Published online Dec 6, 2019. doi: 10.12998/wjcc.v7.i23.4137
Peer-review started: September 26, 2019
First decision: October 24, 2019
Revised: November 1, 2019
Accepted: November 14, 2019
Article in press: November 14, 2019
Published online: December 6, 2019
Processing time: 71 Days and 3.8 Hours
Gastric cancer is the third most lethal malignant tumor worldwide. Metastasis has always been a major cause of poor prognosis. Epidemiological evidence shows that the most common sites for metastasis of gastric carcinoma are the liver (48%), peritoneum (32%), lung (15%), and bone (12%); however, subcutaneous metastasis is are and occurs in approximately 0.8% of cases. We report a rare case of armpit subcutaneous metastasis of gastric cancer. The best surgical window was missed, as a result of lacking attention of the mass.
A 69-year-old man who had previously undergone radical gastrectomy and received eight cycles of oral chemotherapy for gastric cancer showed a rapidly growing mass in his the left armpit; within just 3 mo, the mass grew to a size of 6.9 cm × 4.4 cm × 5.7 cm. Color Doppler ultrasonography and Positron emission tomography/computed tomography prompted the possibility of metastasis of the malignancy. Fine needle aspiration biopsy guided by color Doppler ultrasound showed the presence of cancer cells in the mass. Immunohistochemical examination showed CDX-2 (+), PCK (+), CK20 (+), CK7 (-), and TTF (-), which supported the metastasis of gastric cancer. Considering the risk of resection, the patient did not undergo surgical treatment.
The case indicates that unidentified subcutaneous masses in patients with a history of gastric cancer should be carefully evaluated.
Core tip: Epidemiological evidence shows that the most common metastasis sites of gastric carcinoma are the liver (48%), peritoneum (32%), lung (15%), and bone (12%); however, subcutaneous metastasis is are and occurs in approximately 0.8% of cases. The recurrence and metastasis of malignant tumors still contribute to more than 90% of cancer mortalities. For the uncertainty of mechanism of metastasis and metastatic sites, and the limitations of monitoring methods, early detection of metastatic lesions of gastric cancer is difficult. This case demonstrates more sensitive and applicable monitoring methods and early attention may improve the early diagnosis rate.
- Citation: He FJ, Zhang P, Wang MJ, Chen Y, Zhuang W. Left armpit subcutaneous metastasis of gastric cancer: A case report. World J Clin Cases 2019; 7(23): 4137-4143
- URL: https://www.wjgnet.com/2307-8960/full/v7/i23/4137.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i23.4137
Gastric cancer is prevalent worldwide, with an average of approximately 990000 new cases per year from 182 countries and 30 world regions[1]. The highest incidence is observed in Eastern Asia[2,3]. According to the Eindhoven Cancer Registry statistics, between 1995 and 2012, about 40% of gastric cancer patients had one metastasis at least[4]. The most common metastasis sites of gastric carcinoma are the liver (48%), peritoneum (32%), lung (15%), and bone (12%); however, relevant data indicated that the incidence of subcutaneous metastasis of gastric cancer is about 0.8%[5,6]. Today, there is no data referring to the left armpit metastasis of gastric carcinoma. Here we report the case of a patient with stage III gastric carcinoma who underwent curative intent resection (R0) and D2 lymph node dissection and received eight cycles of chemotherapy post-surgery. However, left armpit subcutaneous metastasis occurred in the fifth year after surgery. We report the case to promote the exploration and monitoring of unusual rare metastatic sites of advanced gastric cancer, and provide clinical evidence for the diagnosis and treatment of metastasis of gastric cancer.
A 69-year-old man was re-admitted to West China Hospital of Sichuan University due to an asymptomatic lump in his left armpit for 3 mo (Figure 1).
The patient had a history of gastric neoplasms. Five years ago, he had undergone curative gastrectomy, followed by eight cycles of oral chemotherapy.
The patient had a free previous medical history.
Physical examination after admission showed that the patient’s body temperature was 36 °C, heart rate was 106 bpm, respiratory rate was 20 breaths per minute, and blood pressure was 140/68 mmHg. A mass of approximately 7.0 cm × 4.5 cm × 5.7 cm mass was observed in the left armpit of the patient. The skin of the mass was reddish, and the temperature was high. There was no skin ulceration or itching. The patient experienced no pain when the mass was pressed. The mass was hard, fixed, and had an unclear boundary.
Blood analysis did not reveal raised levels of tumor markers. Prothrombin and partial thromboplastin times were normal and serum C-reactive protein level had increased to 4.5 mg/dL (normal range: < 0.8 mg/dL).
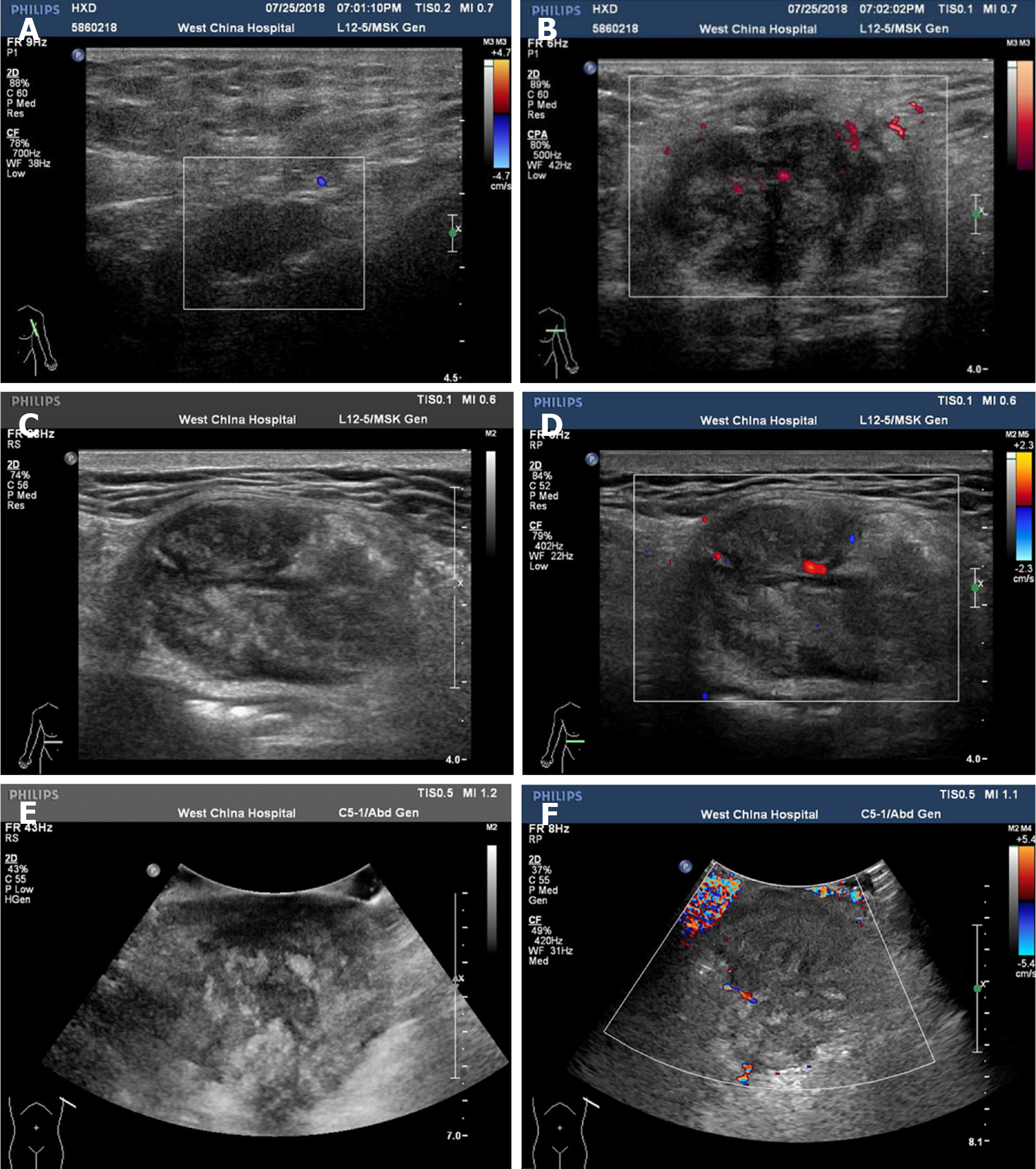
Initial color Doppler ultrasound imaging of the left axillary lump showed a heterogeneous echo pattern sized approximately 4.2 cm × 2.4 cm × 3.8 cm, with an unclear boundary and irregular shape. There was linear blood flow signal observed in the mass. Several abnormally enlarged lymph nodes were observed around the mass. After three months, color Doppler examination revealed that the mass grew to a size of 6.9 cm × 4.4 cm × 5.7 cm (Figure 2). A chest computed tomography (CT) scan revealed a 3.9 cm × 5.7 cm soft tissue lump in the left armpit.
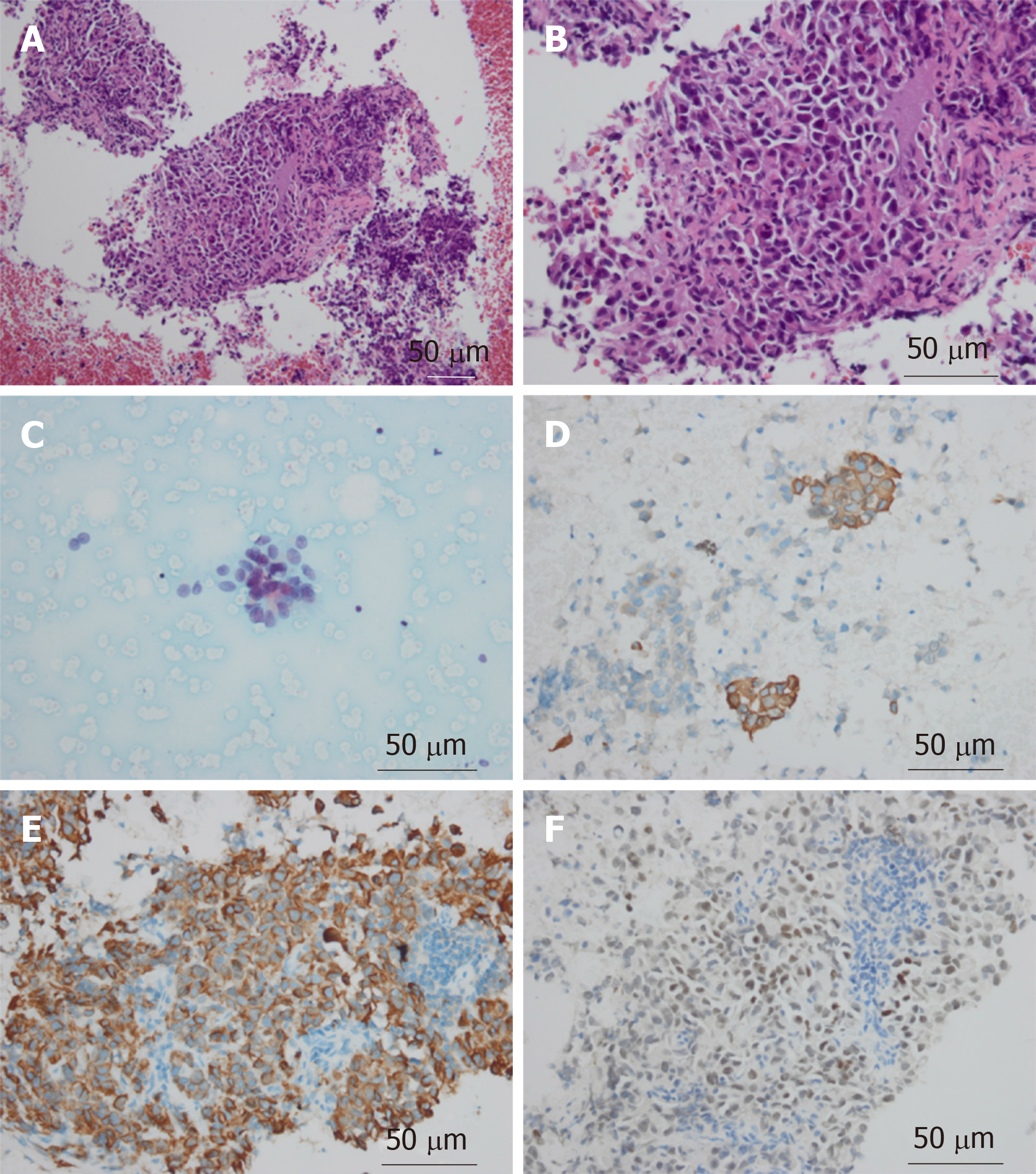
Fine needle aspiration biopsy of the mass guided by color Doppler ultrasound found cancer cells in the mass. Immunohistochemical examination showed that the mass was CDX2-positive, PCK-positive, CK20-positive, CK7-negative, and TTF-negative; this confirmed gastric cancer metastasis (Figure 3).
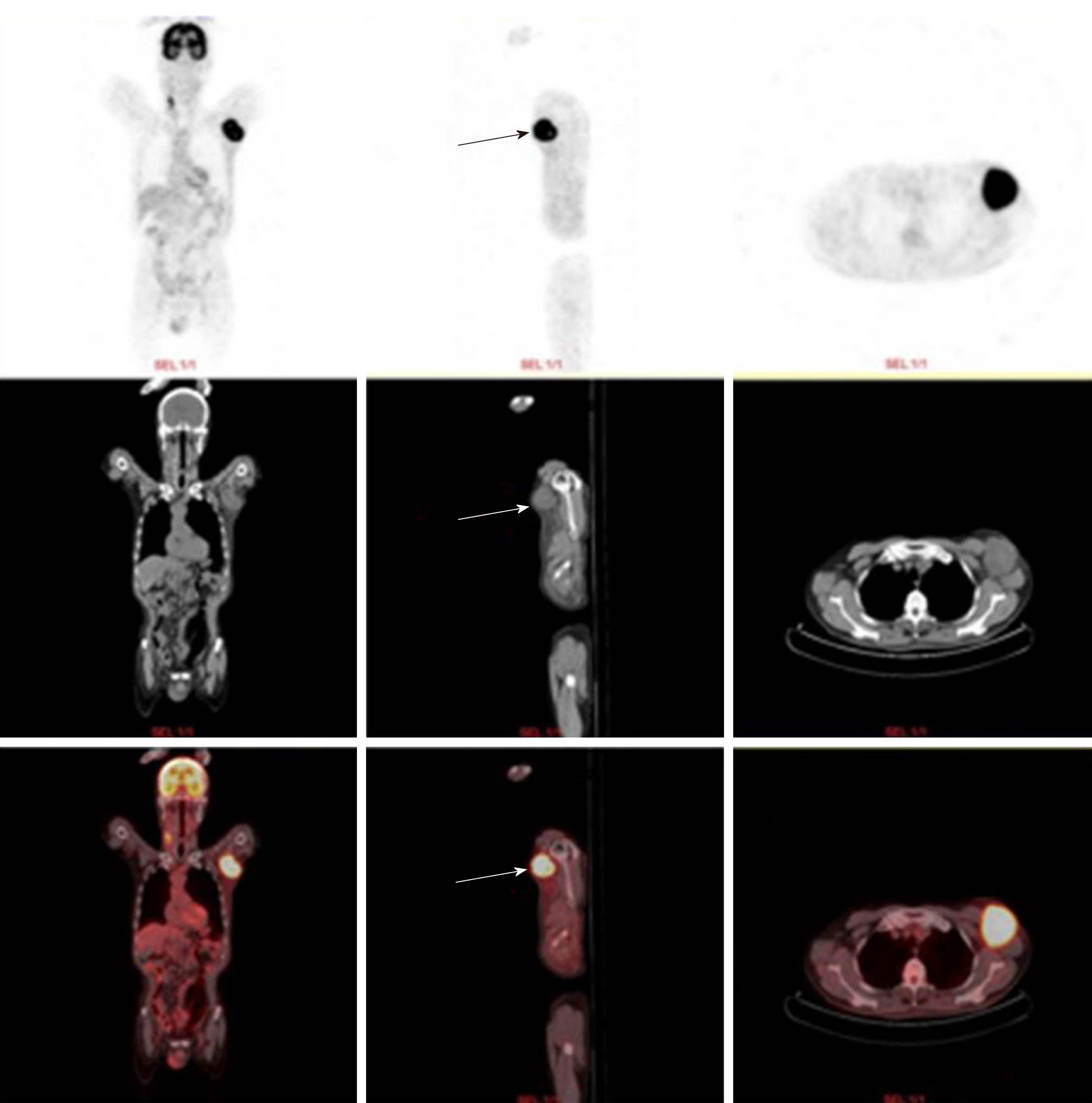
PET/CT examination showed a soft tissue mass sized approximately 6.2 cm × 5.5 cm in the left axilla. The internal density was uneven, and 18F-fludeoxyglucose uptake was abnormally high. The maximum SUV was 11.13 (Figure 4).
The patient should undergo surgical resection of the left axillary tumor and adjuvant radiotherapy, chemotherapy, or targeted therapy.
The patient should undergo surgical treatment of the left mass in his left armpit and total excision of the lesion. If necessary, we will assist in the operation.
Surgical resection of the left axillary subcutaneous tumor may require skin grafting.
Left axillary subcutaneous metastasis of gastric cancer.
Due to the adhesion between the large subcutaneous mass of the left axilla and surrounding tissues and severe local inflammation, skin grafting might be required after operation. We asked plastic surgery experts to assist in the operation of tumor resection. However, considering the risk of resection, the patient did not agree to undergo surgical treatment.
After discharge, the patient was lost to follow-up. However, through telephonic communication, we know that he is on long-term medication and is alive.
Epidemiological studies on metastasis of gastric cancer are rare. Currently, the TNM system is used to stage malignant tumors, and cancer registries often only use “M0” and “M1” to indicate the absence or presence of distant metastasis. Therefore, there is a lack of information regarding specific distant metastasis sites[5].
The five-year cumulative risk of relapse (restricted to patients who undergo R0 resections and excluding in-hospital deaths) for patients with pathological stage T3 tumors is 83% for D1 dissection and 72% for D2 dissection[7]. Although considered a “localized tumor”, gastric cancer may show locoregional metastasis and this can be the most important signal of negative prognosis[8-10].
Metastasis is mostly driven by the acquisition of genetic and/or epigenetic alterations within tumor cells and the formation of the tumor microenvironment[11]. Metastasis of malignant tumors can occur at an early stage of primary tumorigenesis[12]. If metastasis of cancer cells occurs before clinical detection, surgical resection may not prevent recurrence, invasion, and further metastasis. In our case, the patient was followed regularly and monitored through dynamic imaging, and no sign of recurrence was observed. However, in the fifth year, he was diagnosed with distant subcutaneous metastasis. Because of mild clinical manifestations and metastasis into a rare site, the lump was not considered severe. Consequently, we missed the best surgical window.
Currently, ultrasound and color Doppler are the preferred non-invasive imaging modalities of choice allowing to diagnose superficial masses, which can not only differentiate the nature of masses, but also provide detailed information about vascular anatomy[13-15]. Color Doppler, in particular, is highly specific in the identification of benign and malignant nodules of the skin and subcutaneous tissue[16,17]. In addition, high-resolution ultrasound may contribute to the differential diagnosis of skin and subcutaneous lesions[17].
Treatment of even well-confined tumors can become difficult due to repeated changes in molecular phenotypes[18], immune evasion[19], and drug resistance[20]. Through a long-term observation, it has been shown that some types of malignant tumors metastasize only to specific target organs[20]. Cutaneous or subcutaneous tissues may not provide a better growth microenvironment than the liver or peritoneum. However, several cases of subcutaneous metastasis of gastric cancer, including scalp metastasis and mandibular metastasis and so like, have been reported in succession[21,22]. Here we report a rare case that provides clinical evidence for studying the specific metastatic sites of gastric cancer.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Aydin M, Corvino A, Fiori E S-Editor: Dou Y L-Editor: Wang TQ E-Editor: Li X
| 1. | Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893-2917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11128] [Cited by in RCA: 11831] [Article Influence: 845.1] [Reference Citation Analysis (4)] |
| 2. | Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23762] [Cited by in RCA: 25536] [Article Influence: 1824.0] [Reference Citation Analysis (7)] |
| 3. | Forman D, Burley VJ. Gastric cancer: global pattern of the disease and an overview of environmental risk factors. Best Pract Res Clin Gastroenterol. 2006;20:633-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 285] [Cited by in RCA: 307] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 4. | Thomassen I, van Gestel YR, van Ramshorst B, Luyer MD, Bosscha K, Nienhuijs SW, Lemmens VE, de Hingh IH. Peritoneal carcinomatosis of gastric origin: a population-based study on incidence, survival and risk factors. Int J Cancer. 2014;134:622-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 412] [Cited by in RCA: 413] [Article Influence: 37.5] [Reference Citation Analysis (0)] |
| 5. | Riihimäki M, Hemminki A, Sundquist K, Sundquist J, Hemminki K. Metastatic spread in patients with gastric cancer. Oncotarget. 2016;7:52307-52316. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 157] [Cited by in RCA: 297] [Article Influence: 42.4] [Reference Citation Analysis (0)] |
| 6. | Hu SC, Chen GS, Wu CS, Chai CY, Chen WT, Lan CC. Rates of cutaneous metastases from different internal malignancies: experience from a Taiwanese medical center. J Am Acad Dermatol. 2009;60:379-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 160] [Article Influence: 9.4] [Reference Citation Analysis (1)] |
| 7. | Bonenkamp JJ, Hermans J, Sasako M, van de Velde CJ, Welvaart K, Songun I, Meyer S, Plukker JT, Van Elk P, Obertop H, Gouma DJ, van Lanschot JJ, Taat CW, de Graaf PW, von Meyenfeldt MF, Tilanus H; Dutch Gastric Cancer Group. Extended lymph-node dissection for gastric cancer. N Engl J Med. 1999;340:908-914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1158] [Cited by in RCA: 1069] [Article Influence: 41.1] [Reference Citation Analysis (0)] |
| 8. | Imano M, Yasuda A, Itoh T, Satou T, Peng YF, Kato H, Shinkai M, Tsubaki M, Chiba Y, Yasuda T, Imamoto H, Nishida S, Takeyama Y, Okuno K, Furukawa H, Shiozaki H. Phase II study of single intraperitoneal chemotherapy followed by systemic chemotherapy for gastric cancer with peritoneal metastasis. J Gastrointest Surg. 2012;16:2190-2196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Ishigami H, Kitayama J, Kaisaki S, Hidemura A, Kato M, Otani K, Kamei T, Soma D, Miyato H, Yamashita H, Nagawa H. Phase II study of weekly intravenous and intraperitoneal paclitaxel combined with S-1 for advanced gastric cancer with peritoneal metastasis. Ann Oncol. 2010;21:67-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 180] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 10. | Ishigami H, Kitayama J, Kaisaki S, Yamaguchi H, Yamashita H, Emoto S, Nagawa H. Phase I study of biweekly intravenous paclitaxel plus intraperitoneal cisplatin and paclitaxel for gastric cancer with peritoneal metastasis. Oncology. 2010;79:269-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (1)] |
| 11. | Valastyan S, Weinberg RA. Tumor metastasis: molecular insights and evolving paradigms. Cell. 2011;147:275-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2388] [Cited by in RCA: 2954] [Article Influence: 211.0] [Reference Citation Analysis (0)] |
| 12. | Turajlic S, Swanton C. Metastasis as an evolutionary process. Science. 2016;352:169-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 436] [Cited by in RCA: 453] [Article Influence: 50.3] [Reference Citation Analysis (0)] |
| 13. | Corvino A, Catalano O, Corvino F, Sandomenico F, Setola SV, Petrillo A. Superficial temporal artery pseudoaneurysm: what is the role of ultrasound? J Ultrasound. 2016;19:197-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 14. | Corvino A, Corvino F, Catalano O, Sandomenico F, Petrillo A. The Tail and the String Sign: New Sonographic Features of Subcutaneous Melanoma Metastasis. Ultrasound Med Biol. 2017;43:370-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (1)] |
| 15. | Corvino A, Sandomenico F, Setola SV, Corvino F, Pinto F, Catalano O. Added value of contrast-enhanced ultrasound (CEUS) with Sonovue® in the diagnosis of inferior epigastric artery pseudoaneurysm: report of a case and review of literature. J Ultrasound. 2019;22:485-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 16. | Giovagnorio F, Andreoli C, De Cicco ML. Color Doppler sonography of focal lesions of the skin and subcutaneous tissue. J Ultrasound Med. 1999;18:89-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 71] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 17. | Catalano O, Roldán FA, Varelli C, Bard R, Corvino A, Wortsman X. Skin cancer: findings and role of high-resolution ultrasound. J Ultrasound. 2019;22:423-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 67] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 18. | Nakamura J, Okuyama K, Sato H, Yoda Y, Kai K, Noshiro H. Repeated changes of the molecular subtype in gastric metastasis from breast cancer: A case report. Mol Clin Oncol. 2016;4:695-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51728] [Cited by in RCA: 47023] [Article Influence: 3358.8] [Reference Citation Analysis (5)] |
| 20. | Fidler IJ. The pathogenesis of cancer metastasis: the 'seed and soil' hypothesis revisited. Nat Rev Cancer. 2003;3:453-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3231] [Cited by in RCA: 3322] [Article Influence: 151.0] [Reference Citation Analysis (0)] |
| 21. | Kawai S, Nishida T, Hayashi Y, Ezaki H, Yamada T, Shinzaki S, Miyazaki M, Nakai K, Yakushijin T, Watabe K, Iijima H, Tsujii M, Nishida K, Takehara T. Choroidal and cutaneous metastasis from gastric adenocarcinoma. World J Gastroenterol. 2013;19:1485-1488. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 18] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Kirchberger MC. Unusual presentation of a cutaneous metastasis in the face arising from gastric cancer: a case report. SAGE Open Med Case Rep. 2018;6:2050313X18795080. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 23. | Li R, Liu B, Gao J. The application of nanoparticles in diagnosis and theranostics of gastric cancer. Cancer Lett. 2017;386:123-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 52] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 24. | Pantel K, Alix-Panabières C. Liquid biopsy and minimal residual disease - latest advances and implications for cure. Nat Rev Clin Oncol. 2019;16:409-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 440] [Cited by in RCA: 720] [Article Influence: 120.0] [Reference Citation Analysis (0)] |