Published online Mar 26, 2019. doi: 10.12998/wjcc.v7.i6.727
Peer-review started: January 15, 2019
First decision: January 26, 2019
Revised: February 2, 2019
Accepted: February 26, 2019
Article in press: February 26, 2019
Published online: March 26, 2019
Processing time: 71 Days and 23.9 Hours
Hydrocelectomy is the gold standard for the treatment of hydrocele, but it often causes complications after surgery, including hematoma, infection, persistent swelling, hydrocele recurrence, and chronic pain. In recent years, several methods for minimally invasive treatment of hydrocele have been introduced, but they all have limitations. Herein, we introduce a new method of individualized minimally invasive treatment for hydrocele.
To present a new method for the treatment of adult testicular hydrocele.
Fifty-two adult patients with idiopathic testicular hydrocele were included. The key point of this procedure was that the scope of the resection of the sheath of the tunica vaginalis was determined according to the maximum diameter (d) of the effusion measured by ultrasound and the maximum diameter of the portion of the sheath pulled out of the scrotum was approximately πd/2. The surgical procedure consisted of a 2-cm incision in the anterior wall of the scrotum, drainage of the effusion, and dissection of part of the sheath of the tunica vaginalis. After the sheath was peeled away to the predetermined target extent, the pulled-out sheath was removed. The intraoperative findings and postoperative complications were analyzed.
All patients were successfully treated with a median operation time of 18 min. The median maximum diameter of the effusion on ultrasound was 3.5 cm, and the median maximum diameter of the resected sheath was 5.5 cm. Complications occurred in four (7.7%) patients: two (3.8%) cases of mild scrotal edema, one (1.9%) case of scrotal hematoma, and one (1.9%) case of wound infection. All of the complications were grade I-II. Recurrent hydrocele, chronic scrotal pain, and testicular atrophy were not observed during a median follow-up of 12 mo.
We report a new technique for individualized treatment of testicular hydrocele, which is quantitative and minimally invasive and yields good outcomes. Further study is warranted to verify its potential value in clinical practice.
Core tip: Hydrocelectomy, the gold standard for the treatment of hydrocele, often causes complications. We report a minimally invasive technique for individualized treatment of testicular hydrocele. We retrospectively analyzed the records of 52 adult patients with idiopathic hydrocele who underwent this procedure. The extent of tunica vaginalis sheath resection was based on the maximum hydrocele diameter (d) by ultrasound, with the maximum diameter of the resected portion estimated as πd/2. Only a 2-cm incision was required, through which part of the sheath was pulled, separated, and removed. All patients were successfully treated within a short time and with few complications.
- Citation: Lin L, Hong HS, Gao YL, Yang JR, Li T, Zhu QG, Ye LF, Wei YB. Individualized minimally invasive treatment for adult testicular hydrocele: A pilot study. World J Clin Cases 2019; 7(6): 727-733
- URL: https://www.wjgnet.com/2307-8960/full/v7/i6/727.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i6.727
Testicular hydrocele is a common benign disease in men[1,2]. Hydrocelectomy is recognized as the gold standard for the treatment of hydrocele[3-5], but it often causes complications after surgery, including hematoma, infection, persistent swelling, hydrocele recurrence, and chronic pain[2,5]. In recent years, several methods for minimally invasive treatment of hydrocele have appeared, such as hydrocelectomy with a small (3 cm) incision[6] and a 1.5-cm incision pull-out technique for hydrocele[5]. Saber reported a 2-cm incision procedure and excised only a small portion of the disk of the parietal tunica vaginalis, which otherwise would require to double the size of the incision[3,4]. Herein, we introduce a new method for individualized minimally invasive treatment of hydrocele. Unlike the existing procedures, our procedure is individualized and quantitative as well as minimally invasive.
From September 2010 to January 2018, a total of 52 adult patients with idiopathic testicular hydrocele underwent our procedure. The median age was 53 years (range, 23-78 years). Three of the patients had bilateral testicular hydroceles and the remaining 54 had a unilateral lesion. The median duration was 11 mo (range, 3 mo-8 years). Physical examination showed a swollen scrotum on the lesion side, the testis and epididymis were nonpalpable, and the transillumination test was positive. All of the patients underwent scrotal ultrasound examinations in the outpatient department before admission. Patients were included if they met the following criteria: (1) scrotal symptoms that disturb their daily life; (2) diagnosis of testicular hydrocele; (3) agreement to undergo treatment according to this surgical protocol; and (4) absence of other scrotal conditions or diseases such as trauma, tumor, hernia, testicular torsion, acute infection of the scrotal skin, communicating hydrocele, or tuberculosis of the epididymis or testis. All of the enrolled patients were confirmed to have idiopathic testicular hydrocele, without previous scrotal trauma, surgery, puncture, or sclerotherapy. None had chronic illnesses such as severe heart and lung disease, acute infectious diseases, or coagulopathy.
The following data were obtained and analyzed for the purpose of evaluating the clinical outcomes: maximum effusion diameter of the hydrocele according to ultrasound, maximum resection diameter of the parietal tunica vaginalis, operation time, postoperative complications, and patient satisfaction. All of the patients provided written informed consent. All of the study data were securely maintained by a single investigator. The data were obtained solely for the purpose of this study and are not intended for other uses.
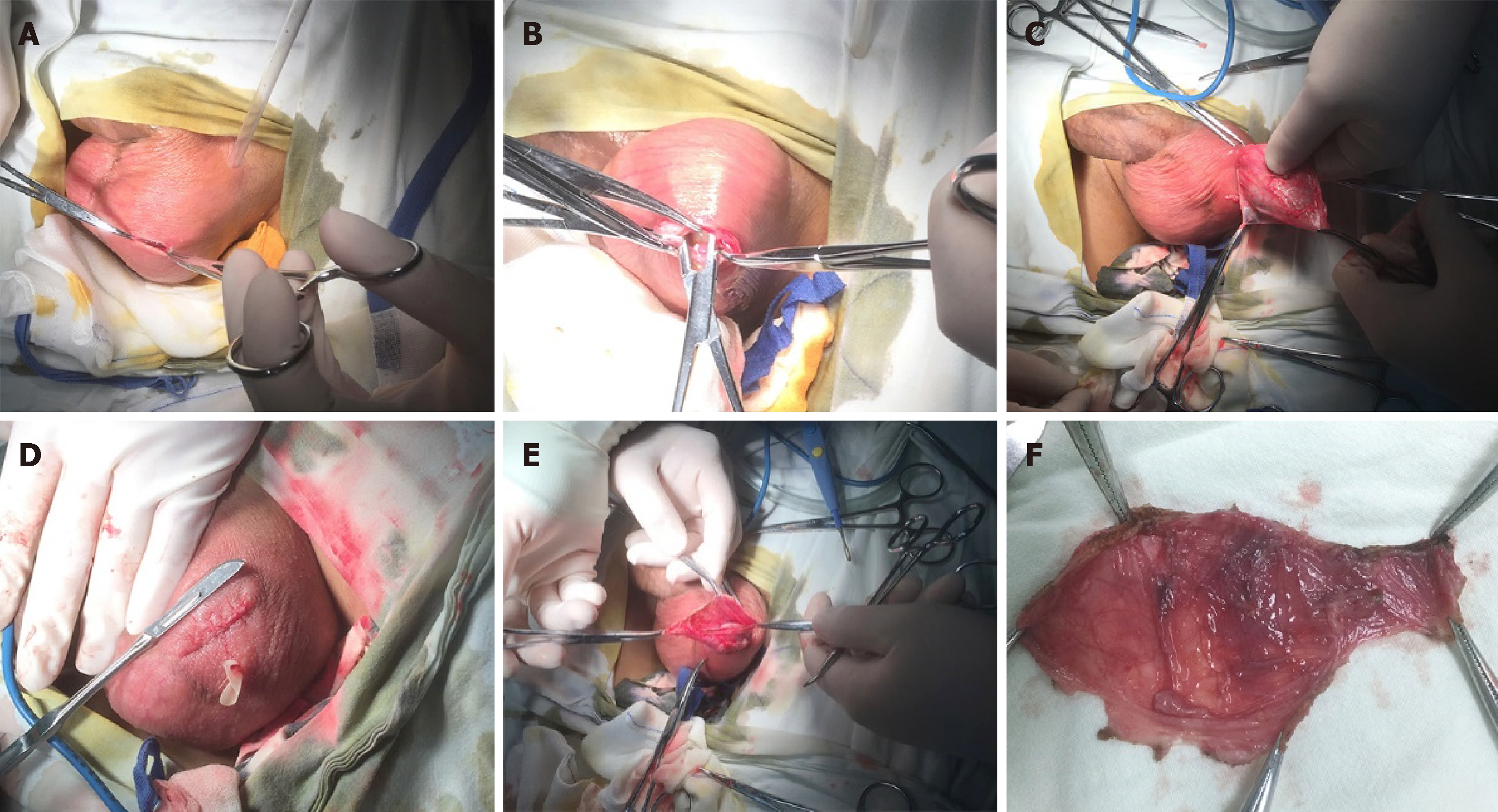
Prophylactic antibacterial treatment was given between 30 min and 2 h before surgery. Lumbar, general, or local anesthesia was administered. Both lithotomy and supine positions were suitable. We then sterilized the perineum and placed a plastic incision drape. Using the left hand and aided by an assistant to squeeze and tighten the scrotum on the affected side, we made a 2-cm incision in the transverse anterior skin of the scrotum (Figure 1A). An electrotome (electroresection at 60 w and electrocoagulation at 40 w) was used to sequentially separate the dartos, external spermatic fascia, cremaster muscle, internal spermatic fascia, and parietal tunica vaginalis and then enter the sheath cavity (Figure 1B). The pale-yellow effusion was released or aspirated from the scrotum. The sheath of the tunica vaginalis was gently pulled with several vascular clamps and bluntly dissected from the other tissues of the scrotum. Hemostasis was maintained during the dissection. If necessary, the forefinger of the left-hand was extended into the sheath cavity to assist the separation (Figure 1C); this both helped to separate the sheath tissue and also protected the testis, epididymis, and spermatic cord from damage. The sheath tissue was separated as much as possible until reaching the intended target size, leaving the remaining part surrounding the testis, epididymis, and spermatic cord intact (Figure 1D). Electrocoagulation was used to remove the peeled-out sheath, and the wound edge of the sheath was completely coagulated to stop bleeding. Another 0.5-cm incision was made at the bottom of the scrotum, and then a rubber drainage membrane was placed. Finally, the absence of active bleeding, torsion, or any testicular, epididymis, or spermatic cord injury was confirmed. Then, the incision was closed with absorbable sutures (Figure 1E). A supportive pressure dressing was routinely placed on the scrotum. The wound dressing was changed regularly and the drainage membrane was removed within 24 to 48 h after surgery. The resected sheath tissue was routinely sent for pathological examination (Figure 1F).
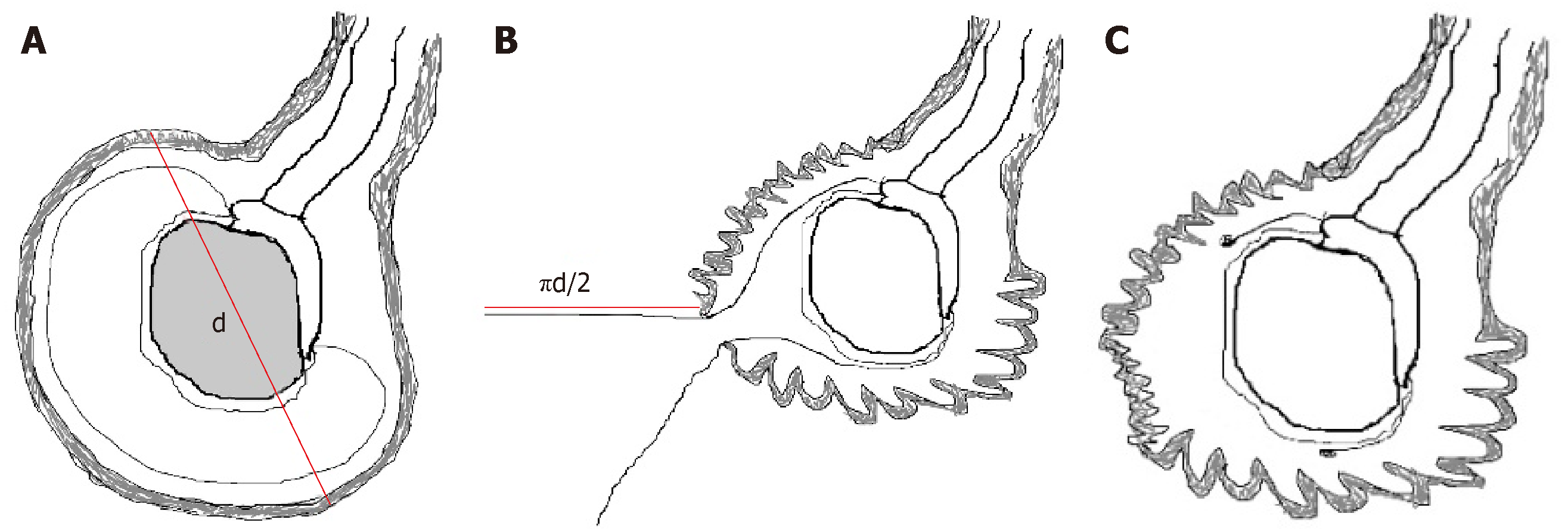
The amount of the sheath removed intraoperatively was according to the maximum diameter of the effusion on ultrasound. The maximum diameter of the peeled sheath was preoperatively estimated according to this ultrasound result. If the maximum diameter of the effusion measured by preoperative ultrasound is d (Figure 2A), the maximum diameter of the sheath that should be peeled off through the small incision would be approximately πd/2 (Figure 2B); this ensured that an adequate amount of sheath was removed (Figure 2C) to prevent recurrence of hydrocele.
All patients completed the operation successfully, with a median operation time of 18 min (range, 13-35 min). The median maximum diameter of the effusion was 3.5 cm (range, 2 cm-12 cm) according to ultrasound. The sheath was removed to reach the preoperative predetermined resection size; that is, its median maximum diameter was 5.5 cm (range, 3.0-18.5 cm). The normality of the resected sheath tissue of the tunica vaginalis was confirmed by postoperative pathological examination. A total of four (7.7%) patients experienced complications. There were two cases (3.8%) of slight scrotal edema and one (1.9%) case of scrotal hematoma; these three patients completely recovered within 48 h of local scrotal compression dressing. One (1.9%) patient developed a wound infection that resolved after 7 d of antibacterial treatment and dressing changes. Acute complications such as injury of the testis, epididymis, or spermatic cord did not occur. According to the classification of surgical complications[7], our complications were all grade I-II. The median length of hospitalization was 2 d (range, 1-5 d). The patients returned to their routine daily activities in a median of 4 d after surgery. The median follow-up period was 12 mo (range, 12-23 mo). One (1.9%) patient expressed dissatisfaction with the surgery, 48 (48/52, 92.3%) were satisfied, and 3 (3/52, 5.7%) reported neutrality. No recurrence of hydrocele, chronic scrotal pain, or testicular atrophy occurred during follow-up.
Testicular hydrocele is a common benign disease in men. The incidence of testicular hydrocele in the male population is about 1%[1,2]. Its treatment can be determined according to the patient age, the size of the hydrocele, and the severity of symptoms. Hydrocelectomy is the gold standard for the treatment of hydrocele[3-5]. However, due to the large incision size and the subsequent large area of separation inside the scrotum, the patient must limit activity after surgery and may experience scrotal discomfort and complications such as scrotal hematoma, wound infection, persistent scrotal pain, and even impaired fertility[2,5]. Puncture aspiration and sclerotherapy are used for conservative treatment of hydrocele but are not widely performed due to uncertain outcomes, strong local response, and high recurrence rates[8,9].
There are several methods for surgical treatment of testicular hydrocele, including sheath fenestration proposed by Ozdilek[10] in 1957, and sheath folding reported by Lord[11] in 1964. In recent years, the surgical treatment of hydrocele has gradually developed in the direction of minimal invasion. The objective of the minimally invasive procedures is to use the smallest incisions possible and to narrow the scope of anatomical separation without compromising the outcomes of safety and effectiveness[12]. As early as 2002, Chalasani and Woo[6] proposed a minimally invasive treatment of hydrocele with a small incision of 3 cm. In 2009, Onol et al[5] used a 1.5-cm incision to pull the sheath out of the scrotum and then remove it. These kinds of surgeries have in common the small skin incisions, but they still entail the removal of most or even all of the anterior wall of the sheath.
Our surgical procedure is basically similar to that of Onol et al[5], in which most of the sheath is removed through the small incision to prevent hydrocele recurrence. Thus, our procedure retains the advantages of that of Onol et al[5]; namely, small incision, few complications, and quick recovery. The main difference between ours and that of Onol et al[5] is that we individualized the treatment. The amount of the sheath removed from each patient was quantified according to the maximum diameter of the hydrocele effusion determined by preoperative ultrasound. In contrast, during the procedure of Onol et al[5], the range of sheath resection was completely determined according to the surgeon's experience[5]. Although their recurrence rate was reportedly low, it is difficult for other surgeons to consistently replicate the procedure. In contrast, our protocol of individualized and quantitative treatment is both simple to perform and easily replicated.
In 2011, Saber[3,4] first reported a procedure involving a 2-cm small incision and a sheath resection size twice that of the incision, which means that all patients underwent resection of approximately 4 cm of the sheath. In Saber’s report, a total of 62 patients accepted the surgery, its median operation time was 15.1 min, and the overall complication rate was 12.88% with no occurrence of hematoma; 75.8% of the patients reported satisfaction, and one patient (1.6%) experienced hydrocele recurrence[3]. In comparison, the size of our sample was slightly smaller (52 cases), the median operation time was slightly longer (18 min), and the overall complication rate seems lower (7.7%) with hematoma occurring in one case (1/52, 1.9%); however, the patient satisfaction rate was slightly higher (48/52, 92.3%) and, most importantly, none of our patients had recurrence of hydrocele. These two studies are comparable with regard to the incision size and the incidence of complications. Our more positive outcomes may be partly attributed to our providing a special care manager to establish a strong partnership with the patient and to collaborate with the physician, positively impacting patient health and self-management[13]. This management model might help reduce the occurrence of avoidable complications and enhance patients’ satisfaction with this medical service.
As our procedure sometimes entailed a relatively large extent of sheath separation and resection, the longer operation time in some cases and a more frequent occurrence of sheath hematoma are understandable. However, the postoperative complications in our study cohort were all grade I-II, and there was no hydrocele recurrence. In contrast, there was one case of grade III hydrocele recurrence reported in Saber’s study. Such recurrences may require interventional treatment such as reoperation[3]. For the Saber procedure, the recurrence of hydrocele could be predictable, as the scope of the hydrocelectomies was fixed at 4 cm for all patients[3]. In our opinion, a 4 cm resection may be sufficient when the maximum diameter of the effusion is approximately 2.5 cm. However, this resection limit would be too restrictive and the possibility of hydrocele recurrence would significantly increase if the maximum diameter of the effusion is extensive (8 cm or greater). Unlike Saber’s procedure, ours was an individualized and quantitative treatment, thus ensuring that the possibility of recurrence could be reduced to a very low level.
In recent years, the scrotoscope has also been used in the diagnosis and treatment of scrotal lesions such as hydrocele[14] and epididymal cysts[15]. As there may be a small secondary part of the hydrocele, and because some primary diseases cannot be detected even when ultrasound is combined with other imaging tests[9], the main purpose of the application of a scrotoscope in this situation is to provide direct visualization of the contents of the scrotum and to confirm or exclude primary diseases[14,15]. In this situation, if the sheath of the tunica vaginalis is simply removed through a small incision, the primary important causes of the hydrocele may be misdiagnosed[9,14,16,17]. The selected cases in our study underwent careful physical examination together with ultrasound and other auxiliary examinations before the diagnosis of idiopathic hydrocele was made. Patients whose preoperative diagnoses were not confirmed were not included in our study. Scrotoscopy or traditional surgical treatments were provided for those patients. Furthermore, the postoperative pathological results were consistent with the preoperative diagnosis and no other scrotal lesions were found during a median follow-up period of 12 mo, suggesting that all patients in our study had idiopathic hydrocele.
This study had limitations associated with a retrospective study design. Also, the sample size is small; this relates to the hierarchical medical system in our country whereby many patients are treated at local medical institutions. We plan to introduce our procedure at these medical institutions and perform further cooperative evaluations of its application. Finally, the extent of sheath removal is based on the experience of our team; the quantitative resection estimate has not been rigorously verified by mathematical models. Future randomized clinical trials with larger sample size are needed to further determine the clinical value of this procedure.
This new surgical treatment for testicular hydrocele is individualized, quantifiable and minimally invasive and yields positive safety and effectiveness outcomes. Additional study is warranted to verify the potential utility of this procedure in clinical practice.
Hydrocelectomy is the gold standard for the treatment of hydrocele, but it often causes complications, including hematoma, infection, persistent swelling, hydrocele recurrence, and chronic pain. Several methods for minimally invasive treatment of hydrocele have been introduced, but they all have limitations. We retrospectively analyzed the records of 52 adult patients with idiopathic testicular hydrocele who underwent a new minimally invasive technique for individualized treatment of testicular hydrocele from September 2010 to January 2018.
To investigate the feasibility of this individualized treatment.
To present a new method of treatment of adult patients with idiopathic testicular hydrocele.
The study subjects were 52 adult patients with idiopathic testicular hydrocele who underwent the minimally invasive procedure. We designed the resection of the sheath of the tunica vaginalis according to the maximum diameter (d) of the hydrocele by ultrasound; the maximum diameter of the removal sheath was estimated as πd/2. A 2-cm incision in the anterior wall of the scrotum was made, through which the sheath of the tunica vaginalis was pulled out and peeled away from the underlying scrotal contents. After the sheath was dissected to the predetermined extent, it was removed. The intraoperative findings and postoperative complications were analyzed.
All patients were successfully treated within a median operation time of 18 minutes. The median maximum diameter of the effusion on ultrasound was 3.5 cm, and the median maximum diameter of the resected sheath was 5.5 cm. Complications occurred in four (7.7%) patients: two (3.8%) cases of mild scrotal edema, one (1.9%) case of scrotal hematoma, and one (1.9%) case of wound infection. All of the complications were grade I-II. Recurrent hydrocele, chronic scrotal pain, and testicular atrophy were not observed during a median follow-up period of 12 mo.
We report a new technique for the individualized treatment of testicular hydrocele, which is quantitative and minimally invasive and yields good outcomes.
We provide a promising application of this individualized treatment for hydrocele; more clinical studies may be needed to verify its safety and efficacy.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ciccone MM, Khuroo MS S-Editor: Ji FF L-Editor: Wang TQ E-Editor: Wu YXJ
| 1. | Mihmanli I, Kantarci F. Sonography of scrotal abnormalities in adults: an update. Diagn Interv Radiol. 2009;15:64-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Kiddoo DA, Wollin TA, Mador DR. A population based assessment of complications following outpatient hydrocelectomy and spermatocelectomy. J Urol. 2004;171:746-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 45] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 3. | Saber A. Minimally access versus conventional hydrocelectomy: a randomized trial. Int Braz J Urol. 2015;41:750-756. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Saber A. New minimally access hydrocelectomy. Urology. 2011;77:487-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Onol SY, Ilbey YO, Onol FF, Ozbek E, Arslan B, Akbaş A. A novel pull-through technique for the surgical management of idiopathic hydrocele. J Urol. 2009;181:1201-1205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Chalasani V, Woo HH. Why not use a small incision to treat large hydroceles? ANZ J Surg. 2002;72:594-595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18532] [Cited by in RCA: 24754] [Article Influence: 1178.8] [Reference Citation Analysis (0)] |
| 8. | Khaniya S, Agrawal CS, Koirala R, Regmi R, Adhikary S. Comparison of aspiration-sclerotherapy with hydrocelectomy in the management of hydrocele: a prospective randomized study. Int J Surg. 2009;7:392-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Cimador M, Castagnetti M, De Grazia E. Management of hydrocele in adolescent patients. Nat Rev Urol. 2010;7:379-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Ozdilek S. The pathogenesis of idiopathic hydrocele and a simple operative technique. J Urol. 1957;77:282-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Lord PH. A bloodless operation for the radical cure of idiopathic hydrocele. Br J Surg. 1964;51:914-916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 69] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 12. | Darzi A, Mackay S. Recent advances in minimal access surgery. BMJ. 2002;324:31-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 72] [Article Influence: 3.1] [Reference Citation Analysis (1)] |
| 13. | Ciccone MM, Aquilino A, Cortese F, Scicchitano P, Sassara M, Mola E, Rollo R, Caldarola P, Giorgino F, Pomo V, Bux F. Feasibility and effectiveness of a disease and care management model in the primary health care system for patients with heart failure and diabetes (Project Leonardo). Vasc Health Risk Manag. 2010;6:297-305. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 128] [Cited by in RCA: 136] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 14. | Bin Y, Yong-Bao W, Zhuo Y, Jin-Rui Y. Minimal hydrocelectomy with the aid of scrotoscope: a ten-year experience. Int Braz J Urol. 2014;40:384-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 15. | Yang JR, Wei YB, Yan B, Yin Z, Gao YL, Wang Z, Zhou KQ. Comparison between Open Epididymal Cystectomy and Minimal Resection of Epididymal Cysts Using a Scrotoscope: A Clinical Trial for the Evaluation of a New Surgical Technique. Urology. 2015;85:1510-1514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Hegde S, Jadhav V, Shankar G. Not a Hydrocele! J Pediatr. 2018;197:311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Maheshwari PN, Abiola OO, Wagaskar VG, Oswal AT. Hydrocele with a surprise: Malignant mesothelioma of the tunica vaginalis - Case report and review of literature. Urol Ann. 2017;9:110-112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |