommended laparoscopy to clarify the diagnosis and for prompt laparoscopic uterine repair or exploratory laparotomy if necessary. Operative findings included transverse uterine scar rupture at the lower uterine segment of approximately 5.0 cm in length and 800 mL of intraoperative pelvic haemoperitoneum. Finally, she successfully underwent laparoscopic repair of uterine rupture and recovered very well according to three-dimensional magnetic resonance imaging at 42 d postpartum.
Routine postpartum intrauterine exploration is not beneficial to the mother and may even increase the risk of rupture. This case highlights a laparoscopic approach for repairing uterine rupture in the immediate postpartum period.
Core tip: With the advent of the two-child policy, the number of vaginal birth after caesarean delivery (VBAC) cases has markedly increased in China. Evaluation of the feasibility and safety of a second VBAC with grand multiparity is worth considering. In addition, if uterine rupture is identified after successful vaginal delivery but vital signs are stable, minimally invasive methods can be used to diagnose and repair uterine rupture. This case highlights a laparoscopic approach for repairing uterine rupture in the immediate postpartum period, and we hope that this technique will have an important clinical role in effectively reducing misdiagnoses of maternal injury and facilitating a quick recovery.
- Citation: Cai YQ, Liu W, Zhang H, He XQ, Zhang J. Laparoscopic repair of uterine rupture following successful second vaginal birth after caesarean delivery: A case report. World J Clin Cases 2020; 8(13): 2855-2861
- URL: https://www.wjgnet.com/2307-8960/full/v8/i13/2855.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i13.2855
Uterine rupture is a serious complication of pregnancy and directly threatens the lives and safety of pregnant women and their foetuses[1-3]. The primary causes of scar rupture include caesarean section, myomectomy, and hysterectomy[4]. According to prospective studies by Singh et al[5], the incidence of uterine rupture among women with a history of caesarean section is 1.69%, which is 11 times higher than that among women without a history of caesarean section. Because of the effects of China's family planning and two-child policies, the rate of vaginal birth after caesarean delivery (VBAC) in China increased by 14% between 2012 and 2016[6]. However, with the increasing trend of VBAC, evaluation of the feasibility and safety of a second VBAC with grand multiparity is worth considering but also challenging in terms of clinical treatment.
At present, many reports are available on risk factors and assessment methods for uterine rupture and the outcomes of the mother and child[7,8]. Many studies have explored the risk of intrauterine rupture as predicted by ultrasound measurements of scar thickness from previous intrauterine dissection, including the remaining myometrium thickness of the uterine scar, the continuity of the myometrium, the serosal surface, and even the changes in the myometrium during pregnancy[9,10]. However, scar thickness measurements in the lower uterine segment are affected by a variety of factors, including the measurement location, gestational age, and bladder filling degree. Therefore, no ideal scar thickness as a predictor of uterine rupture exists. Notably, women with caesarean scar diverticulum (CSD) have a weaker myometrium and a higher risk of uterine rupture in the third trimester than women without CSD, which has been widely accepted by researchers[11]. Uterine scar in CSD women pursuing another pregnancy should be assessed and managed. In a random population of women with a history of caesarean section, the prevalence of CSD ranged from 56% to 84% and 24% to 70% when assessed by transvaginal ultrasound (TVU) with and without contrast enhancement, respectively[12]. Thus, saline infusion sonohysterography and hysteroscopy are superior to conventional TVU for the assessment of uterine scar before pregnancy. If obvious menstrual abnormalities exist, the uterine diverticulum should be promptly repaired. Donnez et al[13] reported that if imaging examination indicates that the anterior wall muscle layer of the lower uterine segment is less than 3 mm, laparoscopic repair of the diverticulum should be performed to increase the thickness of the lower uterine segment.
Intrapartum uterine rupture is diagnosed in approximately one-fifth of all VBAC cases following successful vaginal delivery[14]. For the diagnosis and repair of uterine rupture, primary repair methods are performed by exploratory laparotomy, which undoubtedly increases maternal complications due to secondary trauma. Minimally invasive surgical methods are widely reported to be used to repair caesarean scar defects in women with abnormal menstrual manifestations. To our knowledge, no reports are available on the application of laparoscopy to repair postpartum uterine rupture after a successful second VBAC in China.
The patient experienced irregular uterine contractions for half a day.
A 31-year-old woman (gravida 5, para 2) at 39 wk and 5 d of gestation presented to the labour and delivery unit with spontaneous rupture of membranes. From 34 wk of pregnancy to regular prenatal examination in our hospital, the pregnancy was smooth. Measured in the third trimester, the thickness of the lower uterine muscle layer was 2.1 mm. Because the pregnant woman and her family insisted on vaginal delivery, we closely consulted vaginal delivery trials after informing the patient of her risk. Her labour was natural with epidural analgesia and without induction with Pitocin. The first and second stages of labour lasted 404 and 9 min, respectively, and the weight of the foetus was 3290 grams at birth. No classic signs of uterine rupture were noted at the time of delivery. The placenta was delivered spontaneously and intact. The level of postpartum haemorrhage totalled 140 mL, and no concern for uterine rupture or a retained placenta arose after routine postpartum intrauterine exploration. After observation for approximately 13 h, the patient complained of progressive abdominal pain.
The patient had a history of term caesarean delivery 6 years ago (2013) and successful VBAC 2 years ago (2017). The pregnancy was conceived naturally. No change in postpartum menstruation between the first and second deliveries was reported.
Physical examination showed total abdominal tenderness, positive rebound pain, migration dullness, and notably, tenderness in the lower segment of the uterus. The height of the uterus was one finger breadth under the navel, with a clear outline. All the other vital signs such as heart rate, blood pressure, respiratory rate, and temperature were stable.
Routine blood tests showed a 3-g/L decrease in haemoglobin (120 g/L) compared to that before delivery.
Detailed ultrasound imaging showed that the size of the uterus was 125 cm × 95 cm × 90 mm. A mixed-echoic region of 31 cm × 44 cm × 36 mm in size with an unclear boundary and no blood flow signals inside was observed in the lower uterine segment. However, the pelvic and abdominal cavities showed a large among of effusion, the hepatorenal fossae were 37 mm in length, and the left upper quadrant was 53 mm in length.
The final diagnosis of the case was “G5P3, 39 wk and 5 d of gestation, previous caesarean delivery, VBAC, and uterine rupture.”
Given the symptoms, signs, and auxiliary examination results, intraperitoneal bleeding was considered. Because the patient was stable and ultrasound imaging was the only method available to assess the possibility of rupture, we recommended laparoscopy to clarify the diagnosis and for prompt laparoscopic uterine repair or exploratory laparotomy if necessary. The surgery was performed approximately 15 h after delivery.
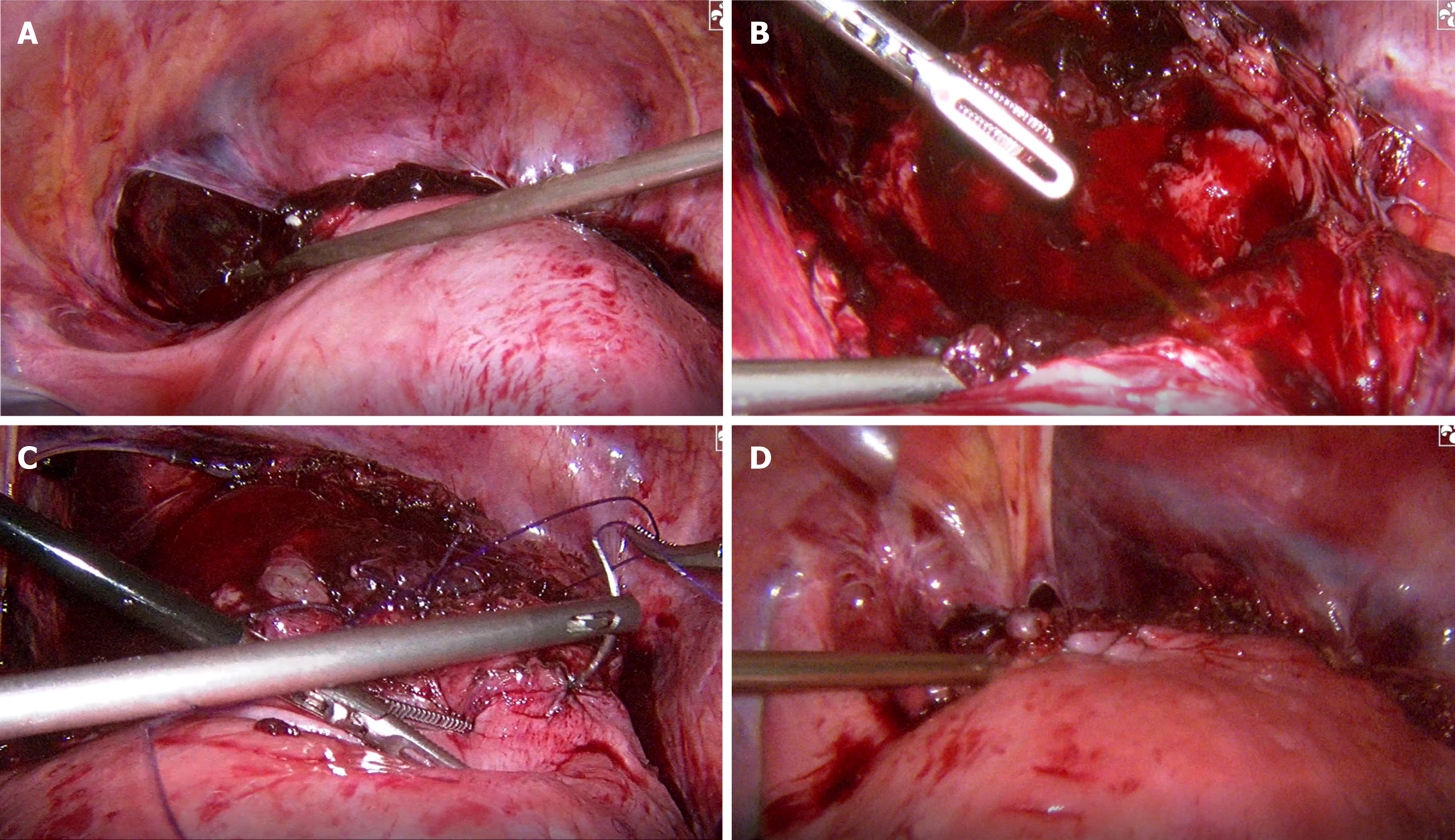
Operative findings included transverse uterine scar rupture in the lower uterine segment of approximately 5.0 cm in length and 800 mL of intraoperative pelvic haemoperitoneum. The ruptured tissue was fresh, and the incised edge was neatly aligned with the boundary of the bladder. The uterine defect was closed using a two-layer technique. The myometrium was completely closed with intermittent 1-0 intestinal sutures. The myometrium and serosal layers were closed with 2-0 Vicryl in a running fashion using an intracorporeal knot-tying technique. Finally, 1-0 Vicryl was used in a running fashion to close the serosal layers again and to interrupt the defect of the bladder peritoneum (Figure 1). The surgery was completed in 2 h, one indwelling abdominal drainage tube was in place postoperatively, and the estimated total blood loss was 1100 mL.
The patient’s postoperative body temperature was stable, the abdominal wound healed well, and she was cured and discharged on the sixth day after the operation.
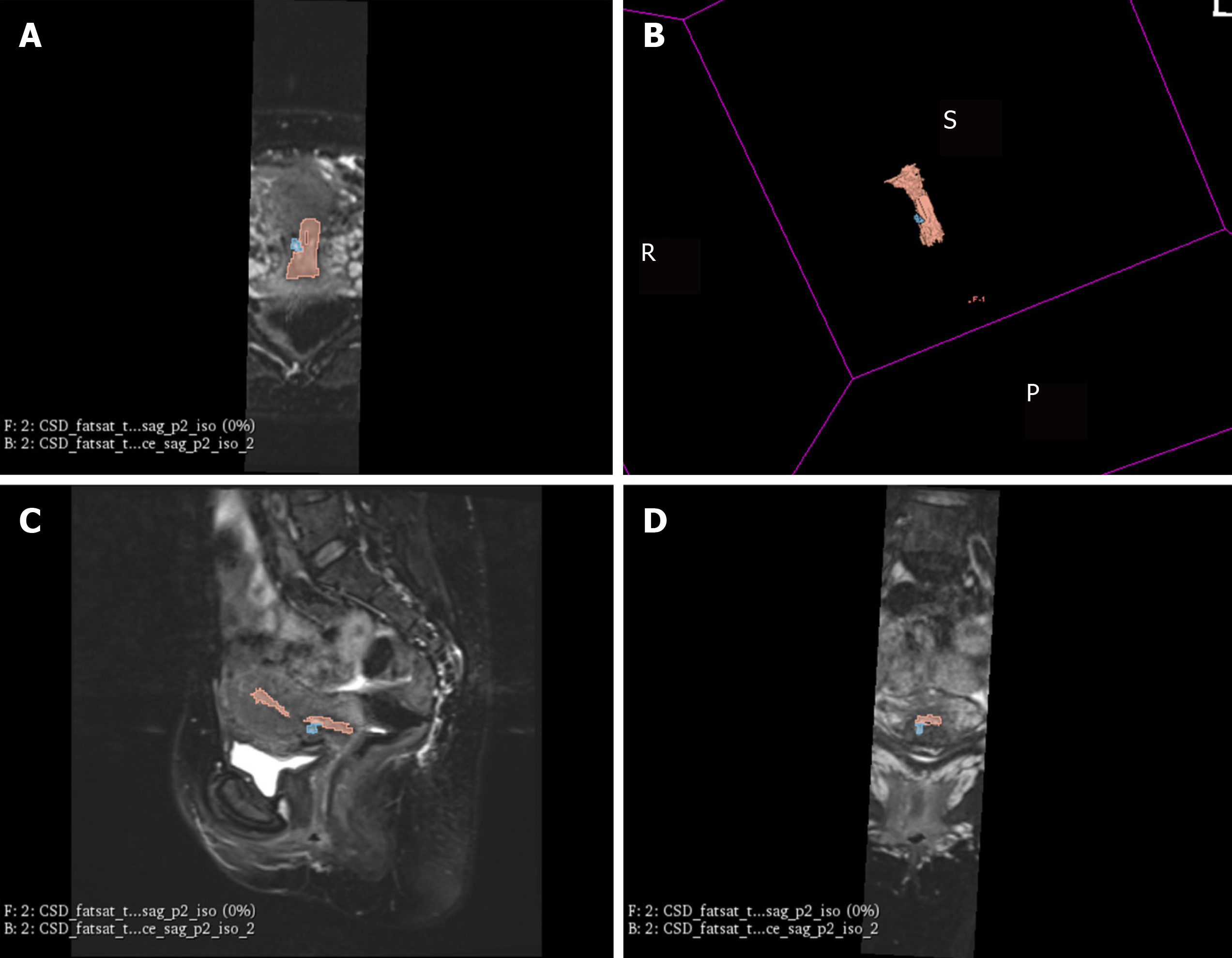
Postpartum follow-up showed that the lochia volume of the patient had decreased, and that postpartum bleeding lasted 25 d. Her routine examination at 42 d postpartum was normal. To understand the recovery of the lower uterine segment, we performed three-dimensional magnetic resonance imaging at 42 d postpartum. In the images, the signal of the muscle layer of the anterior wall of the uterus was uneven, and the high signal shadow penetrated into the muscle layer of the anterior wall of the uterus. The height, length, width, and remaining myometrial thickness of the diverticulum were 3 mm, 12.4 mm, 5.8 mm, and 4 mm, respectively (Figure 2).
Two of the most important factors influencing the success of VBAC are a previous vaginal delivery history and natural labour. According to the report by Guo et al[15], the success rate of VBAC was higher among women with no vaginal delivery history. However, multiple studies have also shown that among the risk factors for uterine rupture, grand multiparty is notably related to an increased risk of uterine rupture after VBAC[16]. Marie Bereka et al[17] demonstrated that uterine rupture was associated with obstructed labour, prolonged labour, malpresentation, and grand multiparity. The research by Ronel et al[18] showed that grand multiparity is an independent risk factor for uterine rupture (odds ratio [OR] = 1.2, 95% confidence interval [CI]: 1.1-1.3). In addition, Al-Zirqi et al[19] noted that compared to a parity of 1-2, parity ≥ 3 (adjusted OR = 2.8, 95%CI: 1.2-6.7) increased the risk of peripartum hysterectomy; that is, higher parity corresponds to lower muscle layer thickness in the lower uterine segment and a higher risk of rupture. Based on 5 years of VBAC case data collected at our hospital, we found that the percentage of successful VBAC cases with grand multiparity pregnancies (parity ≥ 3) was 6%, and 7/16 cases were second VBAC cases. The incidence rates of uterine rupture associated with the first VBAC and the second VBAC were 5.8% and 28.5%, respectively. Therefore, we speculate that the risk of uterine rupture with a second VBAC is definitively higher than that with the first VBAC. The reason may be weakness of the muscle layer of the inferior segment of the uterus after caesarean section and retraction of the myometrium with tissue oedema during vaginal birth for a second pregnancy. The feasibility and safety of a second VBAC require additional large-sample and multicentre studies for validation. Additionally, the patient should be fully informed of the increased risk of rupture during pregnancy and labour. Close monitoring and timely detection of uterine rupture are needed during the intrapartum and postpartum periods.
The diagnosis of uterine rupture is mainly based on clinical manifestations, foetal heart abnormalities, or imaging examinations. Some factors have been identified as independent risk factors for a delayed diagnosis, such as an unscarred uterus (OR = 27.0, 95%CI: 6.58-111.1), epidural analgesia during labour (OR = 7.9, 95%CI: 2.32-27.05), and grand multiparity (OR = 4.6, 95%CI: 1.40-14.99)[14]. The patient in our case report likely received epidural analgesia in her history of grand multiparty, which delayed the detection and diagnosis of uterine rupture. A previous study also showed that a delayed diagnosis was independently associated with hysterectomy and significantly higher rates of blood transfusions and puerperal fever. Clinically, manual exploration of the uterine cavity is commonly carried out after delivery to assess whether a laceration is present in the scar of the lower uterine segment and to observe urine volume and vaginal bleeding. However, the French College of Gynecologists and Obstetricians guidelines recommend that a simple uterine scar is not an indication for routine postpartum uterine cavity exploration, and that only symptomatic rupture requires surgical repair due to the low accuracy of postpartum exploration for diagnosing uterine rupture[20]. In contrast, no surgical treatment is required even if symptoms of suspected uterine rupture are noted on exploration. Additionally, according to Silberstein’s report, the detection rate of scar defects or scars detected by palpation after delivery is only 0.23%, and trauma can easily increase during the intrauterine exploration process[21]. Moreover, some case reports have described uterine rupture caused by postpartum uterine massage[22]. Therefore, routine postpartum intrauterine exploration is not beneficial to the mother and may even increase the risk of rupture. In this case, the patient underwent routine intrauterine exploration after delivery, and no obvious signs of rupture were detected. However, the typical symptom of abdominal pain in the patient appeared 13 h after delivery; therefore, the possibility of rupture caused by missed intrauterine exploration or improper postpartum massage cannot be excluded.
The treatment of uterine rupture mainly depends on the location of the rupture, the degree of involvement of the parauterine tissue, the desire for a subsequent pregnancy, and the willingness of patients and their families to make decisions. The treatment methods include uterine repair and hysterectomy. Exploratory laparotomy is the most commonly used method to confirm uterine rupture in clinical practice; however, laparoscopic uterine repair is rarely reported abroad. A case of postpartum uterine rupture and laparoscopic repair was reported by Rottenstreich et al[23]. Additionally, a special case of uterine and bladder rupture after VBAC and laparoscopic repair was reported by Lua et al[24]. With the continuous development of laparoscopic technology in recent years, its application has become increasingly extensive. The present case report shows that successful repair of uterine rupture can be achieved with a minimally invasive technique in the stable postpartum period. Since the patient had successfully delivered vaginally, no fresh scar was present on the abdomen, and her vital signs were stable. To determine the diagnosis, laparoscopy can be performed first, and then laparoscopic uterine repair can be carried out once the diagnosis is clear. The advantages of this approach include a small surgical wound and quick recovery, a clear diagnosis, fewer misdiagnoses of maternal injury, and the use of well-developed laparoscopic surgical technology. Thus, this approach should be applied more often in clinical practice.
The feasibility and safety of a second VBAC with grand multiparity require detailed clinical evaluations and additional study. Routine postpartum intrauterine exploration is not beneficial to the mother and may even increase the risk of rupture. This case highlights a laparoscopic approach for repairing uterine rupture in the immediate postpartum period.
We thank the woman who participated in the study. The authors thank Hong-Jie Pan for assistance with postpartum magnetic resonance imaging measurement and image acquisition.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Laganà AS S-Editor: Dou Y L-Editor: Wang TQ E-Editor: Xing YX
| 1. | Barger MK, Nannini A, DeJoy S, Wisner K, Markenson G. Maternal and newborn outcomes following uterine rupture among women without versus those with a prior cesarean. J Matern Fetal Neonatal Med. 2013;26:183-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Gibbins KJ, Weber T, Holmgren CM, Porter TF, Varner MW, Manuck TA. Maternal and fetal morbidity associated with uterine rupture of the unscarred uterus. Am J Obstet Gynecol. 2015;213:382.e1-382.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 74] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 3. | Al-Zirqi I, Daltveit AK, Vangen S. Infant outcome after complete uterine rupture. Am J Obstet Gynecol. 2018;219:109.e1-109.e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 4. | Smith JG, Mertz HL, Merrill DC. Identifying risk factors for uterine rupture. Clin Perinatol. 2008;35:85-99, viii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Singh A, Shrivastava C. Uterine Rupture: Still a Harsh Reality! J Obstet Gynaecol India. 2015;65:158-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Mu Y, Li X, Zhu J, Liu Z, Li M, Deng K, Deng C, Li Q, Kang L, Wang Y, Liang J. Prior caesarean section and likelihood of vaginal birth, 2012-2016, China. Bull World Health Organ. 2018;96:548-557. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 7. | Hidalgo-Lopezosa P, Hidalgo-Maestre M. [Risk of uterine rupture in vaginal birth after cesarean: Systematic review]. Enferm Clin. 2017;27:28-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Qu ZQ, Ma RM, Xiao H, Tian YQ, Li BL, Liang K, Du MY, Chen Z, Geng L, Yang MH, Tao YP, Zhu B. [The outcome of trial of labor after cesarean section]. Zhonghua Fu Chan Ke Za Zhi. 2016;51:748-753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 9. | Naji O, Wynants L, Smith A, Abdallah Y, Stalder C, Sayasneh A, McIndoe A, Ghaem-Maghami S, Van Huffel S, Van Calster B, Timmerman D, Bourne T. Predicting successful vaginal birth after Cesarean section using a model based on Cesarean scar features examined by transvaginal sonography. Ultrasound Obstet Gynecol. 2013;41:672-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 10. | Thapsamuthdechakorn A, Sekararithi R, Tongsong T. Factors Associated with Successful Trial of Labor after Cesarean Section: A Retrospective Cohort Study. J Pregnancy. 2018;2018:6140982. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 11. | Fukuda M, Fukuda K, Shimizu T, Bujold E. Ultrasound Assessment of Lower Uterine Segment Thickness During Pregnancy, Labour, and the Postpartum Period. J Obstet Gynaecol Can. 2016;38:134-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Bij de Vaate AJ, van der Voet LF, Naji O, Witmer M, Veersema S, Brölmann HA, Bourne T, Huirne JA. Prevalence, potential risk factors for development and symptoms related to the presence of uterine niches following Cesarean section: systematic review. Ultrasound Obstet Gynecol. 2014;43:372-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 234] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 13. | Donnez O, Donnez J, Orellana R, Dolmans MM. Gynecological and obstetrical outcomes after laparoscopic repair of a cesarean scar defect in a series of 38 women. Fertil Steril. 2017;107:289-296.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 125] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 14. | Rottenstreich M, Rotem R, Hirsch A, Farkash R, Rottenstreich A, Samueloff A, Sela HY. Delayed diagnosis of intrapartum uterine rupture - maternal and neonatal consequences. J Matern Fetal Neonatal Med. 2019;1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Guo N, Bai RM, Qu PF, Huang P, He YP, Wang CL, Mi Y. [Influencing factors and antenatal assessment of the vaginal birth after cesarean section]. Zhonghua Fu Chan Ke Za Zhi. 2019;54:369-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 16. | Wu Y, Kataria Y, Wang Z, Ming WK, Ellervik C. Factors associated with successful vaginal birth after a cesarean section: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2019;19:360. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 84] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 17. | Marie Bereka T, Mulat Aweke A, Eshetie Wondie T. Associated Factors and Outcome of Uterine Rupture at Suhul General Hospital, Shire Town, North West Tigray, Ethiopia 2016: A Case-Control Study. Obstet Gynecol Int. 2017;2017:8272786. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Ronel D, Wiznitzer A, Sergienko R, Zlotnik A, Sheiner E. Trends, risk factors and pregnancy outcome in women with uterine rupture. Arch Gynecol Obstet. 2012;285:317-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 64] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 19. | Al-Zirqi I, Daltveit AK, Vangen S. Maternal outcome after complete uterine rupture. Acta Obstet Gynecol Scand. 2019;98:1024-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 20. | Sentilhes L, Vayssière C, Beucher G, Deneux-Tharaux C, Deruelle P, Diemunsch P, Gallot D, Haumonté JB, Heimann S, Kayem G, Lopez E, Parant O, Schmitz T, Sellier Y, Rozenberg P, d'Ercole C. Delivery for women with a previous cesarean: guidelines for clinical practice from the French College of Gynecologists and Obstetricians (CNGOF). Eur J Obstet Gynecol Reprod Biol. 2013;170:25-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 128] [Article Influence: 10.7] [Reference Citation Analysis (1)] |
| 21. | Silberstein T, Wiznitzer A, Katz M, Friger M, Mazor M. Routine revision of uterine scar after cesarean section: has it ever been necessary? Eur J Obstet Gynecol Reprod Biol. 1998;78:29-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Ugboma HA, Akani CI. Abdominal massage: another cause of maternal mortality. Niger J Med. 2004;13:259-262. [PubMed] |
| 23. | Rottenstreich M, Khatib F, Sela HY, Grisaru-Granovsky S, Armon S. Laparoscopic repair of uterine rupture diagnosed in the early postpartum period. Eur J Obstet Gynecol Reprod Biol. 2019;240:379-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Lua LL, Evans T, Gomez N. Simultaneous Uterine and Bladder Rupture Following Successful Vaginal Birth After Cesarean Delivery: Laparoscopic Repair of Defect. J Minim Invasive Gynecol. 2017;24:329-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |