Published online Mar 26, 2019. doi: 10.12998/wjcc.v7.i6.691
Peer-review started: November 26, 2018
First decision: December 12, 2018
Revised: January 10, 2019
Accepted: January 26, 2019
Article in press: January 26, 2019
Published online: March 26, 2019
Processing time: 124 Days and 21.8 Hours
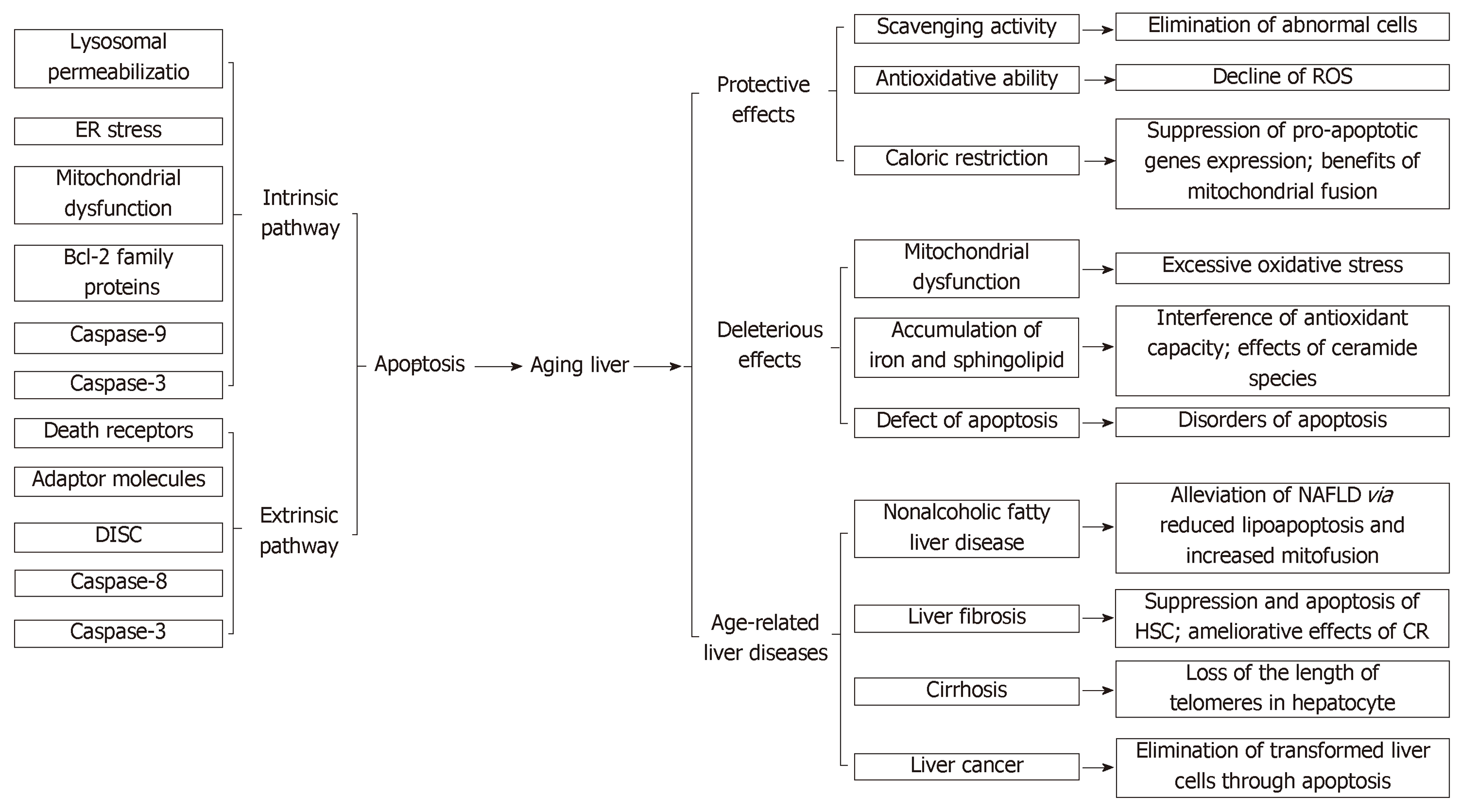
As an irreversible and perennial process, aging is accompanied by functional and morphological declines in organs. Generally, aging liver exhibits a decline in volume and hepatic blood flow. Even with a preeminent regenerative capacity to restore its functions after liver cell loss, its biosynthesis and metabolism abilities decline, and these are difficult to restore to previous standards. Apoptosis is a programmed death process via intrinsic and extrinsic pathways, in which Bcl-2 family proteins and apoptosis-related genes, such as p21 and p53, are involved. Apoptosis inflicts both favorable and adverse influences on liver aging. Apoptosis eliminates transformed abnormal cells but promotes age-related liver diseases, such as nonalcoholic fatty liver disease, liver fibrosis, cirrhosis, and liver cancer. We summarize the roles of apoptosis in liver aging and age-related liver diseases.
Core tip: Aging liver exhibits functional and morphological changes. Apoptosis eliminates transformed abnormal cells but promotes age-related liver diseases, such as nonalcoholic fatty liver disease, liver fibrosis, cirrhosis, and liver cancer. Apoptosis including intrinsic and extrinsic pathways has protective and deleterious effects on liver aging. The occurrence, development, and treatment of age-related liver diseases correlate highly with liver aging and apoptosis. This paper elaborates the effects of apoptosis on liver aging.
- Citation: Hu SJ, Jiang SS, Zhang J, Luo D, Yu B, Yang LY, Zhong HH, Yang MW, Liu LY, Hong FF, Yang SL. Effects of apoptosis on liver aging. World J Clin Cases 2019; 7(6): 691-704
- URL: https://www.wjgnet.com/2307-8960/full/v7/i6/691.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i6.691
Aging process is always accompanied by a gradual decline in the physiological functions of tissues and organs. In the late phase, aging goes along with some degenerative diseases and mortality. Aging liver exhibits some age-related changes, such as a decline in volume and hepatic blood flow[1]. In aging people, the liver shows a brown-like appearance, which is usually caused by the accumulation of lipofuscins in the liver cells with aging[2]. Liver cell survivability decreases due to excessive reactive oxygen species (ROS) caused by lipofuscins[3]. Liver cells consist of hepatocytes and non-hepatocytes, and non-hepatocytes include endothelial cells, Kupffer cells, lymphocytes, stellate cells, and biliary cells[4]. As a site of immune maturation and differentiation, aging liver involves some immune-related changes[5]. There were some immune cells such as macrophages, natural killer cells, T cells, B cells, and neutrophils congregating in the liver tissue of the aged mice[6]. The inflammatory cytokines and chemokines also increased in the aged liver, which caused inflammation and associated with the foreign antigens into the liver. Furthermore, it has also been shown that the increased natural killer cells and macrophages in the aged liver produced more interferon gamma, which impaired the capacity of liver regeneration[7]. The aging process of the liver is associated with the decline of immune response compared with young liver, rendering aging liver more susceptible to infections, malignancies, and autoimmunity[8-10]. During the aging process, mitochondrial dysfunction is induced by perturbation in the electronic conversion process, which results in the reduction of adenosine triphosphate (ATP) production and the increase in oxidation products, such as phospholipids, proteins, and DNA[11]. ROS are by-products of oxidative phosphorylation in the mitochondria. As a perpetrator, senescence severely impairs the antioxidant capacity of normal cells, and its resultant ROS products trigger oxidative stress, damage mitochondrial DNA, and may eventually lead to DNA mutations[12].
As a programmed death pathway, apoptosis can eliminate some degenerative cells, such as abnormal polyploid liver cells, via intrinsic or extrinsic pathways[13]. The former resorts to pro-apoptotic proteins like cytochrome c, and the latter is mainly dependent on death receptors to induce apoptosis. Apoptosis and aging are generally believed to be two biological interaction processes, in which aging regulates the apoptosis progression, and abnormal apoptosis conversely influences the normal aging process[14]. Aging reduces the expressions of several key molecules in the endoplasmic reticulum (ER) and affects its biological functions, including protein folding and lipid synthesis, thereby resulting in ER stress[15]. When long-term chronic ER stress is not relieved in aging liver, the disordered lipid metabolism may cause lipotoxicity that, in turn, would induce cell apoptosis and may finally cause development of non-alcoholic fatty liver disease (NAFLD)[16]. Although some progress has been made in recent years, the interrelationships among apoptosis, hepatic organ senescence, and age-related liver diseases are not yet fully clear. We recently reported the causes of apoptosis during liver aging[17]. Here, we reference and summarize the recent relevant literature to further elaborate the effects of apoptosis on liver aging.
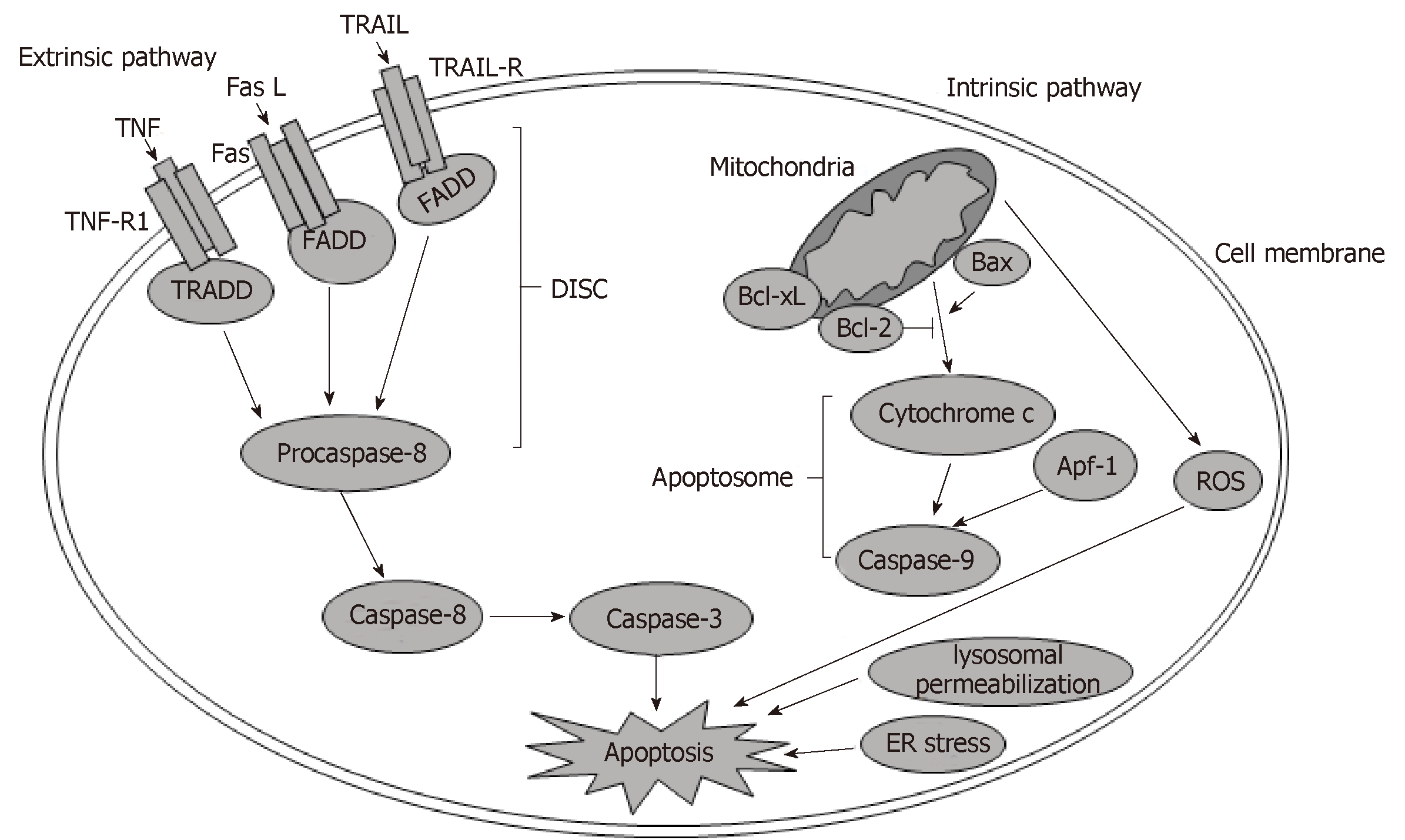
Cell apoptosis is mediated by extracellular or intracellular cascade signaling pathways separately. The extracellular pathway mainly involves special ligands activating its receptors through inward signaling pathways. By contrast, the intracellular apoptosis pathway relies on intracellular organelles, like the mitochondrion and ER[17].
The binding of extracellular ligands and their corresponding receptors on the plasma membrane is the first step by which cell apoptosis is initiated within the extrinsic signaling pathway. These receptors are known as death receptors, including tumor necrosis factor receptor 1 (TNF-R1), TNF-related apoptosis-inducing ligand receptor (TRAIL-R), and Fas[18]. The corresponding extracellular ligands include TNF-alpha (TNF-α), TRAIL, and Fas ligand. When the death receptors are activated by their ligands, conformational changes of death receptors occur, and a tripolymer is formed. Furthermore, the activated receptors recruit cytoplasmic adaptor molecules, including Fas-associated death domain-containing protein and TNFR-associated death domain[19]. Moreover, apoptosis signaling molecules are also recruited. Adaptor molecules then bind with apoptosis-signaling molecules to form a complex named the death-inducing signaling complex (DISC)[20]. Eventually, DISC leads to the activation of caspase-8, and caspase-8 activates executioner caspases, such as caspase-3, to induce apoptosis[21].
Within the intrinsic pathway, organelle dysfunction triggers apoptosis from diverse perspectives. For instance, lysosomal permeabilization, ER stress, mitochondrial dysfunction, and the perturbation of other organelles are all involved in apoptosis[22]. Among these organelles, the mitochondrion is the protagonist in the initiation and progression of apoptosis[23]. Mitochondrial dysfunction induces the opening of mitochondrial permeability transition pore (mtPTP), which allows the release of pro-apoptotic proteins, such as cytochrome c, from mitochondrial intermembrane space into the cytoplasm. Subsequently, with the participation of cytochrome c, apoptotic-protein activation factor-1, and caspase-9, a complex known as the apoptosome is formed, which activates downstream effector caspase-3 to induce apoptosis (Figure 1)[24,25].
The mitochondrion is regulated directly or obliquely by Bcl-2 family proteins, which can be divided into three groups: the pro-apoptotic multi-domain proteins consisting of Bax, Bak, and Bok; the pro-apoptotic BH3-only proteins, such as Bad; and the anti-apoptotic multi-domain proteins, including Bcl-2, Bcl- XL, and Bcl-W[26,27]. With additional proapoptotic proteins, the ratio of pro-apoptotic proteins to anti-apoptotic proteins, such as Bax/Bcl-2, is increased significantly, which causes cellular apoptosis[28]. Mitochondrial dysfunction results in the generation of ROS, which are engendered primarily by deployed electron transport chain and excessive stress in the mitochondrion[29]. Given that the majority of oxygen is consumed in the mi-tochondrion, the mitochondrion determines the generation of most oxygen free radicals and hydroperoxides. Given that mitochondrial dysfunction contributes to the overloading of ROS, overabundance of ROS is detrimental and leads to lipotoxicity, DNA lesion, and protein damage[30,31].
Under physiological conditions, hepatic intrinsic apoptosis increases with age[32]. When exposed to genotoxins from daily diets and free radicals, injured hepatocytes may form neoplasia without sufficient self-clearance due to DNA damage[33]. Fortunately, apoptosis eliminates abnormal cells in a timely manner to avoid malignant change and preserve homeostasis. In contrast to abnormal cells, normal liver cells proliferate and are renewed, thereby maintaining their fundamental physiological function[34]. Giorgadze et al[35] evaluated the effects of age on hepatocyte apoptosis and proliferation in male rats under physiological conditions. Their results suggested that in senescent rats, the amount of polyploid nuclei in liver cells was dramatically high compared with that in young rats. However, polyploid cells exhibited less survival opportunity compared with liver cells. If excessive polyploid cells are present, and renewing cells are lacking, failure may occur during liver damage. Given that polyploid cells are eliminated through apoptosis to avoid liver failure, apoptosis is deemed to protect liver aging.
The free radical theory of aging was first proposed by Harman in 1956, in which oxidative stress was thought to be associated with aging intimately[36]. During liver aging, excessive oxidative stress generates ROS, which perturb the balance between oxidative and antioxidative processes and induce liver injury. Moderate apoptosis can maintain hepatic homeostasis by purging transformed cells. However, excessive oxidative stress induces excessive apoptosis, impairs hepatic function, and accelerates liver aging[37]. Hence, resolving oxidative stress can be a valid strategy to reduce apoptosis and to protect the liver from ROS overload.
Martin et al[38] studied the impact of long-term Mg intake on oxidative stress and apoptosis in rat livers. Treated with deficient Mg dose diets, rat livers showed a decline in glutathione peroxidase (GSH-Px) activity and caspase-3 activation. In addition, telomere shortening was observed in the Mg-deficient group[38]. Herein, adequate Mg dose in diets may reduce oxidative damage and apoptosis, which slows down the progression of liver aging. D-galactose (D-Gal), a monosaccharide consisting of six carbons and one aldehyde, was used to mimic the natural aging process in mice through the induction of oxidative damage and cellular apoptosis[39]. Moderate concentration of D-gal can be wholly metabolized, but its high dose induces ROS that further trigger apoptosis[40]. Based on the aging animal model, whose senescence is induced with D-Gal, drugs at a certain amount are used to counteract oxidative stress, thereby reducing liver damage. Colla corii asini (E’jiao), a traditional Chinese medicine, ameliorates superoxide dismutase (SOD), catalase (CAT), and GSH-Px activities to slow down aging process in D-Gal-induced mice[41]. As a by-product of silymarin production, Silybum marianum oil decreases monoamine oxidase and malondialdehyde (MDA) levels to alleviate oxidative damage apart from improving SOD and GSH-Px activities[42]. Furthermore, polydatin treatment can enhance antioxidant enzyme activities, increase Bcl-2/Bax ratio, and down-regulate caspase-3 protein expression to mitigate D-Gal-induced liver damage[43]. In general, apoptosis is a serviceable and efficacious target for many drugs to diminish oxidative stress and lower liver injury during aging.
Dieting, a vital and protective approach for delaying aging, is very significant in preserving liver function, and caloric restriction (CR) is a major participant in slowing the aging process and extending the life span of animals[44]. CR attenuates the generation of H2O2 in the mitochondria of rat liver and increases the activities of SOD, CAT, and GSH-Px at old age[2,45]. In addition, CR protects the liver through the modulation of apoptosis-related genes. Higami et al[46] examined the effects of aging and diet restriction on the Fas gene. They found that the overexpression of Fas in advanced age increased the susceptibility to apoptosis. However, diet restriction can suppress the overexpression of Fas to reduce apoptosis in hepatocyte aging[46]. The expression of not only Fas but also Fas receptor mRNA is affected by CR. With a 30% reduction in food intake in aging male F344 rats, age-enhanced Fas receptor mRNA and pro-apoptotic gene p53 expression in hepatocytes were suppressed by CR, thereby improving hepatocyte survival in senescent liver[47]. Furthermore, gadd153, a pro-apoptotic gene, is affected by liver aging and CR. Ikeyama et al[48] examined the effects of liver aging and CR on gadd153. Aging increased the expression of gadd153, which sensitized hepatocytes to oxidative damage. CR also decreased the decline of oxidative stress tolerance and attenuated gadd153 expression. Herein, CR reduced oxidative stress and suppressed the overexpression of pro-apoptotic genes, such as gadd153 and Fas, to address liver injury.
The anti-aging ability of CR is also implicated by mitochondrial dynamics involving fusion and fission. The outer membrane GTPases mitofusin 1 (Mfn1) and Mfn2 collaborate with the inner membrane GTPase, optic atrophy 1 (OPA1), to regulate mitochondrial fusion[49]. Mitochondrial fission is mainly regulated by a GTPase, referred to as dynamin-related protein 1, the corresponding receptor of which is fission 1 (Fis1)[50]. In a study by Khraiwesh et al[51], the expression of OPA1 as it relates to mitochondrial fusion can be significantly increased by CR, which can also reduce the expression of Fis1 in hepatocytes. Increased OPA1 upregulates mitochondrial fusion, which is known as an underlying and effective mitochondrial complementation of mtDNA defects[52]. For instance, the complementation of respiratory deficiency caused by mutant mtDNAs significantly reduces oxidative stress[53]. Furthermore, overexpression of the mitochondrial fission protein, Fis1, promotes apoptosis, indicating that Fis1 may be a driver of apoptosis[54]. Downregulation of Fis1 expression reduces mitochondrial fission and leads to extensive mitochondrial elongation and elevated levels of PTEN-induced putative kinase 1, both of which lead to resistance of old cells to oxidative stress-induced apoptosis[55]. Therefore, CR can maintain mitochondrial homeostasis and reduce mitochondrial oxidative stress to slow the aging process through the regulation of mitochondrial fusion and fission.
The mitochondrion, the main producer of intrinsic ROS, is the core component in apoptosis during liver aging. In aging process, mitochondrial dysfunction leads to an imbalance between ROS production and antioxidant ability[56]. Therefore, aging can be recognized as a risk factor for apoptosis in maintaining liver mitochondrial homeostasis[57]. Braidy et al[58] investigated the influence of aging on cofactor nicotinamide adenine dinucleotide (NAD+). They found that the decline of intracellular NAD+ with age reduced mitochondrial activities, which impaired DNA and perturbed redox status. Aging increases ROS production and enhances mutations in mtDNA. Conversely, the accumulation of mtDNA mutations may accelerate mammalian aging process. Aging enhances the activity of mtPTP and the release of proapoptotic proteins, including cytochrome c, procaspases-2 and -3, as well as other apoptosis-initiating factors from the mitochondrial intermembrane space[59,60]. Release of proapoptotic proteins induces apoptosis in aging liver by triggering the intrinsic pathway. For the pro-apoptotic and anti-apoptotic proteins in the mitochondria, aging diminishes the levels of pro-apoptotic proteins, such as Bak, whereas the anti-apoptotic proteins are not affected[61]. Thus, the ratio of Bax/Bcl-2 increases and further induces apoptosis. Mitochondrial dysfunction increases apoptosis extent during liver aging and aggravates liver damage.
During aging, the accumulation of diverse deleterious changes impairs liver functions of retaining homeostasis[62]. Cleaning ability of the liver diminishes with aging, which triggers the accumulation of various deleterious materials, such as iron and sphingolipids. The deposition of iron, a result of the aging process, leads to iron excess, thereby increasing the concentration of reactive oxygen and nitrogen species, and causes the toxicity of superoxide and perturbation of the antioxidant capacity of NO[63,64]. In senescent liver mitochondria, an accumulation of non-heme iron enhances the opening of mtPTP, which changes membrane permeability and even causes the release of diverse signaling transduction molecules that eventually induce mitochondrial dysfunction and oxidative damage[65].
Sphingolipids consisting of ceramide and sphingosine accumulate during liver aging, and their metabolism is influenced by oxidative stress, which increases the risk of progression of age-related hepatic diseases[66,67]. The elevated activation of sphingomyelin synthase and the diminished sphingomyelinase activity disrupt the balance of sphingomyelin, thereby resulting in its accumulation; apoptosis and relevant damage occur in aging liver[68]. In addition, the changes incurred in ceramide species are potential risk factors that are implicated in the development and progression of age-related diseases. Six ceramide synthase (CerS) isoforms participate in the synthesis of ceramide species via the de novo pathway and salvage pathway[69]. Furthermore, ceramide is regarded as a crucial component in sphingolipid biosynthesis and degradation[70,71]. The different distributions of CerS in various tissues lead to the difference in ceramide species among tissues[72]. In Wistar rats with age-related obesity, although the levels of total ceramide contents in epidydimal white adipose tissue showed no increase, levels of C16 ceramide produced by CerS6 were increased, which resulted in age-associated adipose tissue hypertrophy and was correlated with insulin resistance[73]. Turpin et al[74] reported that the CerS6-deficient mice with a high-fat diet exhibited reduced C16 ceramide in white adipose tissue, and the CerS6-deficient mice not only had reduced body weight and adipocyte size, but also reduced serum insulin concentrations, improved glucose tolerance and insulin sensitivity compared to control littermates. Therefore, the increased levels of CerS6-derived C16 ceramide attribute to age-related obesity and insulin resistance[75].
A defect in apoptosis disrupts antiapoptotic and proapoptotic homeostasis and gradually causes severe organ dysfunction. As a part of cysteine protease family, caspase-2 participates in apoptosis and can be activated by signals relative to oxidative stress. In mammalian liver aging, the liver with caspase-2 deficiency possesses increased content of oxidized proteins compared with the wild-type liver, which suggests that the activity of eliminating damaged cells is impaired. In addition, caspase-2 deficiency may incur apoptosis by affecting the executioner caspase-3 and then inducing apoptosis disorder[76]. Here we summarize the effects of apoptosis on liver aging systematically in Figure 2.
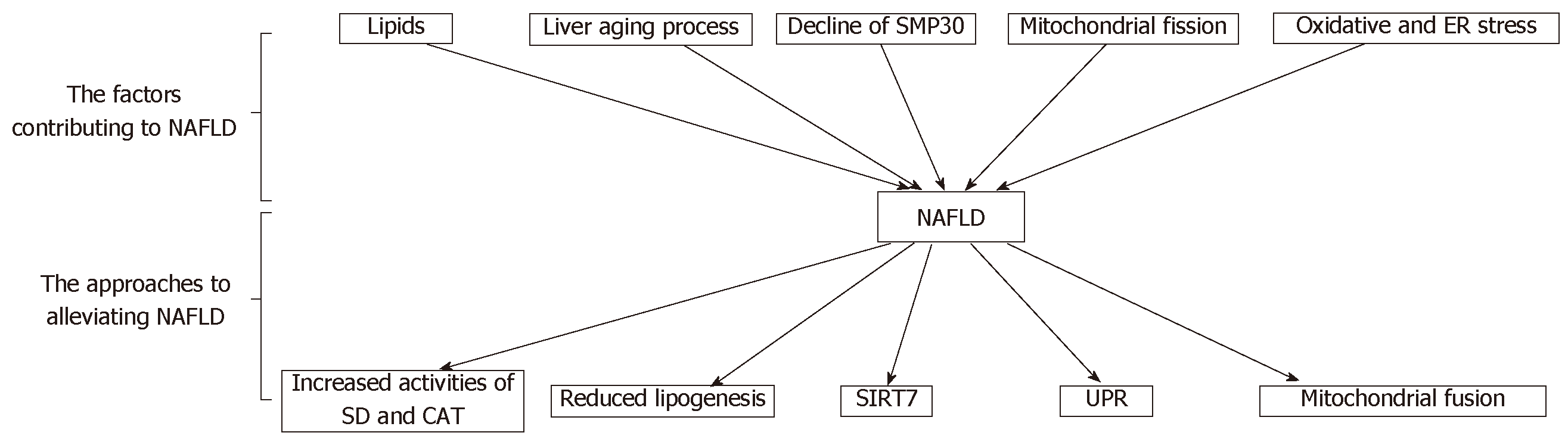
Excessive lipids may transfer from saturated white adipose tissue to non-adipose tissues, such as the liver, and enter non-oxidative pathways where the toxic reactive lipid species are produced. Lipotoxicity, which is induced by reactive lipids, can eventually lead to apoptosis in the liver[77]. NAFLD, which is characterized by significant accumulation of lipids, such as triglycerides, free fatty acids, cholesterol, and phospholipids, is considered the most common chronic liver disorder[78,79] (Figure 3). NAFLD consists of a wide spectrum of liver diseases from benign hepatic steatosis to non-alcoholic steatohepatitis (NASH), advanced fibrosis, cirrhosis, and even hepatocellular carcinoma[80,81].
Aging process upregulates the sensibility of cells to lipotoxicity and represses the metabolic ability concerning lipids, which causes considerable lipotoxicity and increases apoptosis in aging liver[82]. Herein, the prevalence of NAFLD increases in proportion to age[83]. The accumulation of lipotoxicity accelerates apoptosis and liver aging process, and aging increases the severity of lipotoxic damage, thereby forming a vicious circle if prolonged. In NAFLD, the loss of Ca2+ pumping activity induces not only lipotoxicity but also oxidative stress and apoptosis in aging liver through the reduction of senescence marker protein-30 (SMP30). With oxidative and ER stresses, the decline of SMP30 induces inflammatory responses and hepatic steatosis[84]. In addition, NAFLD can evolve into NASH in the presence of oxidative stress, and aging itself enhances this process[85,86]. The occurrence of NASH is relevant to mitochondrial fusion and fission. A high-fat diet and excess glucose can increase Fis1 expression and reduce the levels of Mfn2[87]. Increased Fis1 and reduced Mfn2 interfere with mitochondrial dynamics, thereby causing mitochondrial fission, which in turn induces mitochondrial fragmentation and inhibits mitochondrial fusion[49]. The mitochondrial fragmentation is associated with increased ROS production and inflammation[88,89]. Thus in aging liver, lipotoxicity, SMP30, mitochondrial fission, and oxidative stress may contribute to apoptosis and progression of NAFLD.
Given the crucial role of apoptosis in NAFLD, alleviating apoptosis as a modulatory method may provide curable and innovational strategies to treat NAFLD. The main sources of ROS production and oxidative stress come from mitochondria that participate in the progression of NAFLD[90]. Impaired mitochondria lead to the peroxidation of lipids and induce cell apoptosis known as “lipoapoptosis”. Therefore, mitigation of mitochondrial impairment impedes the progression of NAFLD[91]. Resveratrol ameliorates NAFLD through significantly increasing SOD and CAT activities and decreasing TNF-α, lipid peroxidation, and apoptotic cell contents[92]. Ginkgolide A reduces cellular lipogenesis and lipid accumulation by decreasing mitochondrial oxidative stress and inducing lipoapoptosis to alleviate NAFLD[93]. Lipotoxicity, a complex process, is tightly associated with ER stress. During aging, activated ER stress is associated with fat accumulation, insulin resistance, and apoptosis in NAFLD[16]. Hence, alleviating ER stress is an effective approach to treat NAFLD[94]. In NAFLD, the unfolded protein response (UPR) perturbs hepatic lipogenesis and metabolism and contributes to the progression of NASH. SIRT7 activation can regulate the UPR pathways to suppress ER stress and alleviate and even revert NAFLD[95]. Caspase-3 activation and the imbalance between pro-apoptotic and anti-apoptotic proteins in Bcl-2 family result in liver apoptosis in NAFLD or NASH[96]. Garcimartin et al[97] investigated the effects of silicon on senescent rats with NASH and found that the treatment of silicon can block apoptosis by lowering activated caspase-3 and -9 and the mitochondrial ratio of Bax to Bcl-2 efficiently. Mitochondrial fission may increase the severity of NASH. Conversely, mitochondrial fusion is deemed to ameliorate NASH. Sacerdoti et al[98] reported that induction of heme oxygenase 1 (HO-1) can reduce steatosis and inflammation in NASH by improving mitochondrial fusion. Mitochondrial fusion contributes to mitochondrial elongation, which not only increases the capacity for mitochondrial ATP synthesis, but also reduces oxidative stress, restores insulin sensitivity, and decreases lipogenesis[99,100]. Thus, hepatic mitochondrial fusion, induced by HO-1, is beneficial in reducing the severity of NASH.
During sustained liver damage, liver fibrosis results from the production and degradation imbalance of extracellular matrix (ECM). Once fibrogenesis exceeds fibrolysis, ECM deposits and leads to liver fibrosis. Indeed, with excessive ECM, liver fibrosis is the outcome of chronic hepatic insults, such as NASH and viral hepatitis[101]. In hepatic fibrosis development, activation of hepatic stellate cells (HSCs) and other myofibroblastic cells is the major mechanism in fibrogenesis. Hepatocytes demonstrate significantly impaired regeneration and are then replaced by ECM when exposed to chronic injury[102]. Thus, the activation of HSCs and hepatocyte apoptosis participate in the occurrence of liver fibrosis[76].
Efficacious therapies targeting liver fibrosis rely on the induction of HSC and myofibroblastic cell senescence and apoptosis[103]. CR is involved in preventing age-related liver fibrosis through decreasing the levels of proinflammatory cytokines. The senescence of HSCs can be induced by interleukin (IL)-22 through expressing both IL-10 receptor 2 and IL-22 receptor 1, thereby ameliorating liver fibrosis[104]. Te-tramethylpyrazine can suppress the activation of HSCs and promote HSC senescence via increasing the expression of p53 and silencing Yes-associated protein, which is a therapeutic for liver fibrosis[105]. As a key participant in liver fibrosis, hepatic myofibroblast (MFB) is a target for atorvastatin; hepatic fibrosis is attenuated by induction of hepatic MFB senescence[106]. However, compared with HSC senescence, whole liver aging is a risk factor for and increases the severity of liver fibrosis[107]. The ability of fibrolysis is gradually impaired in liver aging[108]. Mitogen-activated protein kinases (MAPKs), including p38-MAPK, c-Jun N-terminal kinase (JNK), and extracellular signal-regulated kinase, participate in the activation of HSCs via transforming growth factor β1 (TGF-β1), which is closely associated with the development of liver fibrosis[109,110]. Horrillo et al[111] studied the effects of alterations in CR on liver fibrosis in aged Wistar rats. They reported that CR could lower levels of p38-MAPK, JNK, and nuclear factor kappa B to ameliorate liver fibrosis in the elderly. Park et al[112] utilized daumone to mimic CR and found that it effectively inhibited hepatic fibrosis by reducing TGF-β1 in aged mice. In addition, CR can ameliorate the aging related increase in HSC number and reduce the gene expression of α1-(I) collagen in old mice, thereby halting hepatic fibrosis and ECM accumulation[113]. Thus, the induction of HSC and MFB senescence, and the inhibition of MAPK signaling pathways by CR can be therapeutic strategies for age-related liver fibrosis.
From a histological perspective, cirrhosis is structured by regenerative nodules that are encircled by fibrous bands and is regarded as an advanced stage of liver fibrosis[114]. For some patients, NASH and hepatitis C virus are two risk factors for cirrhosis[115,116]. The initial clinical manifestations of cirrhosis are hepatic vasculature disorders, such as portal hypertension, and terminal cirrhosis is characterized by serious complications like hepatic encephalopathy[117].
Telomeres are repeating hexanucleotide sequences and can maintain the stability of chromosomes by avoiding chromosomal end-end fusion. During liver aging, a commensurate loss of the length of telomeres occurs with the progress of aging[118]. Wiemann et al[119] found that telomeres in cirrhosis shorten more significantly than in non-cirrhosis samples. Particularly, in liver cirrhosis, telomere shortening is more evident in hepatocytes than in stellate cells, and the senescence and telomere shortening of hepatocytes are tightly associated with the progression from fibrosis to cirrhosis. At cirrhosis stage, telomere shortening restricts hepatocyte renewing capacity by triggering the p53/p21 pathway that elevates hepatocytes apoptosis, thereby accelerating the development and progression of cirrhosis[120,121]. Furthermore, ER stress involves the formation of cirrhosis. ER stress-related proteins, including inositol-requiring enzyme 1 and C/EBP homologous protein, are activated and induce apoptosis in cirrhosis[122].
The progression from cirrhosis to hepatocellular carcinoma is a complicated and long-term process whose mechanism is not yet clear but may closely involve the relationship between cell apoptosis and cirrhosis[123]. Xu et al[124] discovered that in diethylnitrosamine-induced rat liver cirrhosis, hepatic oval cells are activated and proliferate under the stimulation of hepatocyte apoptosis, which may be the major driver in the evolvement from cirrhosis to hepatocellular carcinoma.
Carcinogenesis is inseparable from apoptosis and cellular senescence. Apoptosis and senescence are generally two beneficial mechanisms to suppress cancer progression but may be reversed to a detrimental one at a later stage of cancer[125]. After age 40, the occurrence of hepatocellular carcinoma increases gradually with age but decreases at around ages of 70–75 years[126]. In aging liver mostly, apoptosis is characterized by perturbation and imbalance in regulation. Thus, maintaining the stability of hepatocyte number and preserving liver functions as before is very difficult. The continuation of this process further decreases apoptosis gradually and increases the incidence of liver cancer. Apoptosis itself can eliminate abnormal cells in the liver. If apoptosis is excessively suppressed and abnormal liver cells cannot be eliminated timely, these abnormal cells may become cancerous and eventually lead to liver cancer[33]. The agonists of the peroxisome proliferator activated receptor-alpha (PPARα), such as peroxisome proliferators, can suppress hepatocyte apoptosis[127]. Through downregulating the expression of Bax mRNA and Fas mRNA and decreasing the level of caspase-2, activated PPARα suppresses hepatic apoptosis, which may promote the generation of liver cancer[128].
Given the central role of aging and apoptosis in tumorigenesis, both apoptosis and aging can become targets in response to liver cancer, which provides a novel perspective for future treatment of liver cancer. p53, a tumor suppression gene, triggers apoptosis and cellular senescence by restricting oncogenes, thereby clearing transformed cells[129]. Xue et al[130] disclosed that the reactivation of p53 gene in liver cancer causes an inhibitory effect on tumors and triggers cell senescence to achieve this inhibitory effect, which is related to upregulating inflammatory cytokines. Furthermore, p53 can induce innate immune response to eliminate tumor cells[130]. Apoptosis is usually at a low level in tumors. Thus, increasing apoptosis of tumor cells is an efficient strategy for a number of anti-tumor drugs. As a non-steroidal anti-inflammatory drug, aspirin in hepatocellular carcinoma cells increases Bax/Bcl-2 ratio, releases cytochrome c, and activates caspase-3, -8, and -9 activities, thereby inhibiting tumor proliferation[131]. Doxorubicin also shows an anti-cancer effect; it can provide highly effective synergy and induce apoptosis when combined with aspirin by increasing the activities of caspase-3, -8, and -9 in human hepatocellular carcinoma cells, which is a novel method to inhibit tumor growth[132].
The liver is an irreplaceable organ with a series of functions, including protein synthesis and detoxification, and its functions and state are critical to human health from a long-term perspective. Liver aging is a natural and spontaneous process with physiological function declines and morphological changes[1,2]. Intrinsic and extrinsic pathways are two primary mechanisms involved in apoptosis and may achieve synergistic effects under some cases[13]. In liver senescence, apoptosis is likened to a double-edged sword: excessive apoptosis causes liver cell loss that can easily lead to liver failure, whereas insufficient apoptosis can lead to the accumulation of abnormal cells, which may conduce to the generation of malignant cells[133].
During liver aging, the overall liver function declines gradually with age. This process may lead to excessive hepatocyte apoptosis, which in turn leads to accumulation of ECM and gradual formation of hepatic fibrosis[76]. Apoptosis and aging play a central role in the occurrence, development, and treatment of age-related liver diseases. Therefore, understanding the role of apoptosis in these diseases will have far-reaching and significant implications for the complete treatment of these diseases in the future. It is vital to explore more accurate methods of detecting apoptosis in the liver. Classic diagnosis of liver damage relies on the histological evaluation from biopsy samples. So, some more accurate noninvasive evaluations remain to be explored for examining cell apoptosis. Many studies above have identified that an age-related increase in inflammation and cellular stress correlates with numerous apoptosis-related genes. Adjusting the expression of apoptosis-related genes to prevent or delay liver disease progression is still challenging. Exploring apoptotic genes further will provide far more valuable insights into apoptosis and better strategies to reduce the morbidity of liver diseases. Therefore, additional scientific research on apoptosis and liver aging needs to be commenced in order to explore potential mechanisms and provide effective countermeasures for treating age-related liver diseases.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cheng TH, Demonacos C, Gassler N, Sugimura H S-Editor: Wang JL L-Editor: Wang TQ E-Editor: Wu YXJ
| 1. | Schmucker DL. Age-related changes in liver structure and function: Implications for disease? Exp Gerontol. 2005;40:650-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 296] [Cited by in RCA: 292] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 2. | Anantharaju A, Feller A, Chedid A. Aging Liver. A review. Gerontology. 2002;48:343-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 139] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 3. | Höhn A, Grune T. Lipofuscin: formation, effects and role of macroautophagy. Redox Biol. 2013;1:140-144. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 179] [Cited by in RCA: 209] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 4. | Wahid B, Ali A, Rafique S, Saleem K, Waqar M, Wasim M, Idrees M. Role of altered immune cells in liver diseases: a review. Gastroenterol Hepatol. 2018;41:377-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Abo T. Extrathymic pathways of T-cell differentiation and immunomodulation. Int Immunopharmacol. 2001;1:1261-1273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Singh P, Coskun ZZ, Goode C, Dean A, Thompson-Snipes L, Darlington G. Lymphoid neogenesis and immune infiltration in aged liver. Hepatology. 2008;47:1680-1690. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 69] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 7. | Singh P, Goode T, Dean A, Awad SS, Darlington GJ. Elevated interferon gamma signaling contributes to impaired regeneration in the aged liver. J Gerontol A Biol Sci Med Sci. 2011;66:944-956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 8. | Kovacs EJ, Palmer JL, Fortin CF, Fülöp T, Goldstein DR, Linton PJ. Aging and innate immunity in the mouse: impact of intrinsic and extrinsic factors. Trends Immunol. 2009;30:319-324. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 137] [Cited by in RCA: 124] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 9. | Weinberger B, Herndler-Brandstetter D, Schwanninger A, Weiskopf D, Grubeck-Loebenstein B. Biology of immune responses to vaccines in elderly persons. Clin Infect Dis. 2008;46:1078-1084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 273] [Cited by in RCA: 284] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 10. | Prelog M. Aging of the immune system: a risk factor for autoimmunity? Autoimmun Rev. 2006;5:136-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 147] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 11. | Navarro A, Boveris A. The mitochondrial energy transduction system and the aging process. Am J Physiol Cell Physiol. 2007;292:C670-C686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 479] [Cited by in RCA: 493] [Article Influence: 25.9] [Reference Citation Analysis (0)] |
| 12. | Busuttil RA, Dollé M, Campisi J, Vijga J. Genomic instability, aging, and cellular senescence. Ann N Y Acad Sci. 2004;1019:245-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Hengartner MO. The biochemistry of apoptosis. Nature. 2000;407:770-776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5259] [Cited by in RCA: 5202] [Article Influence: 208.1] [Reference Citation Analysis (0)] |
| 14. | Joaquin AM, Gollapudi S. Functional decline in aging and disease: a role for apoptosis. J Am Geriatr Soc. 2001;49:1234-1240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 59] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 15. | Salminen A, Kaarniranta K. ER stress and hormetic regulation of the aging process. Ageing Res Rev. 2010;9:211-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 94] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 16. | Fu S, Watkins SM, Hotamisligil GS. The role of endoplasmic reticulum in hepatic lipid homeostasis and stress signaling. Cell Metab. 2012;15:623-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 403] [Cited by in RCA: 448] [Article Influence: 34.5] [Reference Citation Analysis (0)] |
| 17. | Zhong HH, Hu SJ, Yu B, Jiang SS, Zhang J, Luo D, Yang MW, Su WY, Shao YL, Deng HL, Hong FF, Yang SL. Apoptosis in the aging liver. Oncotarget. 2017;8:102640-102652. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 18. | Yin XM, Ding WX. Death receptor activation-induced hepatocyte apoptosis and liver injury. Curr Mol Med. 2003;3:491-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 115] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 19. | Elmore S. Apoptosis: a review of programmed cell death. Toxicol Pathol. 2007;35:495-516. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10243] [Cited by in RCA: 9584] [Article Influence: 532.4] [Reference Citation Analysis (0)] |
| 20. | Pennarun B, Meijer A, de Vries EG, Kleibeuker JH, Kruyt F, de Jong S. Playing the DISC: turning on TRAIL death receptor-mediated apoptosis in cancer. Biochim Biophys Acta. 2010;1805:123-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 70] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 21. | Cao L, Quan XB, Zeng WJ, Yang XO, Wang MJ. Mechanism of Hepatocyte Apoptosis. J Cell Death. 2016;9:19-29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 80] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 22. | Feldstein AE, Gores GJ. Apoptosis in alcoholic and nonalcoholic steatohepatitis. Front Biosci. 2005;10:3093-3099. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 143] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 23. | Battaglia V, Compagnone A, Bandino A, Bragadin M, Rossi CA, Zanetti F, Colombatto S, Grillo MA, Toninello A. Cobalt induces oxidative stress in isolated liver mitochondria responsible for permeability transition and intrinsic apoptosis in hepatocyte primary cultures. Int J Biochem Cell Biol. 2009;41:586-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 78] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 24. | Riedl SJ, Shi Y. Molecular mechanisms of caspase regulation during apoptosis. Nat Rev Mol Cell Biol. 2004;5:897-907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1330] [Cited by in RCA: 1407] [Article Influence: 67.0] [Reference Citation Analysis (0)] |
| 25. | Stoka V, Turk V, Bredesen DE. Differential regulation of the intrinsic pathway of apoptosis in brain and liver during ageing. FEBS Lett. 2006;580:3739-3745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 26. | Ujjan JA. Association between aging, apoptosis and related dysregulations. Int J Sci Eng Res. 2014;5:300-309. |
| 27. | Brunelle JK, Letai A. Control of mitochondrial apoptosis by the Bcl-2 family. J Cell Sci. 2009;122:437-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 628] [Cited by in RCA: 705] [Article Influence: 44.1] [Reference Citation Analysis (0)] |
| 28. | Estaquier J, Vallette F, Vayssiere JL, Mignotte B. The mitochondrial pathways of apoptosis. Adv Exp Med Biol. 2012;942:157-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 362] [Cited by in RCA: 462] [Article Influence: 35.5] [Reference Citation Analysis (0)] |
| 29. | Zorov DB, Juhaszova M, Sollott SJ. Mitochondrial reactive oxygen species (ROS) and ROS-induced ROS release. Physiol Rev. 2014;94:909-950. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2139] [Cited by in RCA: 3812] [Article Influence: 346.5] [Reference Citation Analysis (0)] |
| 30. | Czaja MJ. Induction and regulation of hepatocyte apoptosis by oxidative stress. Antioxid Redox Signal. 2002;4:759-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 87] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 31. | Sastre J, Pallardó FV, Viña J. Mitochondrial oxidative stress plays a key role in aging and apoptosis. IUBMB Life. 2000;49:427-435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 253] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 32. | Molpeceres V, Mauriz JL, García-Mediavilla MV, González P, Barrio JP, González-Gallego J. Melatonin is able to reduce the apoptotic liver changes induced by aging via inhibition of the intrinsic pathway of apoptosis. J Gerontol A Biol Sci Med Sci. 2007;62:687-695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 53] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 33. | Camplejohn RS, Gilchrist R, Easton D, McKenzie-Edwards E, Barnes DM, Eccles DM, Ardern-Jones A, Hodgson SV, Duddy PM, Eeles RA. Apoptosis, ageing and cancer susceptibility. Br J Cancer. 2003;88:487-490. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 34. | Timchenko NA. Aging and liver regeneration. Trends Endocrinol Metab. 2009;20:171-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 163] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 35. | Giorgadze S, Gujabidze N, Tevzadze N, Rukhadze R. Apoptosis and proliferative activity of hepatocytes of white rats during aging. Georgian Med News. 2009;88-91. [PubMed] |
| 36. | Harman D. Aging: a theory based on free radical and radiation chemistry. J Gerontol. 1956;11:298-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5844] [Cited by in RCA: 5426] [Article Influence: 78.6] [Reference Citation Analysis (0)] |
| 37. | Lee HC, Wei YH. Oxidative stress, mitochondrial DNA mutation, and apoptosis in aging. Exp Biol Med (Maywood). 2007;232:592-606. [PubMed] |
| 38. | Martin H, Uring-Lambert B, Adrian M, Lahlou A, Bonet A, Demougeot C, Devaux S, Laurant P, Richert L, Berthelot A. Effects of long-term dietary intake of magnesium on oxidative stress, apoptosis and ageing in rat liver. Magnes Res. 2008;21:124-130. [PubMed] |
| 39. | Zhou YY, Ji XF, Fu JP, Zhu XJ, Li RH, Mu CK, Wang CL, Song WW. Gene Transcriptional and Metabolic Profile Changes in Mimetic Aging Mice Induced by D-Galactose. PLoS One. 2015;10:e0132088. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 40] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 40. | Yoo DY, Kim W, Kim IH, Nam SM, Chung JY, Choi JH, Yoon YS, Won MH, Hwang IK. Combination effects of sodium butyrate and pyridoxine treatment on cell proliferation and neuroblast differentiation in the dentate gyrus of D-galactose-induced aging model mice. Neurochem Res. 2012;37:223-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 41. | Wang D, Liu M, Cao J, Cheng Y, Zhuo C, Xu H, Tian S, Zhang Y, Zhang J, Wang F. Effect of Colla corii asini (E'jiao) on D-galactose induced aging mice. Biol Pharm Bull. 2012;35:2128-2132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 42. | Zhu SY, Dong Y, Tu J, Zhou Y, Zhou XH, Xu B. Silybum marianum oil attenuates oxidative stress and ameliorates mitochondrial dysfunction in mice treated with D-galactose. Pharmacogn Mag. 2014;10:S92-S99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 43. | Xu LQ, Xie YL, Gui SH, Zhang X, Mo ZZ, Sun CY, Li CL, Luo DD, Zhang ZB, Su ZR, Xie JH. Polydatin attenuates d-galactose-induced liver and brain damage through its anti-oxidative, anti-inflammatory and anti-apoptotic effects in mice. Food Funct. 2016;7:4545-4555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 112] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 44. | López-Lluch G, Navas P. Calorie restriction as an intervention in ageing. J Physiol. 2016;594:2043-2060. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 201] [Cited by in RCA: 191] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 45. | Gredilla R, Barja G, López-Torres M. Effect of short-term caloric restriction on H2O2 production and oxidative DNA damage in rat liver mitochondria and location of the free radical source. J Bioenerg Biomembr. 2001;33:279-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 112] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 46. | Higami Y, Shimokawa I, Tomita M, Okimoto T, Koji T, Kobayashi N, Ikeda T. Aging accelerates but life-long dietary restriction suppresses apoptosis-related Fas expression on hepatocytes. Am J Pathol. 1997;151:659-663. [PubMed] |
| 47. | Ando K, Higami Y, Tsuchiya T, Kanematsu T, Shimokawa I. Impact of aging and life-long calorie restriction on expression of apoptosis-related genes in male F344 rat liver. Microsc Res Tech. 2002;59:293-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 48. | Ikeyama S, Wang XT, Li J, Podlutsky A, Martindale JL, Kokkonen G, van Huizen R, Gorospe M, Holbrook NJ. Expression of the pro-apoptotic gene gadd153/chop is elevated in liver with aging and sensitizes cells to oxidant injury. J Biol Chem. 2003;278:16726-16731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 64] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 49. | Meyer JN, Leuthner TC, Luz AL. Mitochondrial fusion, fission, and mitochondrial toxicity. Toxicology. 2017;391:42-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 340] [Cited by in RCA: 385] [Article Influence: 48.1] [Reference Citation Analysis (0)] |
| 50. | Pernas L, Scorrano L. Mito-Morphosis: Mitochondrial Fusion, Fission, and Cristae Remodeling as Key Mediators of Cellular Function. Annu Rev Physiol. 2016;78:505-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 398] [Cited by in RCA: 578] [Article Influence: 57.8] [Reference Citation Analysis (0)] |
| 51. | Khraiwesh H, López-Domínguez JA, Fernández del Río L, Gutierrez-Casado E, López-Lluch G, Navas P, de Cabo R, Ramsey JJ, Burón MI, Villalba JM, González-Reyes JA. Mitochondrial ultrastructure and markers of dynamics in hepatocytes from aged, calorie restricted mice fed with different dietary fats. Exp Gerontol. 2014;56:77-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 52. | Scheckhuber CQ. Impact of mitochondrial dynamics on organismic aging. ScientificWorldJournal. 2009;9:250-254. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 53. | Kowald A, Kirkwood TB. Evolution of the mitochondrial fusion-fission cycle and its role in aging. Proc Natl Acad Sci U S A. 2011;108:10237-10242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 104] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 54. | Lee YJ, Jeong SY, Karbowski M, Smith CL, Youle RJ. Roles of the mammalian mitochondrial fission and fusion mediators Fis1, Drp1, and Opa1 in apoptosis. Mol Biol Cell. 2004;15:5001-5011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 768] [Cited by in RCA: 853] [Article Influence: 40.6] [Reference Citation Analysis (0)] |
| 55. | Mai S, Klinkenberg M, Auburger G, Bereiter-Hahn J, Jendrach M. Decreased expression of Drp1 and Fis1 mediates mitochondrial elongation in senescent cells and enhances resistance to oxidative stress through PINK1. J Cell Sci. 2010;123:917-926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 202] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 56. | Zhang Y, Chong E, Herman B. Age-associated increases in the activity of multiple caspases in Fisher 344 rat organs. Exp Gerontol. 2002;37:777-789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 51] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 57. | Kam PC, Ferch NI. Apoptosis: mechanisms and clinical implications. Anaesthesia. 2000;55:1081-1093. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 133] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 58. | Braidy N, Guillemin GJ, Mansour H, Chan-Ling T, Poljak A, Grant R. Age related changes in NAD+ metabolism oxidative stress and Sirt1 activity in wistar rats. PLoS One. 2011;6:e19194. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 495] [Cited by in RCA: 477] [Article Influence: 34.1] [Reference Citation Analysis (0)] |
| 59. | Mather M, Rottenberg H. Aging enhances the activation of the permeability transition pore in mitochondria. Biochem Biophys Res Commun. 2000;273:603-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 93] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 60. | Kokoszka JE, Coskun P, Esposito LA, Wallace DC. Increased mitochondrial oxidative stress in the Sod2 (+/-) mouse results in the age-related decline of mitochondrial function culminating in increased apoptosis. Proc Natl Acad Sci U S A. 2001;98:2278-2283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 338] [Cited by in RCA: 354] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 61. | Mach J, Huizer-Pajkos A, Kane A, Jones B, McKenzie C, Mitchell SJ, de Cabo R, Cogger VC, Le Couteur DG, Hilmer SN. The effect of aging on mitochondrial and cytosolic hepatic intrinsic death pathway and apoptosis associated proteins in Fischer 344 rats. Exp Gerontol. 2015;67:54-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 62. | Harman D. Aging: overview. Ann N Y Acad Sci. 2001;928:1-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 285] [Cited by in RCA: 305] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 63. | Puntarulo S. Iron, oxidative stress and human health. Mol Aspects Med. 2005;26:299-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 247] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 64. | Killilea DW, Wong SL, Cahaya HS, Atamna H, Ames BN. Iron accumulation during cellular senescence. Ann N Y Acad Sci. 2004;1019:365-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 70] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 65. | Seo AY, Xu J, Servais S, Hofer T, Marzetti E, Wohlgemuth SE, Knutson MD, Chung HY, Leeuwenburgh C. Mitochondrial iron accumulation with age and functional consequences. Aging Cell. 2008;7:706-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 92] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 66. | Cutler RG, Mattson MP. Sphingomyelin and ceramide as regulators of development and lifespan. Mech Ageing Dev. 2001;122:895-908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 128] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 67. | Lightle SA, Oakley JI, Nikolova-Karakashian MN. Activation of sphingolipid turnover and chronic generation of ceramide and sphingosine in liver during aging. Mech Ageing Dev. 2000;120:111-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 89] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 68. | Sacket SJ, Chung HY, Okajima F, Im DS. Increase in sphingolipid catabolic enzyme activity during aging. Acta Pharmacol Sin. 2009;30:1454-1461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 51] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 69. | Pewzner-Jung Y, Park H, Laviad EL, Silva LC, Lahiri S, Stiban J, Erez-Roman R, Brügger B, Sachsenheimer T, Wieland F, Prieto M, Merrill AH, Futerman AH. A critical role for ceramide synthase 2 in liver homeostasis: I. alterations in lipid metabolic pathways. J Biol Chem. 2010;285:10902-10910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 213] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 70. | Saddoughi SA, Song P, Ogretmen B. Roles of bioactive sphingolipids in cancer biology and therapeutics. Subcell Biochem. 2008;49:413-440. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 190] [Cited by in RCA: 182] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 71. | Hannun YA, Obeid LM. Many ceramides. J Biol Chem. 2011;286:27855-27862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 417] [Cited by in RCA: 478] [Article Influence: 34.1] [Reference Citation Analysis (0)] |
| 72. | Stiban J, Tidhar R, Futerman AH. Ceramide synthases: roles in cell physiology and signaling. Adv Exp Med Biol. 2010;688:60-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 130] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 73. | Bonzón-Kulichenko E, Moltó E, Pintado C, Fernández A, Arribas C, Schwudke D, Gallardo N, Shevchenko A, Andrés A. Changes in Visceral Adipose Tissue Plasma Membrane Lipid Composition in Old Rats Are Associated With Adipocyte Hypertrophy With Aging. J Gerontol A Biol Sci Med Sci. 2018;73:1139-1146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 74. | Turpin SM, Nicholls HT, Willmes DM, Mourier A, Brodesser S, Wunderlich CM, Mauer J, Xu E, Hammerschmidt P, Brönneke HS, Trifunovic A, LoSasso G, Wunderlich FT, Kornfeld JW, Blüher M, Krönke M, Brüning JC. Obesity-induced CerS6-dependent C16:0 ceramide production promotes weight gain and glucose intolerance. Cell Metab. 2014;20:678-686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 441] [Cited by in RCA: 544] [Article Influence: 49.5] [Reference Citation Analysis (0)] |
| 75. | Błachnio-Zabielska AU, Baranowski M, Hirnle T, Zabielski P, Lewczuk A, Dmitruk I, Górski J. Increased bioactive lipids content in human subcutaneous and epicardial fat tissue correlates with insulin resistance. Lipids. 2012;47:1131-1141. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 51] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 76. | Zhang Y, Zhang QQ, Guo XH, Zhang HY, Liu LX. IGFBPrP1 induces liver fibrosis by inducing hepatic stellate cell activation and hepatocyte apoptosis via Smad2/3 signaling. World J Gastroenterol. 2014;20:6523-6533. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 18] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 77. | Slawik M, Vidal-Puig AJ. Lipotoxicity, overnutrition and energy metabolism in aging. Ageing Res Rev. 2006;5:144-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 179] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 78. | Li L, Li L, Chen L, Lin X, Xu Y, Ren J, Fu J, Qiu Y. Effect of oleoylethanolamide on diet-induced nonalcoholic fatty liver in rats. J Pharmacol Sci. 2015;127:244-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 51] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 79. | Abd El-Kader SM, El-Den Ashmawy EM. Non-alcoholic fatty liver disease: The diagnosis and management. World J Hepatol. 2015;7:846-858. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 233] [Cited by in RCA: 267] [Article Influence: 26.7] [Reference Citation Analysis (5)] |
| 80. | Sass DA, Chang P, Chopra KB. Nonalcoholic fatty liver disease: a clinical review. Dig Dis Sci. 2005;50:171-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 176] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 81. | Falck-Ytter Y, Younossi ZM, Marchesini G, McCullough AJ. Clinical features and natural history of nonalcoholic steatosis syndromes. Semin Liver Dis. 2001;21:17-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 426] [Cited by in RCA: 402] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 82. | Gong Z, Tas E, Yakar S, Muzumdar R. Hepatic lipid metabolism and non-alcoholic fatty liver disease in aging. Mol Cell Endocrinol. 2017;455:115-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 99] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 83. | Fan JG, Zhu J, Li XJ, Chen L, Li L, Dai F, Li F, Chen SY. Prevalence of and risk factors for fatty liver in a general population of Shanghai, China. J Hepatol. 2005;43:508-514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 304] [Cited by in RCA: 293] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 84. | Kondo Y, Ishigami A. Involvement of senescence marker protein-30 in glucose metabolism disorder and non-alcoholic fatty liver disease. Geriatr Gerontol Int. 2016;16 Suppl 1:4-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 85. | Sheedfar F, Di Biase S, Koonen D, Vinciguerra M. Liver diseases and aging: friends or foes? Aging Cell. 2013;12:950-954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 183] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 86. | Bertolotti M, Lonardo A, Mussi C, Baldelli E, Pellegrini E, Ballestri S, Romagnoli D, Loria P. Nonalcoholic fatty liver disease and aging: epidemiology to management. World J Gastroenterol. 2014;20:14185-14204. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 232] [Cited by in RCA: 226] [Article Influence: 20.5] [Reference Citation Analysis (1)] |
| 87. | Satapati S, Kucejova B, Duarte JA, Fletcher JA, Reynolds L, Sunny NE, He T, Nair LA, Livingston KA, Fu X, Merritt ME, Sherry AD, Malloy CR, Shelton JM, Lambert J, Parks EJ, Corbin I, Magnuson MA, Browning JD, Burgess SC. Mitochondrial metabolism mediates oxidative stress and inflammation in fatty liver. J Clin Invest. 2015;125:4447-4462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 315] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 88. | Bach D, Naon D, Pich S, Soriano FX, Vega N, Rieusset J, Laville M, Guillet C, Boirie Y, Wallberg-Henriksson H, Manco M, Calvani M, Castagneto M, Palacín M, Mingrone G, Zierath JR, Vidal H, Zorzano A. Expression of Mfn2, the Charcot-Marie-Tooth neuropathy type 2A gene, in human skeletal muscle: effects of type 2 diabetes, obesity, weight loss, and the regulatory role of tumor necrosis factor alpha and interleukin-6. Diabetes. 2005;54:2685-2693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 297] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 89. | Liesa M, Shirihai OS. Mitochondrial dynamics in the regulation of nutrient utilization and energy expenditure. Cell Metab. 2013;17:491-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 834] [Cited by in RCA: 1040] [Article Influence: 86.7] [Reference Citation Analysis (0)] |
| 90. | Spahis S, Delvin E, Borys JM, Levy E. Oxidative Stress as a Critical Factor in Nonalcoholic Fatty Liver Disease Pathogenesis. Antioxid Redox Signal. 2017;26:519-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 232] [Cited by in RCA: 290] [Article Influence: 36.3] [Reference Citation Analysis (0)] |
| 91. | Ajith TA. Role of mitochondria and mitochondria-targeted agents in non-alcoholic fatty liver disease. Clin Exp Pharmacol Physiol. 2018;45:413-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 44] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 92. | Hajighasem A, Farzanegi P, Mazaheri Z. Effects of combined therapy with resveratrol, continuous and interval exercises on apoptosis, oxidative stress, and inflammatory biomarkers in the liver of old rats with non-alcoholic fatty liver disease. Arch Physiol Biochem. 2018;1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 93. | Jeong HS, Kim KH, Lee IS, Park JY, Kim Y, Kim KS, Jang HJ. Ginkgolide A ameliorates non-alcoholic fatty liver diseases on high fat diet mice. Biomed Pharmacother. 2017;88:625-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 94. | Cao SS, Kaufman RJ. Targeting endoplasmic reticulum stress in metabolic disease. Expert Opin Ther Targets. 2013;17:437-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 119] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 95. | Shin J, He M, Liu Y, Paredes S, Villanova L, Brown K, Qiu X, Nabavi N, Mohrin M, Wojnoonski K, Li P, Cheng HL, Murphy AJ, Valenzuela DM, Luo H, Kapahi P, Krauss R, Mostoslavsky R, Yancopoulos GD, Alt FW, Chua KF, Chen D. SIRT7 represses Myc activity to suppress ER stress and prevent fatty liver disease. Cell Rep. 2013;5:654-665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 227] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 96. | Wang Y, Ausman LM, Russell RM, Greenberg AS, Wang XD. Increased apoptosis in high-fat diet-induced nonalcoholic steatohepatitis in rats is associated with c-Jun NH2-terminal kinase activation and elevated proapoptotic Bax. J Nutr. 2008;138:1866-1871. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 105] [Cited by in RCA: 112] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 97. | Garcimartín A, López-Oliva ME, Sántos-López JA, García-Fernández RA, Macho-González A, Bastida S, Benedí J, Sánchez-Muniz FJ. Silicon Alleviates Nonalcoholic Steatohepatitis by Reducing Apoptosis in Aged Wistar Rats Fed a High-Saturated Fat, High-Cholesterol Diet. J Nutr. 2017;147:1104-1112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 98. | Sacerdoti D, Singh SP, Schragenheim J, Bellner L, Vanella L, Raffaele M, Meissner A, Grant I, Favero G, Rezzani R, Rodella LF, Bamshad D, Lebovics E, Abraham NG. Development of NASH in Obese Mice is Confounded by Adipose Tissue Increase in Inflammatory NOV and Oxidative Stress. Int J Hepatol. 2018;2018:3484107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 99. | Zhao L, Zou X, Feng Z, Luo C, Liu J, Li H, Chang L, Wang H, Li Y, Long J, Gao F, Liu J. Evidence for association of mitochondrial metabolism alteration with lipid accumulation in aging rats. Exp Gerontol. 2014;56:3-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 66] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 100. | Sebastián D, Hernández-Alvarez MI, Segalés J, Sorianello E, Muñoz JP, Sala D, Waget A, Liesa M, Paz JC, Gopalacharyulu P, Orešič M, Pich S, Burcelin R, Palacín M, Zorzano A. Mitofusin 2 (Mfn2) links mitochondrial and endoplasmic reticulum function with insulin signaling and is essential for normal glucose homeostasis. Proc Natl Acad Sci U S A. 2012;109:5523-5528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 434] [Cited by in RCA: 539] [Article Influence: 41.5] [Reference Citation Analysis (0)] |
| 101. | Puche JE, Saiman Y, Friedman SL. Hepatic stellate cells and liver fibrosis. Compr Physiol. 2013;3:1473-1492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 421] [Cited by in RCA: 570] [Article Influence: 51.8] [Reference Citation Analysis (0)] |
| 102. | Bataller R, Brenner DA. Liver fibrosis. J Clin Invest. 2005;115:209-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3381] [Cited by in RCA: 4118] [Article Influence: 205.9] [Reference Citation Analysis (3)] |
| 103. | Krizhanovsky V, Yon M, Dickins RA, Hearn S, Simon J, Miething C, Yee H, Zender L, Lowe SW. Senescence of activated stellate cells limits liver fibrosis. Cell. 2008;134:657-667. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1625] [Cited by in RCA: 1532] [Article Influence: 90.1] [Reference Citation Analysis (0)] |
| 104. | Kong X, Feng D, Wang H, Hong F, Bertola A, Wang FS, Gao B. Interleukin-22 induces hepatic stellate cell senescence and restricts liver fibrosis in mice. Hepatology. 2012;56:1150-1159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 317] [Cited by in RCA: 357] [Article Influence: 27.5] [Reference Citation Analysis (0)] |
| 105. | Jin H, Lian N, Zhang F, Bian M, Chen X, Zhang C, Jia Y, Lu C, Hao M, Yao S, Shao J, Wu L, Chen A, Zheng S. Inhibition of YAP signaling contributes to senescence of hepatic stellate cells induced by tetramethylpyrazine. Eur J Pharm Sci. 2017;96:323-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 106. | Klein S, Klösel J, Schierwagen R, Körner C, Granzow M, Huss S, Mazar IG, Weber S, van den Ven PF, Pieper-Fürst U, Fürst DO, Nattermann J, Lammert F, Sauerbruch T, Trebicka J. Atorvastatin inhibits proliferation and apoptosis, but induces senescence in hepatic myofibroblasts and thereby attenuates hepatic fibrosis in rats. Lab Invest. 2012;92:1440-1450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 81] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 107. | Delire B, Lebrun V, Selvais C, Henriet P, Bertrand A, Horsmans Y, Leclercq IA. Aging enhances liver fibrotic response in mice through hampering extracellular matrix remodeling. Aging (Albany NY). 2016;9:98-113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 108. | Iredale JP, Benyon RC, Pickering J, McCullen M, Northrop M, Pawley S, Hovell C, Arthur MJ. Mechanisms of spontaneous resolution of rat liver fibrosis. Hepatic stellate cell apoptosis and reduced hepatic expression of metalloproteinase inhibitors. J Clin Invest. 1998;102:538-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 785] [Cited by in RCA: 828] [Article Influence: 30.7] [Reference Citation Analysis (0)] |
| 109. | Lee SY, Lee J, Lee H, Kim B, Lew J, Baek N, Kim SH. MicroRNA134 Mediated Upregulation of JNK and Downregulation of NFkB Signalings Are Critically Involved in Dieckol Induced Antihepatic Fibrosis. J Agric Food Chem. 2016;64:5508-5514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 110. | Cheng CF, Pan TM. Ankaflavin and Monascin Induce Apoptosis in Activated Hepatic Stellate Cells through Suppression of the Akt/NF-κB/p38 Signaling Pathway. J Agric Food Chem. 2016;64:9326-9334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 111. | Horrillo D, Gallardo N, Lauzurica N, Barrus MT, San Frutos MG, Andres A, Ros M, Fernandez-Agullo T. Development of liver fibrosis during aging: effects of caloric restriction. J Biol Regul Homeost Agents. 2013;27:377-388. [PubMed] |
| 112. | Park JH, Chung HY, Kim M, Lee JH, Jung M, Ha H. Daumone fed late in life improves survival and reduces hepatic inflammation and fibrosis in mice. Aging Cell. 2014;13:709-718. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 113. | Chen J, King K, Zhang JX. Effect of caloric restriction on hepatic sinusoidal system and stellate cells in mice. J Aging Res. 2014;2014:670890. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 114. | Romanelli RG, Stasi C. Recent Advancements in Diagnosis and Therapy of Liver Cirrhosis. Curr Drug Targets. 2016;17:1804-1817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 70] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 115. | Bellentani S, Pozzato G, Saccoccio G, Crovatto M, Crocè LS, Mazzoran L, Masutti F, Cristianini G, Tiribelli C. Clinical course and risk factors of hepatitis C virus related liver disease in the general population: report from the Dionysos study. Gut. 1999;44:874-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 154] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 116. | Farrell GC, Larter CZ. Nonalcoholic fatty liver disease: from steatosis to cirrhosis. Hepatology. 2006;43:S99-S112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1756] [Cited by in RCA: 1822] [Article Influence: 95.9] [Reference Citation Analysis (0)] |
| 117. | Schuppan D, Afdhal NH. Liver cirrhosis. Lancet. 2008;371:838-851. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1686] [Cited by in RCA: 1565] [Article Influence: 92.1] [Reference Citation Analysis (0)] |
| 118. | Hoare M, Das T, Alexander G. Ageing, telomeres, senescence, and liver injury. J Hepatol. 2010;53:950-961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 132] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 119. | Wiemann SU, Satyanarayana A, Tsahuridu M, Tillmann HL, Zender L, Klempnauer J, Flemming P, Franco S, Blasco MA, Manns MP, Rudolph KL. Hepatocyte telomere shortening and senescence are general markers of human liver cirrhosis. FASEB J. 2002;16:935-942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 374] [Cited by in RCA: 382] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 120. | Wagayama H, Shiraki K, Sugimoto K, Ito T, Fujikawa K, Yamanaka T, Takase K, Nakano T. High expression of p21WAF1/CIP1 is correlated with human hepatocellular carcinoma in patients with hepatitis C virus-associated chronic liver diseases. Hum Pathol. 2002;33:429-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 121. | Wagayama H, Shiraki K, Yamanaka T, Sugimoto K, Ito T, Fujikawa K, Takase K, Nakano T. p21WAF1/CTP1 expression and hepatitis virus type. Dig Dis Sci. 2001;46:2074-2079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 122. | Jiang T, Wang L, Li X, Song J, Wu X, Zhou S. Inositol-requiring enzyme 1-mediated endoplasmic reticulum stress triggers apoptosis and fibrosis formation in liver cirrhosis rat models. Mol Med Rep. 2015;11:2941-2946. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 123. | Fattovich G, Stroffolini T, Zagni I, Donato F. Hepatocellular carcinoma in cirrhosis: incidence and risk factors. Gastroenterology. 2004;127:S35-S50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1691] [Cited by in RCA: 1792] [Article Influence: 85.3] [Reference Citation Analysis (2)] |
| 124. | Xu XM, Yuan GJ, Deng JJ, Wu YG, Ge W, Song QB. Hepatic oval cells activated by hepatocyte apoptosis in diethylnitrosamine-induced rat liver cirrhosis. Saudi Med J. 2010;31:490-494. [PubMed] |
| 125. | Cerella C, Grandjenette C, Dicato M, Diederich M. Roles of Apoptosis and Cellular Senescence in Cancer and Aging. Curr Drug Targets. 2016;17:405-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 126. | El-Serag HB. Hepatocellular carcinoma. N Engl J Med. 2011;365:1118-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2881] [Cited by in RCA: 3088] [Article Influence: 220.6] [Reference Citation Analysis (0)] |
| 127. | Roberts RA, James NH, Hasmall SC, Holden PR, Lambe K, Macdonald N, West D, Woodyatt NJ, Whitcome D. Apoptosis and proliferation in nongenotoxic carcinogenesis: species differences and role of PPARalpha. Toxicol Lett. 2000;112-113:49-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 46] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 128. | Yosef R, Pilpel N, Tokarsky-Amiel R, Biran A, Ovadya Y, Cohen S, Vadai E, Dassa L, Shahar E, Condiotti R, Ben-Porath I, Krizhanovsky V. Directed elimination of senescent cells by inhibition of BCL-W and BCL-XL. Nat Commun. 2016;7:11190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 485] [Cited by in RCA: 703] [Article Influence: 78.1] [Reference Citation Analysis (0)] |
| 129. | Harris SL, Levine AJ. The p53 pathway: positive and negative feedback loops. Oncogene. 2005;24:2899-2908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1399] [Cited by in RCA: 1410] [Article Influence: 70.5] [Reference Citation Analysis (0)] |
| 130. | Xue W, Zender L, Miething C, Dickins RA, Hernando E, Krizhanovsky V, Cordon-Cardo C, Lowe SW. Senescence and tumour clearance is triggered by p53 restoration in murine liver carcinomas. Nature. 2007;445:656-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1709] [Cited by in RCA: 1933] [Article Influence: 107.4] [Reference Citation Analysis (0)] |
| 131. | Hossain MA, Kim DH, Jang JY, Kang YJ, Yoon JH, Moon JO, Chung HY, Kim GY, Choi YH, Copple BL, Kim ND. Aspirin induces apoptosis in vitro and inhibits tumor growth of human hepatocellular carcinoma cells in a nude mouse xenograft model. Int J Oncol. 2012;40:1298-1304. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 80] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 132. | Hossain MA, Kim DH, Jang JY, Kang YJ, Yoon JH, Moon JO, Chung HY, Kim GY, Choi YH, Copple BL, Kim ND. Aspirin enhances doxorubicin-induced apoptosis and reduces tumor growth in human hepatocellular carcinoma cells in vitro and in vivo. Int J Oncol. 2012;40:1636-1642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 133. | Patel T. Apoptosis in hepatic pathophysiology. Clin Liver Dis. 2000;4:295-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 23] [Article Influence: 0.9] [Reference Citation Analysis (0)] |