Published online Dec 26, 2019. doi: 10.12998/wjcc.v7.i24.4270
Peer-review started: September 20, 2019
First decision: October 20, 2019
Revised: November 7, 2019
Accepted: November 15, 2019
Article in press: November 15, 2019
Published online: December 26, 2019
Processing time: 95 Days and 17.7 Hours
Acute appendicitis in a solid organ transplant recipient is a rare occurrence, and experience remains limited. Appendicitis in uterine transplant recipients has never been reported. Immunocompromised patients with acute abdomen often present late and with attenuated symptoms. The differential diagnosis in a transplanted patient is broad and challenging due to possible existing complications associated with the graft, effects of immunosuppression, and altered anatomical relations.
A 26-year-old woman suffering from absolute uterine factor infertility received a uterus transplant. In the post-transplant period, she suffered from leukopenia and recurrent acute cellular rejection. Her compliance was suboptimal. She travelled to an exotic destination despite the physician’s recommendation not to do so. Following her vacation, she presented with abdominal discomfort, nausea and diarrhoea. There was no sign of acute abdomen; the abdominal ultrasound was negative on day 0. Clostridium difficile colitis was verified and treated with perorally administered vancomycin. On day 4, the discomfort changed to pain; the ultrasound scan revealed a finding suggestive of appendicitis. Surgical exploration revealed perforated appendicitis, and appendectomy was performed. From a surgical point of view, the patient’s follow-up was uneventful. The patient underwent a successful embryo transfer 6 months after the appendectomy. The patient gave birth to a healthy boy at the 35th week of gestation.
A high index of suspicion of an atypical course and symptomatology of acute abdomen should be maintained in immunosuppressed patients.
Core tip: Herein, we present a unique report of a woman with a viable transplanted uterus graft who was suffering from concurrent Clostridium difficile colitis and acute appendicitis. The differential diagnosis in an immunosuppressed patient may be complex, and a high index of suspicion of an atypical course of acute abdomen should be maintained in immunosuppressed patients. Sometimes, more than one synchronous pathological condition may be present. This case highlights the ultimate importance of focusing on the achievement of successful embryo transfer in the uterus transplantation recipients as soon as possible since they are vulnerable to a multitude of possible complications.
- Citation: Kristek J, Kudla M, Chlupac J, Novotny R, Mirejovsky T, Janousek L, Fronek J. Acute appendicitis in a patient after a uterus transplant: A case report. World J Clin Cases 2019; 7(24): 4270-4276
- URL: https://www.wjgnet.com/2307-8960/full/v7/i24/4270.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i24.4270
Uterus transplantation (UTx) is an experimental treatment method for women with uterine factor infertility (UFI). It is a novel, challenging procedure performed in only a few centres around the world; hence, experience with acute abdomen in UTx recipients is rare. The lifetime risk of acute appendicitis (AA) in a normal population has been estimated to be 8.6% and 6.7% for males and females, respectively[1]. AA in solid organ transplant recipients is rare, yet a few small case series have been reported[2,3]. This article presents the first case of a woman with a history of UTx who suffered from AA.
A 26-year-old Caucasian woman suffering from congenital absolute UFI underwent a deceased donor UTx. In the first year of the post-transplant period, 4 episodes of mild acute cellular rejection were diagnosed by cervical biopsy. They were treated with pulses of glucocorticoids and the addition of azathioprine to a maintenance immunosuppressive regimen of tacrolimus. In the further course, the patient developed secondary neutropenia, which was addressed by withdrawal of azathioprine and administration of several pulses of granulocyte colony-stimulating factor.
Apart from congenital uterine agenesis which was treated with UTx, the patient was healthy with no history of further operations. Family history was negative for inherent diseases.
Five months after the UTx, the patient’s compliance was suboptimal. She decided to go on vacation to Egypt despite clear physician recommendation not to do so considering the high risk of acquisition of infectious gastroenteritis.
After her return from Egypt, the patient presented with nausea, abdominal discomfort, and diarrhoea. She was hospitalized to receive rehydration therapy and to run necessary tests.
Upon admission, there were no signs of acute abdomen. The abdomen was mildly tender in all quadrants; there were no signs of peritoneal inflammation.
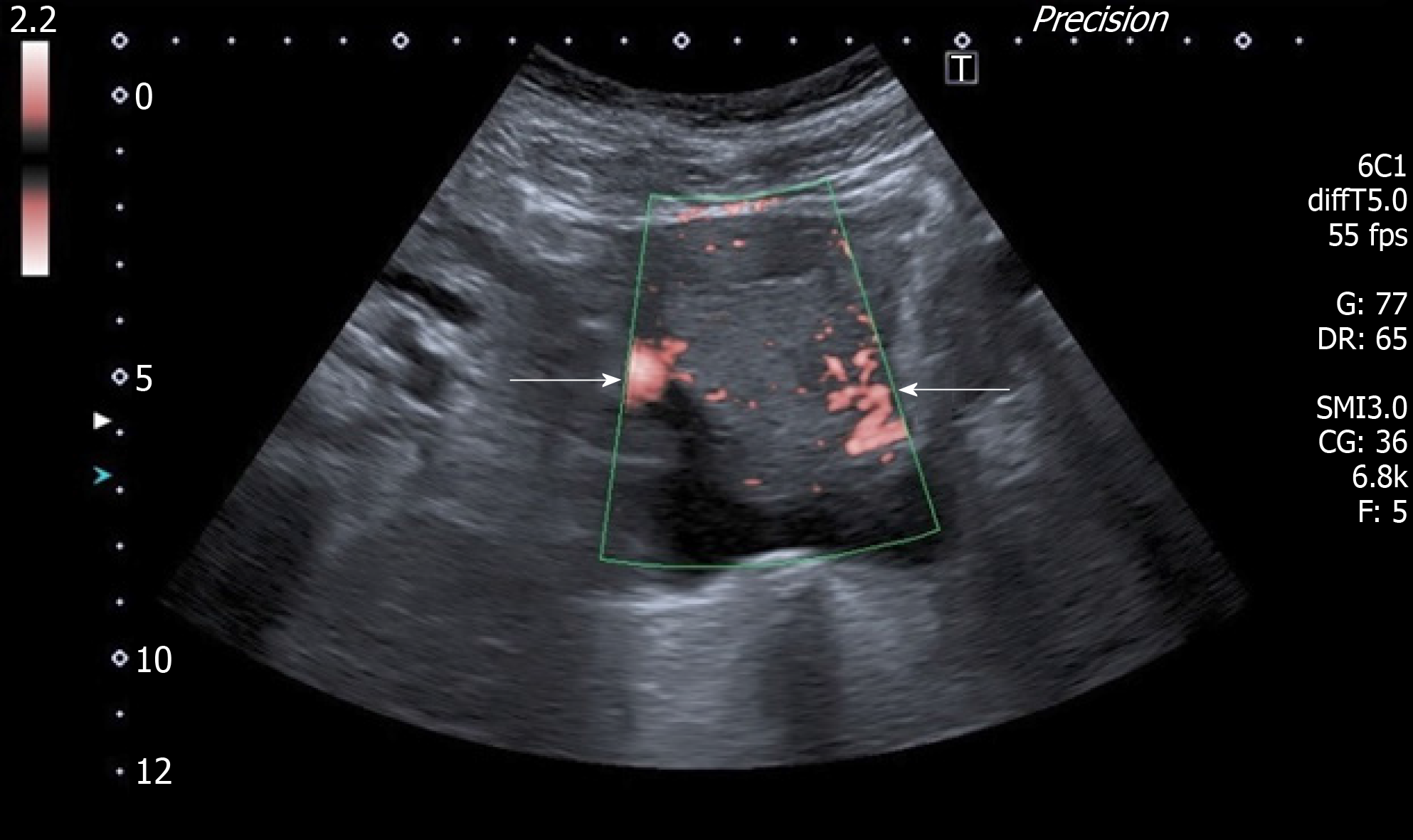
Upon admission, her abdominal ultrasound (US) was normal, although the appendix was not differentiated on baseline US. There was no suspicion of acute abdomen, and thrombosis of the uterine graft was excluded using Doppler ultrasound (Figure 1).
C-reactive protein was 27 mg/L on day 0; the level of leukocytes was within the normal range. However, tests proved to be positive for Clostridium difficile colitis. Due to lack of signs of acute abdomen and verified colitis, we felt it was not necessary to run computed tomography (CT) of the abdomen. A therapy of perorally administered vancomycin 125 mg 4 times a day was started. Viral and parasitic colitis were excluded. Additionally, cytomegalovirus (CMV) polymerase chain reaction was negative. In the course of the next few days, there was a steady progressive elevation of the level of C-reactive protein up to 83 mg/L on day 4. Although the differential blood count showed a normal level of leukocytes, it was considered pathologic because the patient had been leukopenic chronically and there was a new finding of neutrophilia. On day 4, the abdominal discomfort changed to pain and became localized to the right hypogastrium.
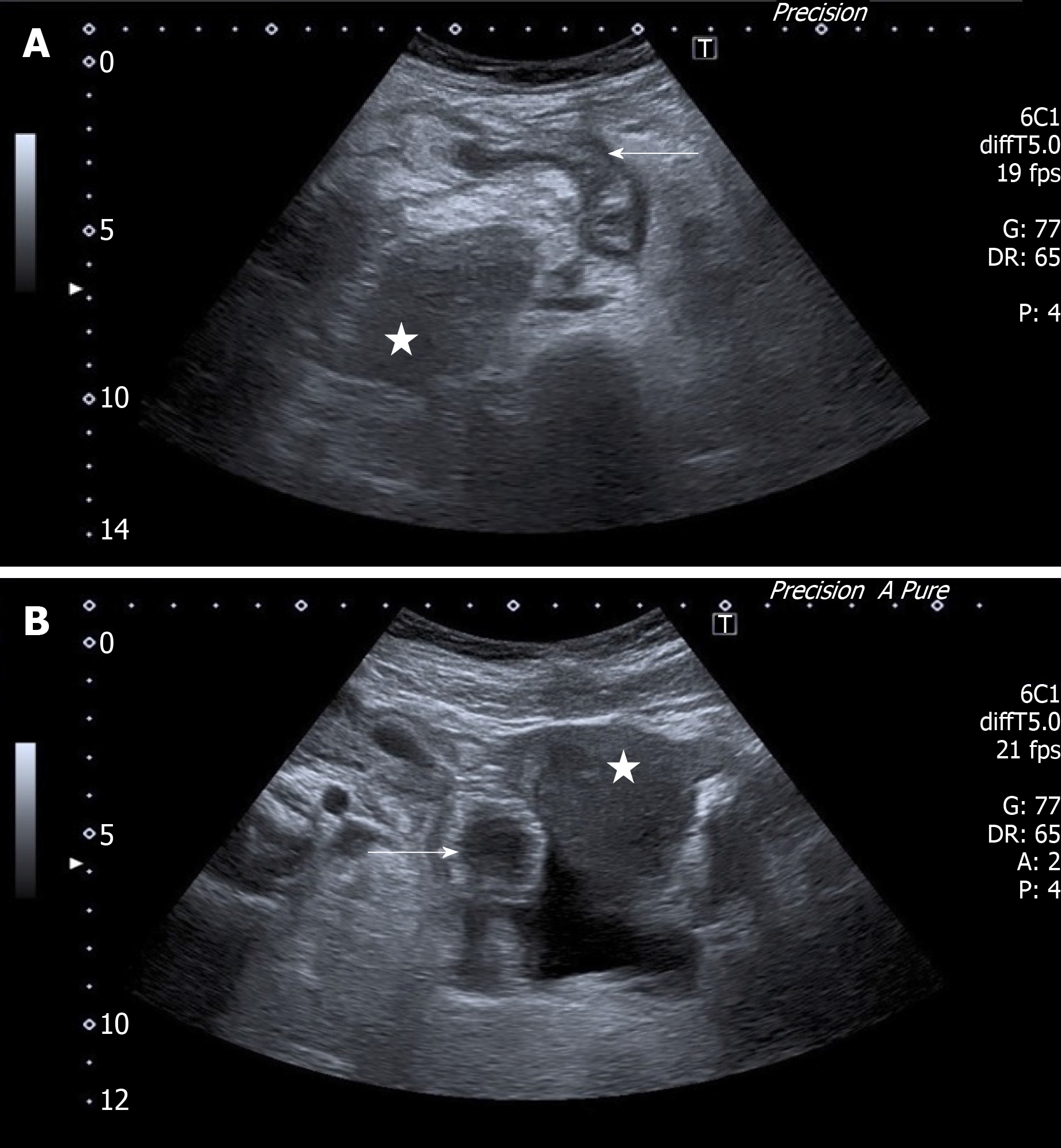
A subsequent US scan revealed a nonhomogeneous tubular structure located behind the uterus, i.e., a finding suggestive of AA (Figure 2A and B). The final diagnosis of the presented case is concurrent Clostridium difficile colitis and acute perforated appendicitis.
The patient underwent an uncomplicated conversion lap-to-open appendectomy. A gangrenous perforated appendix with localized peritonitis was found dorsal to the uterus (Figures 3 and 4). The patient was treated with metronidazole and amoxicillin with clavulanic acid; the tacrolimus immunosuppressive regimen was not discontinued because she was not septic. Subsequently, the tacrolimus levels increased to toxic levels, probably due to diarrhoea and consequently impaired resorption. The medication was changed, and probiotics were administered.
Apart from long-lasting diarrhoea and pancytopenia of complex aetiology, the patient’s follow-up was uneventful. The interval between transplant and appendectomy was 502 days. The patient underwent a successful embryo transfer 6 months after the appendectomy. Apart from pregnancy-induced diabetes, the pregnancy was uneventful. The patient gave birth to a healthy boy at week 35 of gestation.
Although AA has been rarely observed and described in recipients of solid organ transplants, this is the first reported case of AA in a uterus transplant recipient. According to the official transplant terminology, uterus transplant is not considered a solid organ transplant but a vascularized composite allograft, as are other non-vital transplantable organs, including the face, extremities, abdominal wall, and larynx[4]. The prevalence of AA is reported as 0.35%, 0.49%, and 0.21% in kidney transplant recipients (n = 2880), liver transplant recipients (n = 817), and liver, heart, kidney, pancreas-kidney and heart-kidney transplant recipients (n = 8000), respectively[2,3,5].
Generally, immunocompromised patients tend to present late and with minimal symptoms; the symptoms of acute abdomen tend to be weakened by the attenuated immune response. Classic signs of peritonitis, e.g., rebound tenderness and fever, may be feeble or even absent in immunocompromised hosts. Furthermore, nonspecific signs such as tachycardia, hypotension, and confusion may present the only warning of existing abdominal catastrophe[6]. Savar et al[2] came to slightly different conclusions, at least with regard to AA. In their cohort of 15 transplant recipients suffering from AA, the physical findings were similar to the findings in the non-transplant population, i.e., abdominal/right hypogastrium pain (present in 94% of cases) and nausea and vomiting (present in 88% of cases)[2]. Generally, after solid organ transplants that are typically placed in the right iliac fossa/retroperitoneum (kidney or pancreas), AA may be misdiagnosed as a graft-related complication, e.g., infection, acute urine outflow obstruction, or acute rejection of the graft. In UTx recipients, thrombosis of the graft remains the most feared complication. Thrombosis of the vascular pedicles of the uterine graft has been repeatedly presented as a cause of loss of the graft in both animal as well as human studies[7,8]. Since diarrhoea may lead to dehydration and the association between dehydration and a higher risk of venous thrombosis is presumed, graft thrombosis was immediately suspected and subsequently excluded using Doppler US in our case[9]. A possible cause of AA after kidney transplantation is CMV infection. Invasive CMV infection must always be excluded by definitive histopathological evaluation. If the test for CMV is positive, effective antiviral treatment must be instituted[10].
The risk of perforation of an inflamed appendix escalates over time. Perforation is present in approximately 10% of patients by 24 h and in up to 50% of patients by 48 h in the non-transplanted paediatric population[11]. Although the diagnosis of AA is often based on clinical and laboratory findings, the use of either US or CT is recommended if AA is suspected; the sensitivity and specificity of CT are up to 98.5% and up to 98%, respectively[12]. According to a meta-analysis, the rate of a negative appendectomy was 8.7% with the use of preoperative abdominal CT compared to 16.7% based on clinical evaluation alone[13]. However, US may be almost as sensitive as CT in diagnosing AA when performed by well-trained radiologists, with the advantage of no radiation exposure[14].
In our case, if CT was used upon admission, it may have led to timely diagnosis and appendectomy of inflamed yet non-perforated appendix. However, we have suspicion that Clostridium difficile colitis may have been the very cause of the appendicitis. In other words, it may be a case of Clostridium difficile colitis and subsequent acute appendicitis.
UTx is primarily considered a temporary transplant. It cannot be emphasized enough that UTx recipients should preferentially focus on achieving successful embryo transfer. Since UTx recipients are prone to a variety of complications and the side effects of immunosuppression, it is advisable to obviate any risky activities that might compromise achieving the primary aim.
In this paper, we present a unique report of a woman with a viable transplanted uterus graft suffering from Clostridium difficile colitis and AA. The differential diagnosis in an immunosuppressed patient may be complex, and a high index of suspicion of atypical course and indefinite symptomatology of acute abdomen should be maintained in immunosuppressed patients. Sometimes, more than one synchronous pathological condition may be present. In transplanted patients, thrombosis of the vascular pedicles must always be excluded if pain or alteration to the graft’s function occurs. UTx recipients should preferentially focus on achieving successful embryo transfer because they are prone to a variety of complications.
The author would like to thank Dr. Kornelia Chrapkova, PG Dip, for her invaluable help with review of the literature.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: Czech Republic
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hefny AF S-Editor: Zhang L L-Editor: A E-Editor: Qi LL
| 1. | Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132:910-925. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1307] [Cited by in RCA: 1302] [Article Influence: 37.2] [Reference Citation Analysis (0)] |
| 2. | Savar A, Hiatt JR, Busuttil RW. Acute appendicitis after solid organ transplantation. Clin Transplant. 2006;20:78-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Kwon SH, Park SH, Lee HY, Ko EJ, Ban TH, Chung BH, Yang CW. Clinical Characteristics of Acute Appendicitis in Kidney Transplant Recipients. Ann Transplant. 2019;24:168-173. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Samuel U. Regulatory aspects of VCA in Eurotransplant. Transpl Int. 2016;29:686-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Wu L, Zhang J, Guo Z, Tai Q, He X, Ju W, Wang D, Zhu X. Diagnosis and treatment of acute appendicitis after orthotopic liver transplant in adults. Exp Clin Transplant. 2011;9:113-117. [PubMed] |
| 6. | Scott-Conner CE, Fabrega AJ. Gastrointestinal problems in the immunocompromised host. A review for surgeons. Surg Endosc. 1996;10:959-964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Brännström M, Wranning CA, Altchek A. Experimental uterus transplantation. Hum Reprod Update. 2010;16:329-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 79] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 8. | Fageeh W, Raffa H, Jabbad H, Marzouki A. Transplantation of the human uterus. Int J Gynaecol Obstet. 2002;76:245-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 339] [Cited by in RCA: 328] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 9. | Verhaeghe R, Vermylen J, Verstraete M. Thrombosis in particular organ veins. Herz. 1989;14:298-307. [PubMed] |
| 10. | Posen A, Renckens I, Sagaert X, Kuypers D. Subacute cytomegalovirus appendicitis in a renal transplant recipient. Transpl Infect Dis. 2013;15:96-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Chan MK, Wilcox DT, Trompeter RS. Acute appendicitis in children after renal transplantation. Arch Dis Child. 1999;81:372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Pickhardt PJ, Lawrence EM, Pooler BD, Bruce RJ. Diagnostic performance of multidetector computed tomography for suspected acute appendicitis. Ann Intern Med. 2011;154:789-796, W-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 126] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 13. | Krajewski S, Brown J, Phang PT, Raval M, Brown CJ. Impact of computed tomography of the abdomen on clinical outcomes in patients with acute right lower quadrant pain: a meta-analysis. Can J Surg. 2011;54:43-53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 105] [Cited by in RCA: 98] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 14. | Doria AS, Moineddin R, Kellenberger CJ, Epelman M, Beyene J, Schuh S, Babyn PS, Dick PT. US or CT for Diagnosis of Appendicitis in Children and Adults? A Meta-Analysis. Radiology. 2006;241:83-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 486] [Cited by in RCA: 476] [Article Influence: 25.1] [Reference Citation Analysis (0)] |