Published online Jun 6, 2020. doi: 10.12998/wjcc.v8.i11.2359
Peer-review started: March 11, 2020
First decision: April 14, 2020
Revised: April 27, 2020
Accepted: May 14, 2020
Article in press: May 14, 2020
Published online: June 6, 2020
Processing time: 86 Days and 22.9 Hours
Fistulization is a rare complication of esophageal diverticula. Patients with this condition often require surgery, which unfortunately can be invasive and traumatic. Endoscopic therapy is an alternative method for treating esophageal fistula. Hereby we introduce a new endoscopic technique that uses an esophageal pedicle flap to close esophageal fistulas.
A 49-year-old male patient, complaining of backache and choking, was formerly diagnosed with chronic bronchopneumonia. Chest computed tomography and esophagram confirmed the presence of esophageal diverticulum and mediastinal esophageal fistula. The patient was then treated by covering the fistulas using a pedicled flap that was acquired through endoscopic submucosal dissection of a patch from the proximal esophageal mucosa. Then the pedicle flap was reversed 180° to cover the fistula. Titanium clips were used to fix the flap. The procedure ended with percutaneous endoscopic gastrostomy for enteral nutrition. The patient was followed up to evaluate the size reduction of the fistula. Cough, backache, and fever were alleviated within a week. Forty-five days after the surgery, endoscopic examination showed that the fistulas were reduced in size. The larger one reduced from 0.5 cm to 0.2 cm, while the smaller one was fully closed.
Transplantation of a pedicle flap obtained from the esophageal mucosa endoscopically is minimally invasive for the treatment of fistula.
Core tip: Transplantation of muscle flaps or omental ones for esophageal leakage or fistula from outside the wall is reported to be effective. But surgical intervention often has postoperative morbidities and is contraindicated when the patient has poor health conditions. We developed this endoscopic pedicle grafting method based on the hypothesis that a mucosal flap could induce epithelization. Our single case study showed that the flap can heal a small fistula orifice and can reduce large one. It exhibits the potential to cure selected esophageal fistulas when surgery is not viable.
- Citation: Zhang YH, Du J, Li CH, Hu B. Endoscopic pedicle flap grafting in the treatment of esophageal fistulas: A case report. World J Clin Cases 2020; 8(11): 2359-2363
- URL: https://www.wjgnet.com/2307-8960/full/v8/i11/2359.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i11.2359
The esophageal diverticulum is a rare disorder, which is usually asymptomatic and does not require treatment. Fistulization is a rare complication of esophageal diverticula[1], which often requires surgery that can be invasive and traumatic. In addition, because the diverticulum is a cavity protruding outward from the esophageal lumen, it might not be appropriate to use a stent as treatment.
Flap transplantation has been widely used in plastic surgery for treating various skin defects, chronic ulcers, fistulas, or sinus tracts. Pedicle flap is a type of flap attached to the original site that provides blood supply during grafting. Muscle or omental flaps have been reported to be used in surgical repair of esophageal leakage and fistula[2,3]. Hochberger et al[4] endoscopically transplanted a gastric mucosal flap to prevent esophageal stricture after endoscopic submucosal dissection of early squamous cell carcinoma. Inspired by that study, we hypothesized that the mucosal flap could help induce the closing of esophageal fistula when surgery is contraindicated. Therefore, we improved this mucosal transplantation method by using pedicle esophageal mucosal flap to close mediastinal esophageal fistulas.
A 49-year-old man was admitted to our hospital complaining of reiterative backache, occasional bloody sputum, and choking when eating or drinking.
Symptoms of backache and bloody sputum started 7 years ago. The pain was located in the scapular region. Consequently, the patient was diagnosed with chronic bronchopneumonia and was treated accordingly. Ten months ago, he experienced choking during eating or drinking. Recently, the aforementioned symptoms became aggravated and were followed by a low-grade fever.
The patient had a history of an esophageal diverticulum 10 years ago.
The patient had concomitant mild depression and was taking Olanzapine 2.5 mg qd.
Upon admission, the patient’s temperature was 37.5 °C, pulse rate was 84 bpm, respiratory rate was 19 breaths per minute, and the blood pressure was 102/62 mmHg. Breath sounds at the right lower pulmonary lobe region were reduced, and fine rales could be heard.
Blood analysis revealed that white blood count was 4.49 × 109/L with a neutrophil percentage of 79.3%. The biochemistry test and electrocardiogram were normal. Sputum microbiological cultivation revealed no obvious pathogenic bacteria.
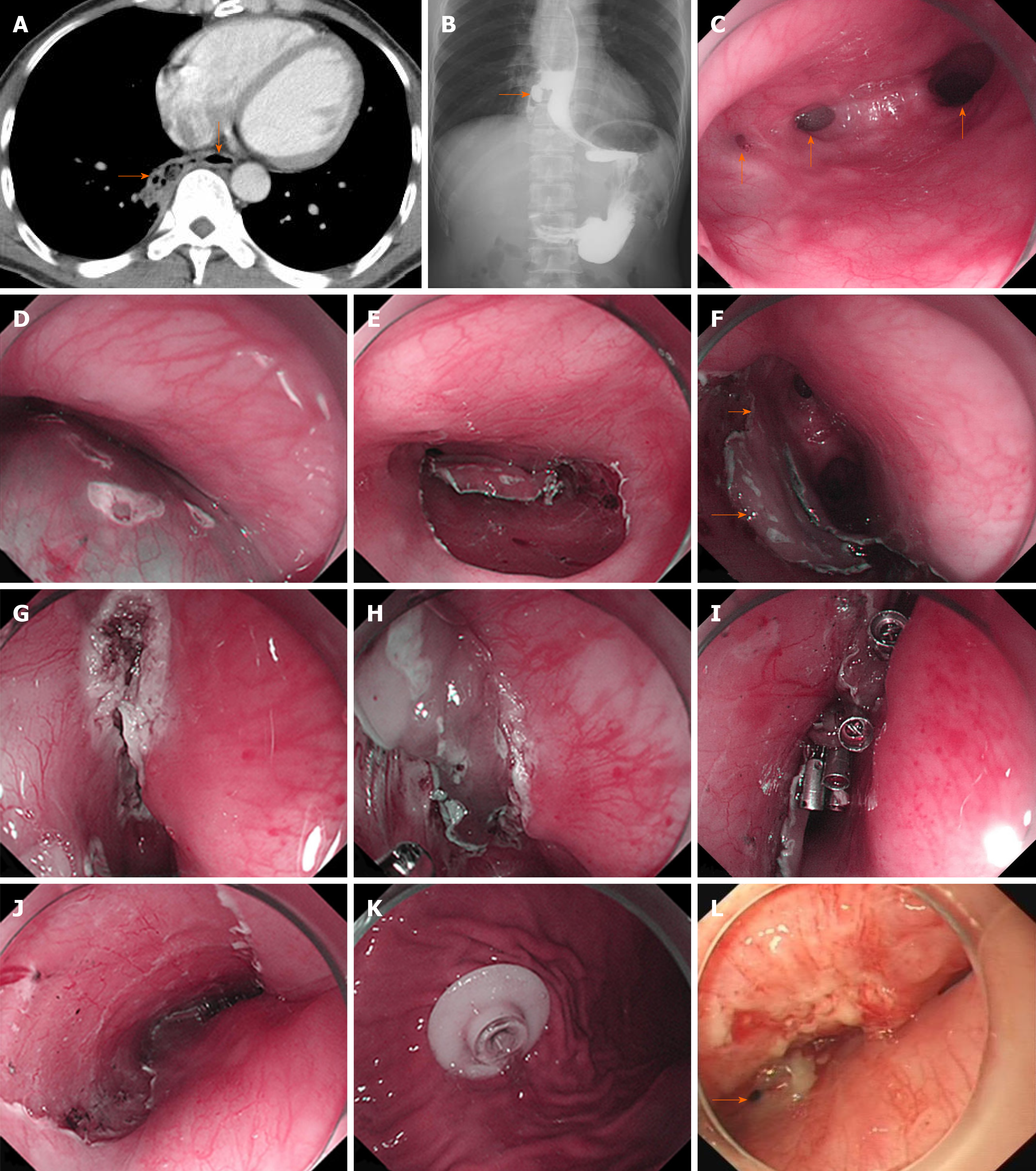
Chest computed tomography showed dilation of the lower esophagus and air in the adjacent mediastinum (Figure 1A). Esophagram confirmed the presence of mediastinal esophageal fistula around the 9th thoracic vertebra level (Figure 1B). In addition, esophagogastroduodenoscopy revealed a giant diverticulum of 2.0 cm in diameter at the right post wall, 32-34 cm aborally. Two fistulas (0.5 cm and 0.3 cm in diameter respectively; 33 cm aborally) were confirmed in the cavity of the diverticulum (Figure 1C).
The final diagnosis suggested an esophageal fistula secondary to spontaneous rupture of the diverticulum.
Based on this diagnosis, surgical resection of the diverticulum or repair of the fistulas was not recommended by the surgeon due to possible side effects related to surgery (uncontrolled mediastinitis or nonhealing of suture wounds) of fistula with chronic infection. In addition, the doctor suggested that a stent should not be applied because it could not seal fistula orifices in the outward protruding diverticulum, and the diverticulum cavity might contain pus. Instead, an endoscopic pedicle flap grafting (EPFG) was recommended and accepted by the patient who signed the informed consent.
Upon admission, the patient was prescribed cefoxitin 2000 mg ivgtt q12h and parenteral nutrition. EPFG was performed under general anesthesia as follows: (1) An area of about 2.0 cm × 1.0 cm cranially to the fistulas was marked; (2) The saline-epinephrine-indigo carmine solution was then injected into the submucosal layer (Figure 1D). Mucosal incision and submucosal dissection were performed (Figure 1E) using a dual knife (Olympus, Tokyo, Japan), leaving the distal edge of the flap (the pedicle, 0.4 cm in diameter) intact; (3) When the pedicle flap was ready (Figure 1F), we applied ablation to the surrounding mucosa of the fistulas using argon plasma coagulation (ERBE, Germany) to make it easier for later attachment (Figure 1G); (4) Rat-tooth forceps were employed to match the free edges of the flap to the ablated mucosa (Figure 1H). Moreover, several titanium clips were used for fixation (Figure 1I) leaving an ulcer area of the original flap (Figure 1J); and (5) Finally, percutaneous endoscopic gastrostomy was performed for future enteral nutrition (Figure 1K).
No procedure-related complications were observed. Ceftriaxone 2000 mg ivgtt qd, esomeprazole 40 mg ivgtt qd, carbazochrome sodium 60 mg ivgtt qd, and enteral nutrition through the percutaneous endoscopic gastrostomy tube were administered after the surgery.
Coughing and backache were relieved, and no fever was observed a week after the surgery. The patient was discharged from the hospital thereafter. Forty-five days after the surgery, endoscopic examination showed that the fistulas were reduced in size. The larger one was reduced from 0.5 cm to 0.2 cm, while the smaller one was fully closed (Figure 1L). We offered the patient a second chance of EPFG, but it was refused. The patient is now considering a surgical option of resecting the diverticulum and is waiting for the clearance of the chronic infection so as to be indicated for surgery by feeding through the percutaneous endoscopic gastrostomy tube.
Esophageal fistulization is usually caused by trauma, surgery, neoplasm, radiation, or erosion. In this case, it occurred on the basis of diverticulum. Diverticulum, which causes fistula, is rather rare and is often misdiagnosed as a lung infection, bronchiectasis, or pulmonary abscess[5]. Surgery or endoscopic techniques are required to remove or close fistulas from the esophagus[6,7]. Yet, surgical closure or resection can be performed only in cases with small defects and without contamination in the mediastinum[8]. In this case, the patient presented with sputum caused by a local infection in the lung and mediastinum, which excluded surgery.
For benign esophageal fistulas, nonsurgical treatment like endoscopic stent placement has similar outcomes compared with surgical modality[9]. Nevertheless, this type of treatment has shown to be effective in only 45% of cases and mainly for patients with punctiform orifices (less than approximately 2.5 mm)[10]. Therefore, the size of the orifices might be slightly larger in our case. In addition, the diverticulum cavity is protruding outward, which makes it difficult for the stent to cover the orifice. In that case, the cavity would become a container for pus, which might induce further inflammation if surgery was performed.
Endoscopic cell sheets and free mucosal flap transplantation have been reported to prevent strictures secondary to endoscopic submucosal dissection[11,12]. On this basis, we hypothesized that a pedicle flap with sufficient blood supply than mere free mucosa would endure longer and exhibit greater potential to close the fistula, reserving the integrity of the esophagus. We chose an adjacent esophageal pedicle flap other than skin or previously reported gastric mucosa because skin could not maintain long-term esophageal function and often develops morphological changes, while gastric mucosa has acid-secreting capability[13].
Although the larger fistula was not completely closed, the reduction in size suggested that this new approach was effective in treating esophageal fistula. Possible reasons for the incomplete closure may be that the course of the disease was too long and that local infection and inflammation impeded epithelization. In view of this, we speculate that selected cases with smaller fistula and little contamination may be better candidates for flap grafting. Nevertheless, future studies with more cases are needed to validate its efficacy and identify best candidates. Comparative studies involving EPFG, stent, and surgical repair using muscle flap are also needed in the future to demonstrate the advantage and disadvantage of each modality. Perhaps a combination of EPFG and stent might also be a choice.
Considering the fistula’s anatomic and physiologic traits, accessibility, and minimally invasive nature, pedicle flap grafting under endoscopy might be a better choice for esophageal fistula. In addition, it exhibits potential to be applied in esophageal fistulas without diverticulum, and its combination with stent could be considered as well. Future studies are needed to explore its clinical applicability.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cho YS, Morales HL S-Editor: Tang JZ L-Editor: Filipodia E-Editor: Xing YX
| 1. | Wang ZM, Zhang SC, Teng X. Esophageal diverticulum serves as a unique cause of bronchoesophageal fistula in children: A case report. Medicine (Baltimore). 2017;96:e9492. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Balakrishnan A, Tapias L, Wright CD, Lanuti MX, Gaissert HA, Mathisen DJ, Muniappan A. Surgical Management of Post-Esophagectomy Tracheo-Bronchial-Esophageal Fistula. Ann Thorac Surg. 2018;106:1640-1646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Asaad M, Van Handel A, Akhavan AA, Huang TT, Rajesh A, Allen MA, Shen KR, Sharaf B, Moran SL. Muscle Flap Transposition for the Management of Intrathoracic Fistulas. Plast Reconstr Surg. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Hochberger J, Koehler P, Wedi E, Gluer S, Rothstein RI, Niemann H, Hilfiker A, Gonzalez S, Kruse E. Transplantation of mucosa from stomach to esophagus to prevent stricture after circumferential endoscopic submucosal dissection of early squamous cell. Gastroenterology. 2014;146:906-909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Zuo CY, Xu ZJ. [Esophageal bronchial fistula secondary to esophageal diverticulum: A case report and literature review]. Zhonghua Jie He He Hu Xi Za Zhi. 2018;41:622-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Onwugbufor MT, Obirieze AC, Ortega G, Allen D, Cornwell EE, Fullum TM. Surgical management of esophageal diverticulum: a review of the Nationwide Inpatient Sample database. J Surg Res. 2013;184:120-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | von Renteln D, Denzer UW, Schachschal G, Anders M, Groth S, Rösch T. Endoscopic closure of GI fistulae by using an over-the-scope clip (with videos). Gastrointest Endosc. 2010;72:1289-1296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 81] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 8. | Uno K, Koike T, Takahashi S, Komazawa D, Shimosegawa T. Management of aorto-esophageal fistula secondary after thoracic endovascular aortic repair: a review of literature. Clin J Gastroenterol. 2017;10:393-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 9. | Lenz CJ, Bick BL, Katzka D, Nichols FC, Depew ZS, Wong Kee Song LM, Baron TH, Buttar NS, Maldonado F, Enders FT, Harmsen WS, Dierkhising RA, Topazian MD. Esophagorespiratory Fistulas: Survival and Outcomes of Treatment. J Clin Gastroenterol. 2018;52:131-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 10. | Debourdeau A, Gonzalez JM, Dutau H, Benezech A, Barthet M. Endoscopic treatment of nonmalignant tracheoesophageal and bronchoesophageal fistula: results and prognostic factors for its success. Surg Endosc. 2019;33:549-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 11. | Hürtgen M, Herber SCA. Treatment of malignant tracheoesophageal fistula. Thorac Surg Clin. 2014;24:117-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 47] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 12. | Leggett CL, Gorospe EC, Lutzke L, Anderson M, Wang KK. A new era: endoscopic tissue transplantation. Curr Opin Gastroenterol. 2013;29:495-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Imaizumi A, Liem AA, Yang CF, Chen W, Chen SH, Chen HC. Long-Term Outcomes of Simultaneous Skin and Bowel Flaps for Esophageal Reconstruction. Ann Plast Surg. 2015;75:180-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |