Published online Jul 6, 2020. doi: 10.12998/wjcc.v8.i13.2749
Peer-review started: March 2, 2020
First decision: April 22, 2020
Revised: May 14, 2020
Accepted: May 30, 2020
Article in press: May 30, 2020
Published online: July 6, 2020
Processing time: 126 Days and 5.1 Hours
Osteonecrosis of the femoral head (ONFH) is a destructive condition most commonly affecting young and middle-aged patients. The leading consequence of ONFH is often a significant articular disability. Effective joint-preserving surgical treatments are urgently needed for patients with early stage ONFH when outcomes of treatment are in general better than the advanced stage disease.
To introduce a new surgery procedure called percutaneous expanded core decompression and mixed bone graft technique, which is a new way of joint-preserving surgical treatments.
The clinical data of 6 patients with ONFH diagnosed and treated with the procedure called percutaneous expanded core decompression and mixed bone graft technique at The First Hospital of Qiqihar from March 2013 to August 2019 were retrospectively analyzed; the follow-up ended in December 2019.
There were 6 male patients with an average age of 43 years in our study. Gratifying results have been obtained from the comparison of Harris hip score, visual analogue scale, and imaging examination before and after operation.
This new modified technique is simple, safe, and reliable. No serious perioperative complications were observed in our cases. Advantages of the single blade expandable reamer are obvious. The adjuvant substance is inexpensive and easy to obtain. Thus, this technique is an effective joint-preserving surgical treatment for patients with early stage of ONFH.
Core tip: Percutaneous expanded core decompression and mixed bone graft technique is simple, safe, and reliable. In our cases no serious perioperative complications were observed. Advantages of the single blade expandable reamer are obvious. The adjuvant is inexpensive and easy to obtain. Thus, this technique is an effective joint-preserving surgical treatment for patients with early stage of osteonecrosis of the femoral head. It is easy to master as well as costs less. We present it here in the hope that colleagues in other institutions could try to use it and together to fully demonstrate its effectiveness.
- Citation: Lin L, Jiao Y, Luo XG, Zhang JZ, Yin HL, Ma L, Chen BR, Kelly DM, Gu WK, Chen H. Modified technique of advanced core decompression for treatment of femoral head osteonecrosis. World J Clin Cases 2020; 8(13): 2749-2757
- URL: https://www.wjgnet.com/2307-8960/full/v8/i13/2749.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i13.2749
Osteonecrosis of the femoral head (ONFH) is a destructive condition most commonly affecting young and middle-aged patients. ONFH often progresses to femoral head collapse, which in some cases can lead to total hip arthroplasty (THA)[1-4]. The treatment of ONFH has been studied extensively, and there are many options available for ONFH, including both nonsurgical treatment and surgical treatment. However, there is little supporting data on nonsurgical treatment when the condition is identified in the early stages. Activity modification with restricted weight bearing is often used for symptom relief but does not seem to alter disease progression[5,6]. Pharmacologic and biophysical treatments of ONFH consist of bisphosphonates, anticoagulants, vasodilators, statins, and biophysical modalities. The current state of nonsurgical treatment modalities for treatment of ONFH is still quite experimental in nature.
The most common surgical treatment is core decompression (with or without adjuvants) for early stage disease and THA. For patients with advanced stage of ONFH or failure of joint-preserving surgical treatments, THA is a better choice with excellent outcomes in terms of pain relief and survivorship[1,4,7]. Despite the excellent survivorship of THA, most patients with ONFH are young when they receive their THA, leaving them most likely to experience loosening and revision in their lifetime[8]. The ideal goal of early stage treatment is to postpone or stop the progression of the disease before femoral head collapse. Therefore, the most suitable time to intervene is the early stage of the disease before the mechanical failure of the subchondral bone and femoral head collapse, which belong to Association Research Circulation Osseous (ARCO) classification system stage I and II. A consensus has been reached on the following treatment modalities against the ONFH: Joint–preserving surgery for early stage and arthroplasty for later stage[9].
Core decompression is a joint-preserving surgical treatment that aims to improve blood flow and decrease intraosseous pressure for relieving pain. Its main goal is to promote early healing prior to collapse, thereby potentially postponing or avoiding THA[4,10]. But studies have shown that the femoral head after simple decompression may not provide structural support; as a result, the risk of femoral head collapse increases[11,12].
Bone grafting has been used to treat ONFH since the mid-twentieth century and is theorized to prevent femoral head collapse by providing structural support and establishing a stable environment for the growth of new bone[13]. Kong et al[14] studied the outcome of percutaneous core decompression with bone grafting on ONFH. They concluded that this method can be used to effectively treat the early stage of ONFH. This treatment modality can also significantly relieve symptoms, improve movement of hip, and postpone or stop femoral head collapse[14]. Zalavras et al[3] treated 17 hips in 15 patients with core decompression with autologous bone graft, and allogenic fibula perfused with human bone morphogenetic protein and noncollagenous proteins. Through a mean follow-up of 53 mo, 14 of 15 hips (93%) had relief of outcomes and no radiographic progression. Now the clinical outcome of core decompression with bone grafting on early stage of ONHF has been confirmed[3].
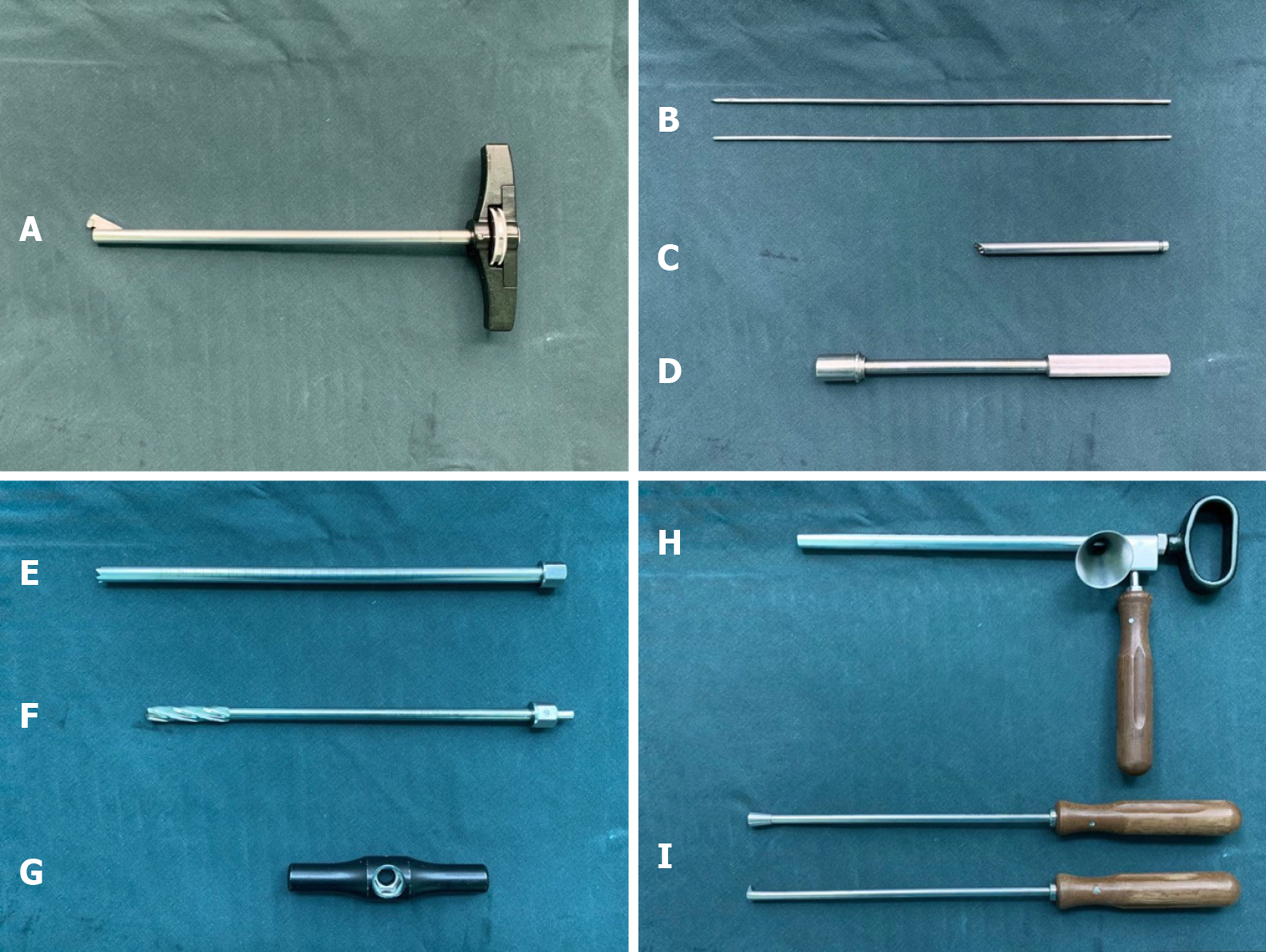
Advanced core decompression (ACD) is a relatively new technique using a percutaneous expandable reamer that allows more efficient removal of necrotic tissue from the femoral head[15-17]. Our new method is to use a single blade expandable reamer (Yierkang Technology Development Co., Ltd, Beijing, CHN) so that the lesion can be removed more precisely and thoroughly (Figure 1). Residual necrotic lesions are removed by cleaning with a sharp spoon. We use autologous bone from the ipsilateral ilium mixing allogeneic bone pieces with autologous bone marrow aspirate (BMA) and backfill the bone defects in the femoral head. We consider this is a good improvement of traditional surgical technique.
The aim of this article is to introduce a new modified surgical technique of ACD for early stage ONFH and demonstrate with one case from a group of patients treated with this method.
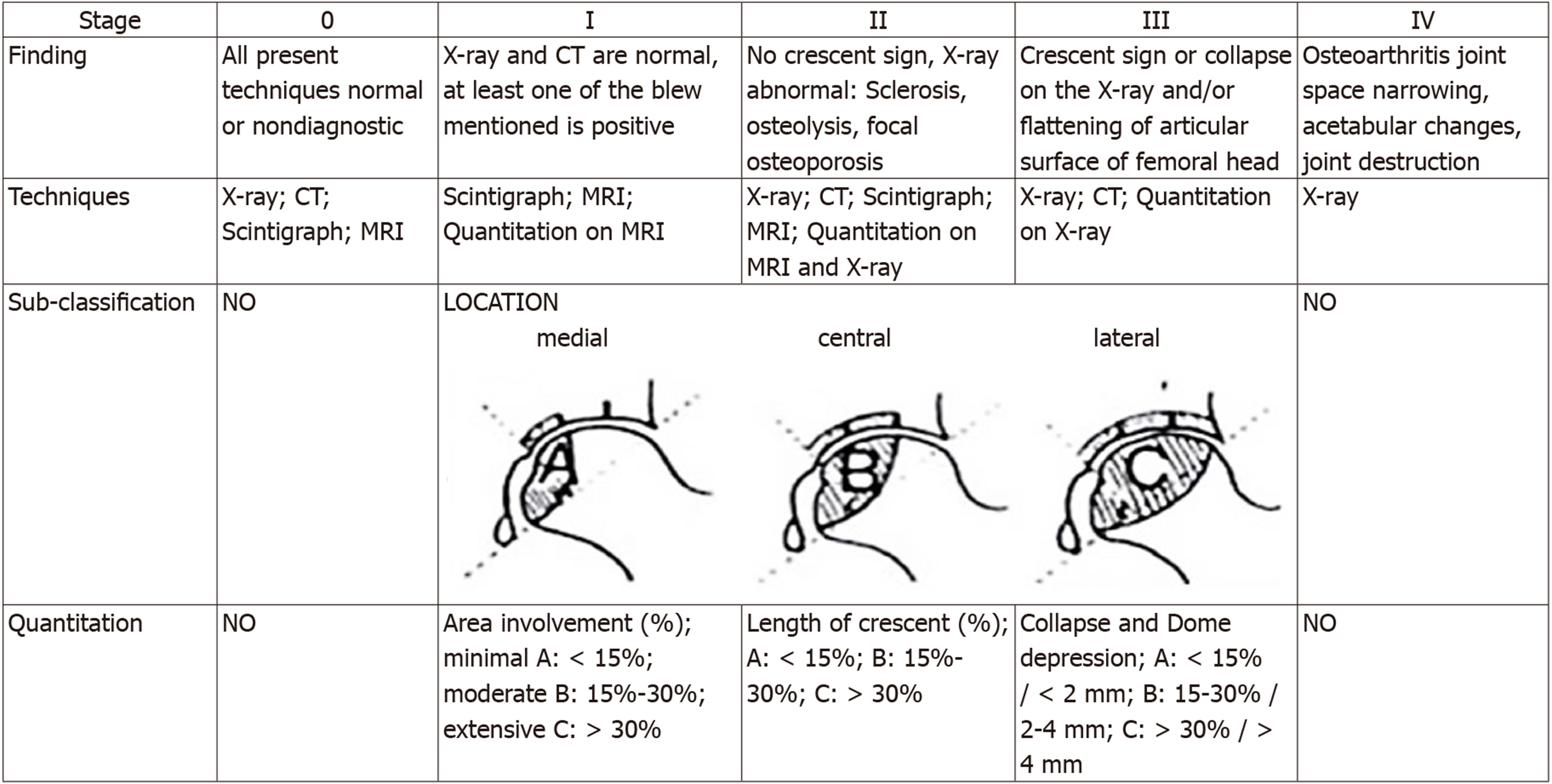
The patients for this treatment were chosen based on the 2012 Expert Consensus on the Diagnosis and Treatment Criteria for Adult Osteonecrosis of Femoral Head and belonged to the stage II of the ARCO classification system (Figure 2).
In addition, they needed to fulfill the following requirements: (1) The boundary of osteonecrosis in the femoral head was clear; (2) The patient’s age was under 60-years-old; and (3) Good hip range of motion in order to maintain the requirements of intraoperative position.
The outcome was evaluated by the Harris hip score (HHS), visual analogue scale (VAS), radiography, and computed tomography changes preoperative and postoperative.
Our new method is similar to the ACD procedure described by Landgraeber et al[17]. Improvements were made in expandable reamer and adjuvant substances.
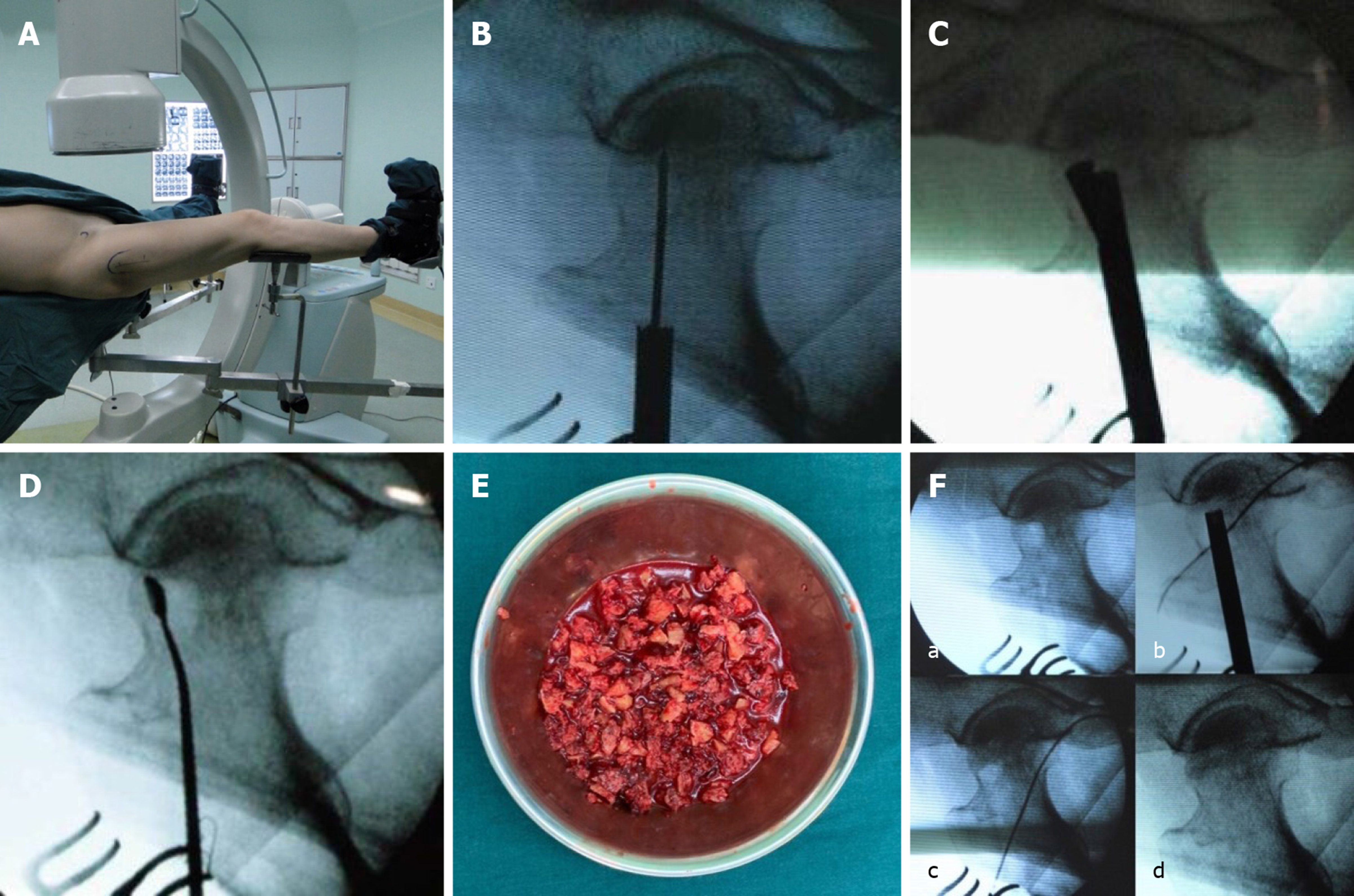
The surgery was performed with the patient lying flat on a trauma table and receiving continuous epidural anesthesia or general anesthesia (Figure 3A).
After the best entrance point for the drilling had been defined, a 2-3 cm skin incision at the distal end of the tuberculum innominatum was made. A 2.5 mm guide wire into the lesion area was introduced, then the introducer was placed (Figure 1C and D) along the guide wire and fixed on the lateral cortical bone of the femur. The design of this introducer made it easy and safe for the trephine to enter the bone. Then a 12 mm trephine into the lesion area under guidance of the introducer. To avoid deviation from the correct drilling, the trephine was guided by the introducer and the guide wire (Figure 3B). Then the introducer and the guide wire were removed, and a 10 mm trephine into the 12 mm trephine was drilled by turning the 10 mm trephine the cancellous bone in the femoral neck and a bone cylinder from the lateral cortical bone of femur. Afterwards, the drilling was completed with the 12 mm cannulated drill. These steps must be performed under C-arm fluoroscopy in both directions to make sure that the instruments were placed in the best possible position without damaging the cartilage or cortical bone.
The next step was different from the previous technique. A single blade expandable reamer into the drilling channel was introduced. By turning the handle and the blade control knob on it, the reamer can be rotated and the blades expanded under C-arm fluoroscopy to cut the necrotic lesion and dead bone as precisely as possible (Figure 3C). This instrument is different from the traditional expandable reamer in that its cutting plane is circular or fan-shaped by controlling the rotation angle. Therefore, its cutting range is more precise than traditional instruments, and the healthy bone can be retained to the maximum extent. After removal of the single blade expandable reamer, a sample of the necrotic lesion can be taken for pathological analysis to confirm the diagnosis. The residual lesions were removed by a sharp spoon (Figure 3D). Then the drilling channel and lesion area were flushed using a combination of irrigation and suction. These steps were important in order to remove the necrotic lesion and avoid postoperative infection. It should be repeated several times to achieve better results.
Finally, the lesion area and the surgical operation created bone defect were backfilled. This is another difference from the previous technique: We took the appropriate amount of cancellous bone and autologous BMA from the patient’s ipsilateral ilium. Both autologous bone and allogeneic bone was divided into small pieces and mixed. After adding the BMA, the mixture (Figure 3E) was introduced through a bone graft funnel (Figure 1H) into the lesion area, and the mixture was tamped by a pestle. Lastly, bone cylinder was used to backfill the lateral of femur (Figure 3F).
The incision was closed by the standard steps. After operation, patients were routinely given infection prevention and venous thromboembolism prevention. They were asked to come to the hospital for reexamination regularly, and they were put on weight-bearing restriction for 4 wk or their doctor’s recommendation.
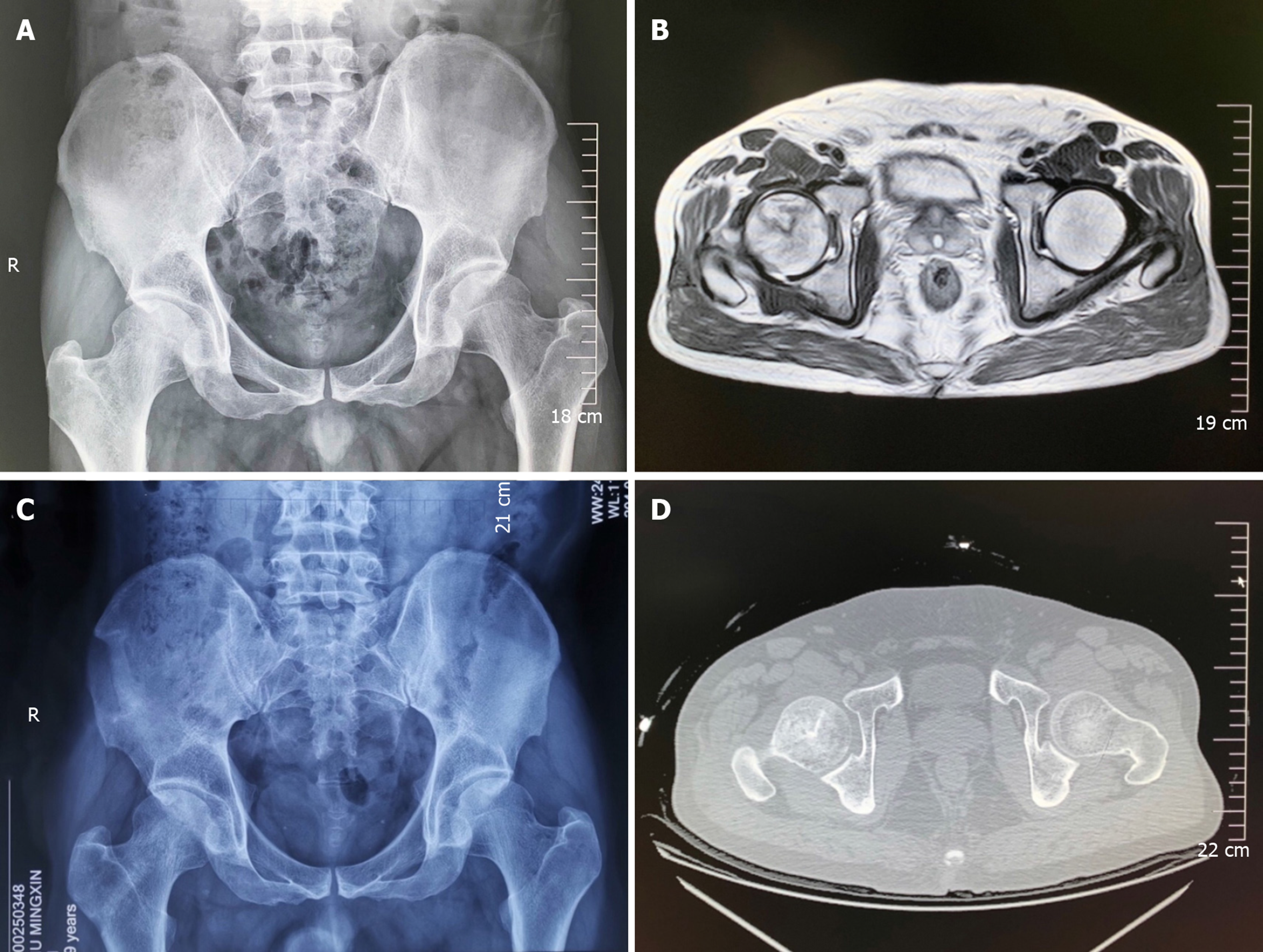
A 49-year-old male patient was diagnosed with nontraumatic osteonecrosis of the right femoral head and had a history of hypertension and smoking. The pain of the right hip joint was accompanied by limited movement for 2 mo. Magnetic resonance imaging showed the evidence of osteonecrosis of the right femoral head in stage II b of the ARCO system. The preoperative HHS was 68, and VAS was 6. We operated on him by the method described in this article. The surgical time was 50 min, and intraoperative bleeding was 100 mL. After operation, the patient was routinely given infection prevention and venous thromboembolism prevention. No complications occurred during the treatment. At 3 mo after surgery his HHS was 91, and VAS was 1. His right hip was almost free of discomfort. Radiography and computed tomography showed that the implanted bone was basically healed (Figure 4).
Since 2014, we have used this new modified technique in multiple patients, and gratifying results have been obtained from the comparison of HHS, VAS, and imaging examination before and after operation (Table 1).
| ID | Gender | Age | Diagnosis | Stage, ARCO | Date of surgery | Pre-op HHS/VAS | 3-mo HHS/VAS | Arthroplasty, 5 yr |
| 653075 | M | 48 | Non-traumatic ONFH (R) | II c | 3-12-2013 | 50/8 | 83/1 | No |
| 653711 | M | 50 | Non-traumatic ONFH (L) | II a | 3-13-2013 | 63/7 | 93/1 | No |
| 665314 | M | 27 | Non-traumatic ONFH (R) | II b | 3-24-2013 | 66/7 | 97/0 | No |
| 947454 | M | 46 | Non-traumatic ONFH (B) | R: II b; L: II b | 1-22-2016 | R: 71/6; L: 73/5 | R: 85/1; L: 86/1 | _ |
| 1265962 | M | 49 | Non-traumatic ONFH (R) | II b | 8-8-2019 | 68/6 | 91/1 | _ |
| 1270768 | M | 38 | Non-traumatic ONFH (R) | II b | 8-30-2019 | 63/7 | 83/1 | _ |
ONFH is due to osteocyte ischemia and necrosis, trabecular fracture, and femoral head collapse induced by a local blood circulation disorder of the femoral head because of various factors[3]. This disease is also a debilitating disease that leads to articular significant disability in young and middle-aged people. Without active and effective treatment, most of the patients need a THA after 2 years due to articular collapse[11,18]. Current consensus is that THA is used just for advanced-stage ONFH in older patients or those who have failed joint-preserving treatment[19]. Therefore, a definite and effective joint-preserving surgical treatment is urgently needed for young and middle-aged patients with early stage ONFH.
Core decompression combined with adjuvant substances as a joint-preserving surgical treatment has been widely recognized before[3,10,20-22]. In recent years, studies also showed that patients with ARCO classification system stage II treated by ACD in combination with autologous bone and BMA had good outcomes[23]. The usefulness of eliminating the necrotic bone and structural support by the adjuvant substances in the treatment of early ONFH has already been shown by other studies[3,16,24].
The differences between us and previous technologies are application of the single blade expandable reamer and a new bone grafting method. The single blade expandable reamer structure is simpler, and the safety and reliability are higher when it is used in operation. The design of the single blade can also make the core decompression more precise and thorough. More healthy bone can be retained than the previous expandable reamer. It is known that autologous bone graft has better biomechanical and biological properties than artificial bone graft and has all the requirements for good bone remodeling in terms of osteoconduction, osteoinduction, osteogenesis as well as osteointegration[25]. Autologous bone is precious and limited for every patient, so we mix allogeneic bone with it to increase the amount of bone graft. The biomechanical properties of allogeneic bone are similar to autologous bone. In China it is more cost effective than artificial bone. In addition, the mixture of autologous bone and allogeneic bone with BMA have better biological activity and are beneficial to the bone growth in the lesion area[18,21,25,26].
However, this new technique needs to be confirmed in more cases along with more detailed data comparison and further research. In the future, the research will also include age factors, Kerboul angle, and the size and location of lesions on the outcomes.
In conclusion, this new modified technique is simple, safe, and reliable. No serious perioperative complications were observed in our cases. Advantages of the single blade expandable reamer are obvious. The adjuvant substance is inexpensive and easy to obtain. Thus, this technique is an effective joint-preserving surgical treatment for patients with early stage ONFH. Although it's too early to come to a definitive conclusion, in our opinion this technique is easy to master as well as costs less. We present it here in the hope that colleagues in other institutions will try to use it and fully demonstrate its effectiveness.
Osteonecrosis of the femoral head (ONFH) is a terrible disease that usually affects young and middle-aged patients. The treatment of ONFH has been studied extensively. There are many options available for ONFH, including both nonsurgical treatment and surgical treatment. However, there is little supporting data on nonsurgical treatment when the condition is identified in the early stages. Most of the patients need a total hip arthroplasty after 2 years due to articular collapse. So effective joint-preserving surgical treatments are urgently needed for patients with early stage ONFH when outcomes of treatment are in general better than the advanced stage disease.
We would like to introduce a new technology that is safe, reliable, and effective in order for other doctors to adopt this new method for the joint-preserving treatment of ONFH.
Our study confirmed that percutaneous expanded core decompression and mixed bone graft technique is an effective joint-preserving surgical treatment for patients with early stage ONFH. It is easy to master and costs less than other methods. We want colleagues in other institutions to use it and also demonstrate its effectiveness.
From 2013 to 2019, we used percutaneous expanded core decompression and mixed bone graft technique to operate on a group of patients with ONFH. After the operation, the patients were routinely given infection prevention and venous thromboembolism prevention and asked to come to hospital for reexamination regularly while restricting weight-bearing movement for 4 wk. Through the application of a single blade expandable reamer, the core decompression can be precise and thorough. Following the decompression, the mixed bone graft is added. It consists of autologous bone, allogeneic bone, and bone marrow aspirate for a combination of biological activity and structural supporting. An excellent result was obtained by comparing Harris hip score, visual analogue scale, and imaging examination before and after operation.
All of the patients have achieved satisfactory results in our study from 2013 to 2019. After surgery their Harris hip score and visual analogue scale were improved. Radiography and computed tomography showed that the implanted bone was healed. Clinical symptoms were also significantly relieved. None of the patients needed to accept the total hip arthroplasty in 5 years after surgery. No serious perioperative complications were observed in our cases.
Percutaneous expanded core decompression and mixed bone graft technique is simple, safe, and reliable. Advantages of the single blade expandable reamer are obvious. The material of adjuvant substance is inexpensive and easy to obtain. Thus, this technique is an effective joint-preserving surgical treatment for patients with early stage ONFH. This new technique is easy to master as well as costs less than other methods. It is worth popularizing and verifying.
For future research, the effect of age, Kerboul angle, and the size and location of lesions on outcomes should be demonstrated.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: Orthopaedics Committee of Qiqihar Medical Association; and Joint Diseases Alliance of Heilongjiang Medical Association.
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Salvadori M S-Editor: Liu M L-Editor: Filipodia E-Editor: Liu JH
| 1. | Mont MA, Cherian JJ, Sierra RJ, Jones LC, Lieberman JR. Nontraumatic Osteonecrosis of the Femoral Head: Where Do We Stand Today? A Ten-Year Update. J Bone Joint Surg Am. 2015;97:1604-1627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 266] [Cited by in RCA: 346] [Article Influence: 34.6] [Reference Citation Analysis (0)] |
| 2. | Choi HR, Steinberg ME, Y Cheng E. Osteonecrosis of the femoral head: diagnosis and classification systems. Curr Rev Musculoskelet Med. 2015;8:210-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 83] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 3. | Zalavras CG, Lieberman JR. Osteonecrosis of the femoral head: evaluation and treatment. J Am Acad Orthop Surg. 2014;22:455-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 237] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 4. | Banerjee S, Issa K, Pivec R, Kapadia BH, Khanuja HS, Mont MA. Osteonecrosis of the hip: treatment options and outcomes. Orthop Clin North Am. 2013;44:463-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Mont MA, Carbone JJ, Fairbank AC. Core decompression versus nonoperative management for osteonecrosis of the hip. Clin Orthop Relat Res. 1996;324:169-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 372] [Cited by in RCA: 333] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 6. | Mont MA, Zywiel MG, Marker DR, McGrath MS, Delanois RE. The natural history of untreated asymptomatic osteonecrosis of the femoral head: a systematic literature review. J Bone Joint Surg Am. 2010;92:2165-2170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 355] [Cited by in RCA: 301] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 7. | Pierce TP, Elmallah RK, Jauregui JJ, Verna DF, Mont MA. Outcomes of total hip arthroplasty in patients with osteonecrosis of the femoral head-a current review. Curr Rev Musculoskelet Med. 2015;8:246-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2079] [Cited by in RCA: 3260] [Article Influence: 181.1] [Reference Citation Analysis (0)] |
| 9. | Zhao DW, Hu YC. Chinese experts' consensus on the diagnosis and treatment of osteonecrosis of the femoral head in adults. Orthop Surg. 2012;4:125-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 47] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 10. | Pierce TP, Jauregui JJ, Elmallah RK, Lavernia CJ, Mont MA, Nace J. A current review of core decompression in the treatment of osteonecrosis of the femoral head. Curr Rev Musculoskelet Med. 2015;8:228-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 91] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 11. | Musso ES, Mitchell SN, Schink-Ascani M, Bassett CA. Results of conservative management of osteonecrosis of the femoral head. A retrospective review. Clin Orthop Relat Res. 1986;209-215. [PubMed] |
| 12. | Kamath AF, McGraw MH, Israelite CL. Surgical management of osteonecrosis of the femoral head in patients with sickle cell disease. World J Orthop. 2015;6:776-782. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Millikan PD, Karas V, Wellman SS. Treatment of osteonecrosis of the femoral head with vascularized bone grafting. Curr Rev Musculoskelet Med. 2015;8:252-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Kong FG, Han SH, Liu FW, Li YJ. Percutaneous core decompression combined with percutaneous coronary intervention for the treatment of femoral head necrosis in adults. Zhongguo Yiyao Zhinan. 2014;35:32-34. [DOI] [Full Text] |
| 15. | Civinini R, De Biase P, Carulli C, Matassi F, Nistri L, Capanna R, Innocenti M. The use of an injectable calcium sulphate/calcium phosphate bioceramic in the treatment of osteonecrosis of the femoral head. Int Orthop. 2012;36:1583-1588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 57] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 16. | Classen T, Warwas S, Jäger M, Landgraeber S. Two-year follow-up after advanced core decompression. J Tissue Eng Regen Med. 2017;11:1308-1314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 17. | Landgraeber S, Theysohn JM, Classen T, Jäger M, Warwas S, Hohn HP, Kowalczyk W. Advanced core decompression, a new treatment option of avascular necrosis of the femoral head--a first follow-up. J Tissue Eng Regen Med. 2013;7:893-900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 18. | Ohzono K, Saito M, Takaoka K, Ono K, Saito S, Nishina T, Kadowaki T. Natural history of nontraumatic avascular necrosis of the femoral head. J Bone Joint Surg Br. 1991;73:68-72. [PubMed] |
| 19. | Cohen-Rosenblum A, Cui Q. Osteonecrosis of the Femoral Head. Orthop Clin North Am. 2019;50:139-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 119] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 20. | Hernigou P, Beaujean F. Treatment of osteonecrosis with autologous bone marrow grafting. Clin Orthop Relat Res. 2002;405:14-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 422] [Cited by in RCA: 419] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 21. | Houdek MT, Wyles CC, Martin JR, Sierra RJ. Stem cell treatment for avascular necrosis of the femoral head: current perspectives. Stem Cells Cloning. 2014;7:65-70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 22. | Larson E, Jones LC, Goodman SB, Koo KH, Cui Q. Early-stage osteonecrosis of the femoral head: where are we and where are we going in year 2018? Int Orthop. 2018;42:1723-1728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 110] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 23. | Landgraeber S, Warwas S, Claßen T, Jäger M. Modifications to advanced Core decompression for treatment of Avascular necrosis of the femoral head. BMC Musculoskelet Disord. 2017;18:479. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 24. | Landgraeber S, Tran TN, Claßen T, Warwas S, Theysohn J, Lazik A, Jäger M, Kowalczyk W. Geometric analysis of an expandable reamer for treatment of avascular necrosis of the femoral head. Arch Orthop Trauma Surg. 2015;135:1357-1362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Hernigou P, Flouzat-Lachaniette CH, Delambre J, Poignard A, Allain J, Chevallier N, Rouard H. Osteonecrosis repair with bone marrow cell therapies: state of the clinical art. Bone. 2015;70:102-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 92] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 26. | Papakostidis C, Tosounidis TH, Jones E, Giannoudis PV. The role of "cell therapy" in osteonecrosis of the femoral head. A systematic review of the literature and meta-analysis of 7 studies. Acta Orthop. 2016;87:72-78. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 91] [Cited by in RCA: 90] [Article Influence: 10.0] [Reference Citation Analysis (0)] |