Published online Nov 6, 2019. doi: 10.12998/wjcc.v7.i21.3615
Peer-review started: July 16, 2019
First decision: September 9, 2019
Revised: September 20, 2019
Accepted: October 5, 2019
Article in press: October 5, 2019
Published online: November 6, 2019
Processing time: 127 Days and 20.1 Hours
Adenomyomatous hyperplasia of the distal common bile duct (CBD) is very rare, with only scarce case reports in the literature. Diagnosis is usually based on imaging findings, and endoscopic biopsy is very difficult before operation. It is believed that adenomyomatous hyperplasia has little or no risk of malignant transformation.
A 68-year-old woman with abdominal pain in the right upper quadrant was referred to our hospital. Abdominal ultrasonography in the emergency ward revealed acute cholecystitis and dilated CBD. Laboratory findings showed elevated levels of transaminases, phosphatase, and γ-glutamyltranspeptidase. Pharmaceutical treatment for 3 d did not relieve the symptoms. Magnetic resonance cholangiopancreatography (MRCP) and computed tomography (CT) showed proximal bile duct dilatation but could not identify the cause. Endoscopic ultrasonography (EUS) demonstrated a mixed echogenic mass in the distal CBD. During surgery, a firm mass was found in the distal CBD and the Whipple procedure was performed with the initial concern of malignancy. Histology showed diffuse adenomyomatous hyperplasia.
EUS may be a useful choice to diagnose adenomyoma of the distal CBD before operation, especially in patients with ambiguous MRCP/CT findings.
Core tip: The distal common bile duct is an extremely rare site of adenomyomatous hyperplasia. Diagnosis is usually based on imaging findings, and endoscopic biopsy is difficult before operation. We present here a rare case of adenomyomatous hyperplasia of the distal common bile duct demonstrated by endoscopic ultrasound, which revealed a nodular change and bile duct wall thickening. We concluded that the mass was a benign, non-neoplastic lesion. This case highlights how endoscopic ultrasound may be a useful choice for the diagnosis of adenomyoma of the distal common bile duct, especially in patients with ambiguous magnetic resonance cholangiopancreatography/computed tomography findings.
- Citation: Xu LM, Hu DM, Tang W, Wei SH, Chen W, Chen GQ. Adenomyoma of the distal common bile duct demonstrated by endoscopic ultrasound: A case report and review of the literature. World J Clin Cases 2019; 7(21): 3615-3621
- URL: https://www.wjgnet.com/2307-8960/full/v7/i21/3615.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i21.3615
Most of adenomyomas are located in the gallbladder, stomach, duodenum, and jejunum[1-5]. The distal common bile duct (CBD) is an extremely rare site of adenomyomatous hyperplasia[1,5,6], and here we report here our experience with such a case. For our case, histology demonstrated glandular structures that were surrounded by a fibroblastic or myofibroblastic proliferation. Reported symptoms for these rare cases are nonspecific and include jaundice, abdominal pain, nausea, vomiting, dysphagia, and unintentional weight loss[1,3,7]. A dilated CBD is common and sometimes presents intermittently in the adenomyoma of the Vaterian system[1,3]. It can be very difficult to distinguish an adenomyoma from a malignancy before operation; this is a valid concern as adenomyomas have little or no risk of malignant transformation[8-10].
A 68-year-old woman with abdominal pain located in the right upper quadrant was referred to our hospital. Abdominal ultrasonography (US) performed in the emergency ward revealed stones in the gallbladder, with acute cholecystitis and dilated CBD.
The patient’s symptoms had begun 5 h prior to presentation at the hospital. The patient reported no vomiting or fever. Upon hospital admission, the initial treatment with antibiotics and anticholinergic did not relieve the symptoms.
The patient had a history of hypertension and appendectomy. She was allergic to penicillin.
The patient had no habits of tobacco or alcohol intake. There were no risk factors for common diseases in the family history.
On admission, the patient’s temperature was 36.5 °C, heart rate was 85 beats per min, respiratory rate was 18 breaths per min, and blood pressure was 120/70 mmHg. Routine abdominal examination revealed tenderness and rebound tenderness in the right upper quadrant. There was no shifting dullness. Normal active intestinal sounds were heard. There was no jaundice of the sclera or skin. There were no significant findings from palpation of the lymph nodes and no edema. Lung and heart auscultation was negative.
Laboratory tests were conducted and the results were as follows: White blood cell count, 5.7 × 10³/μL; neutrophil count, 4.7 × 10³/μL; hemoglobin, 12.7 g/dL; platelet count, 182 × 10³/μL; total bilirubin/direct bilirubin, 18.7/9.5 μmol/L; aspartate aminotransferase/alanine aminotransferase, 540/482 U/L; alkaline phosphatase/γ-glutamyltranspeptidase, 111/175 U/L; amylase/lipase, 54/34 U/L; C-reactive protein 58.8 mg/L; carcinoembryonic antigen, 2.03 ng/mL; carbohydrate antigen 19-9, 76.11 U/mL; and carbohydrate antigen 50, 30.46 IU/mL. Hepatitis tests showed positivity for hepatitis B surface, e, and core antibodies. Symptoms were not relieved after 3 d of pharmaceutical treatments (reductive glutathione at 2.4 qdivgtt; ceftizoxime at 2.0 bid ivgtt). Laboratory findings showed decreased levels of transaminases (192/103 U/L) and elevated levels of phosphatase (203 U/L) and γ-glutamyltranspeptidase (496 U/L).
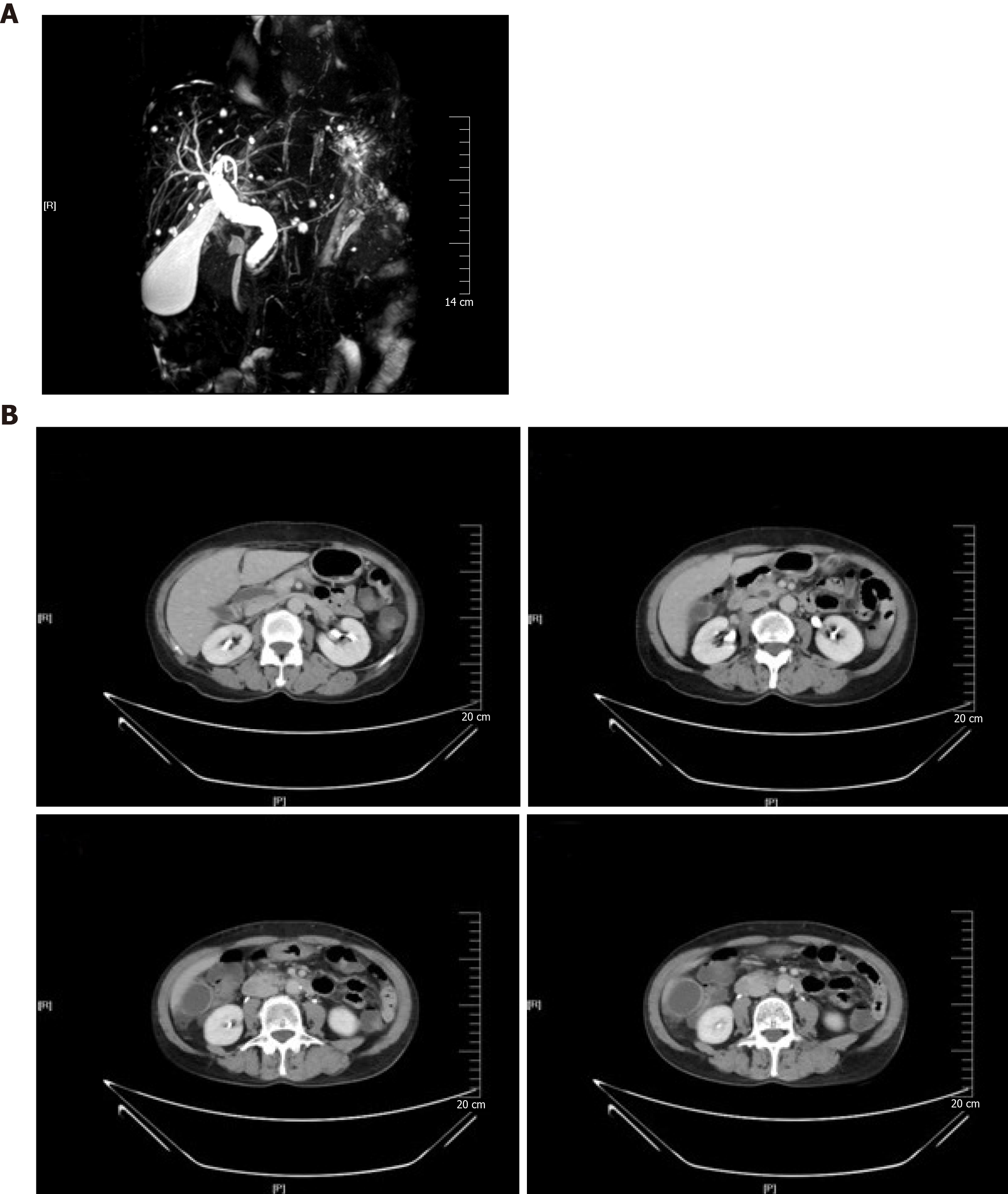
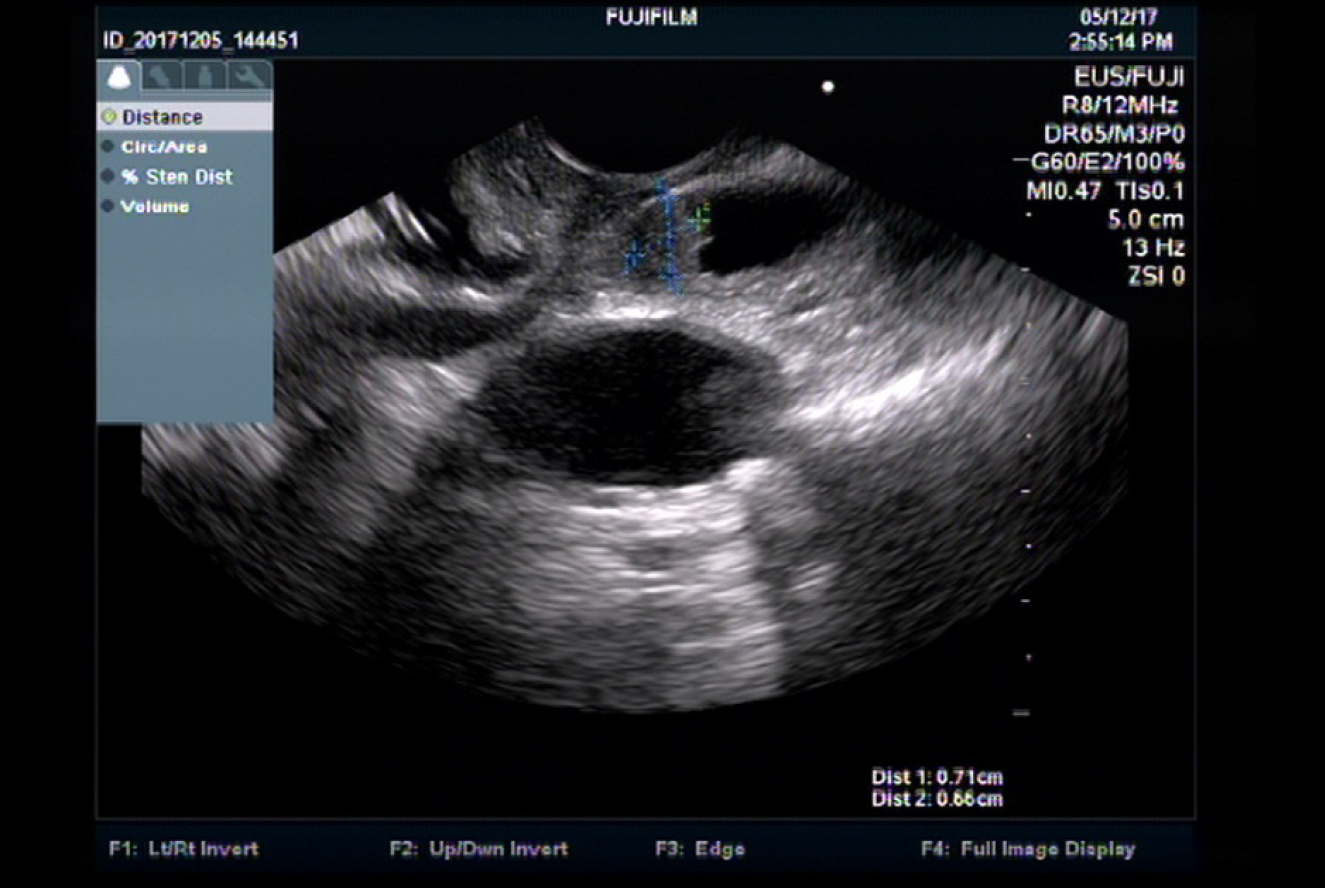
Magnetic resonance cholangiopancreatography (MRCP) showed proximal bile duct dilatation, with the diameter being 17.5 mm (Figure 1A). 128-row multi-detector computed tomography (CT) and magnetic resonance imaging of the abdomen were consistent, showing diffused dilatation of the extra-hepatic bile duct and significantly enhanced bile duct wall (Figure 1B). Endoscopic US (EUS) was performed for the evaluation of distal CBD obstruction, which demonstrated a mixed echogenic structure (low-mild amplitude echoes, 7.1 mm × 6.6 mm) in the distal CBD (Figure 2).
The final diagnosis prior to surgery was neoplasm of the distal CBD.
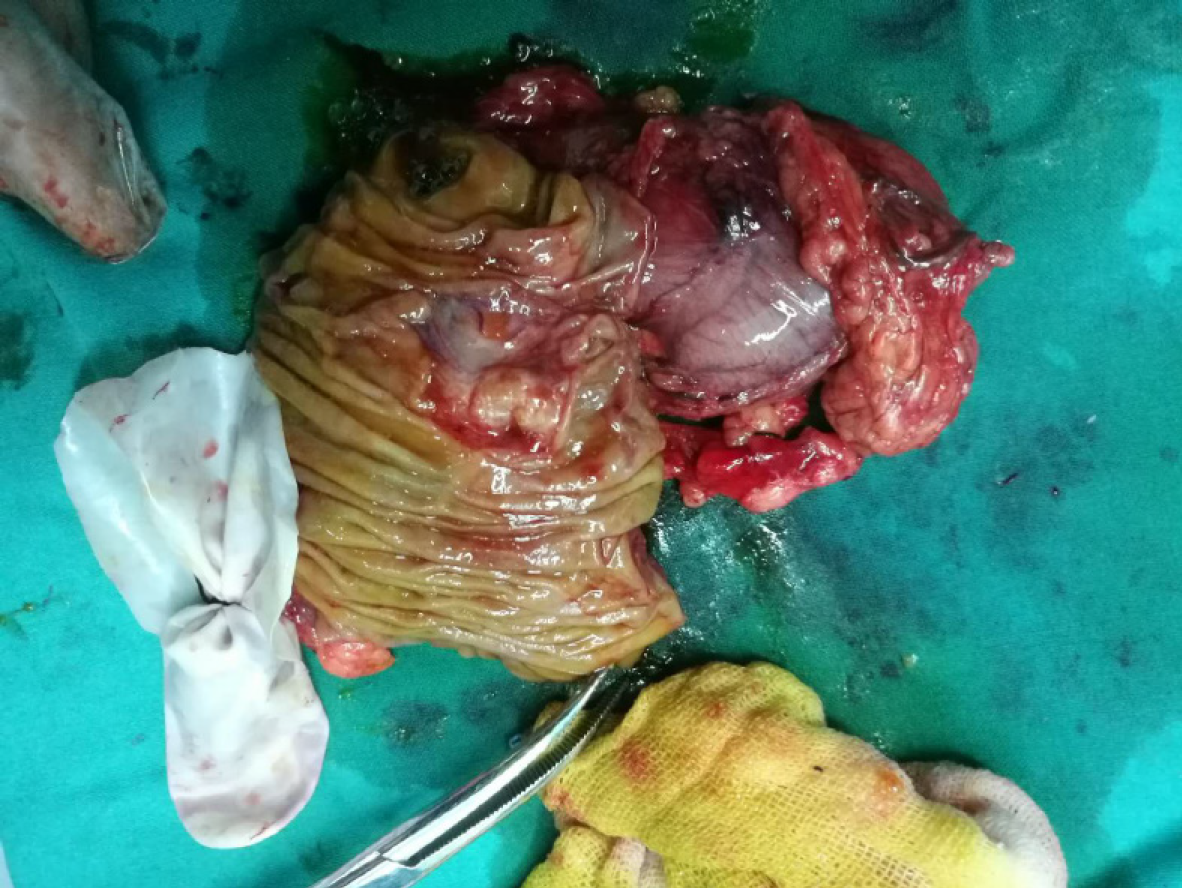
In accordance with the diagnosis, the patient agreed to undergo surgery. During the operation, a 7 mm × 7 mm sized, firm mass was found in the distal CBD near the ampulla of Vater. The surgeon performed radical pancreaticoduodenectomy by the Whipple procedure and cholecystectomy, having concern of a malignant tumor.
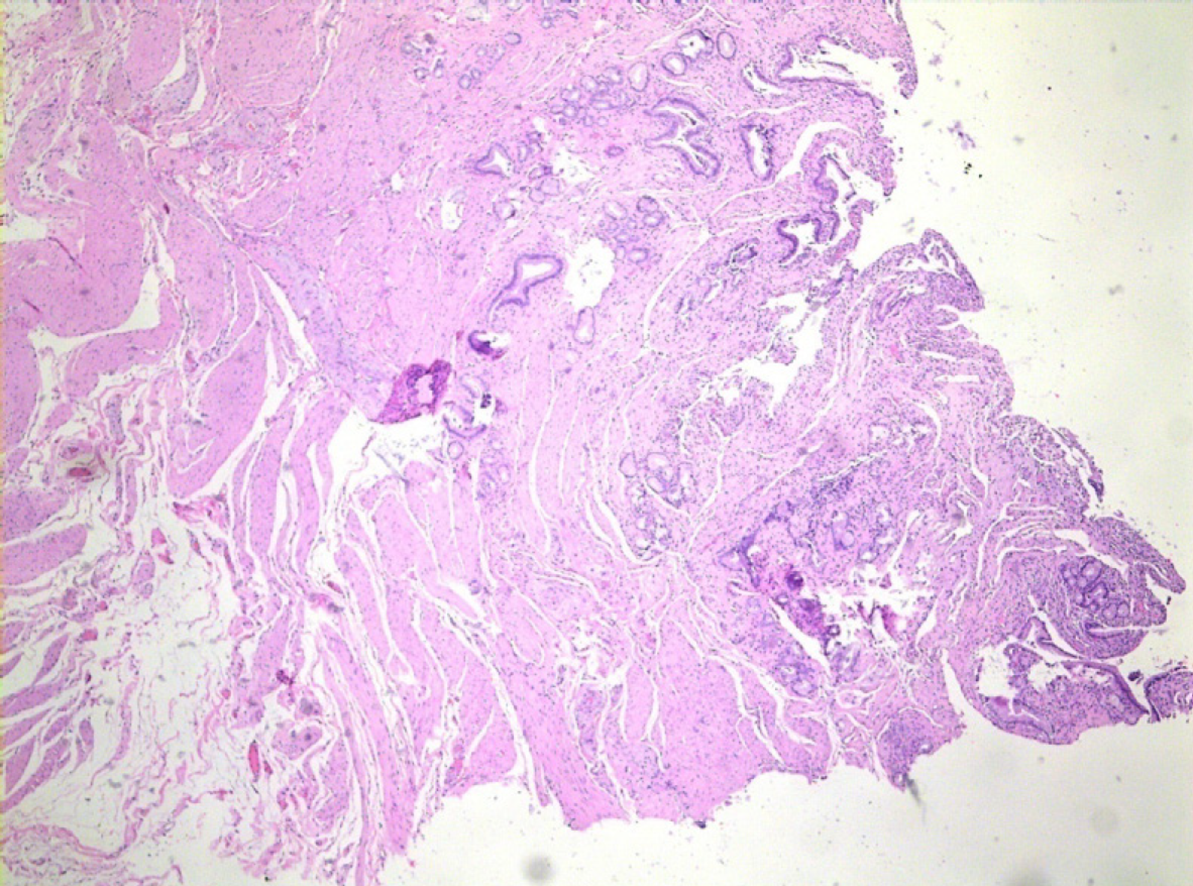
The gross specimen appeared as an irregular mass, measuring 1 cm and having an obscure boundary (Figure 3). For resection, the tumor was separated from the surrounding duodenum and pancreas. Histology of the specimen showed diffuse adenomyomatous hyperplasia of the distal CBD and acute cholecystitis. All the regional lymph nodes showed reactive hyperplasia. No evidence of vascular or perineural neoplastic invasion was observed (Figure 4). The diagnosis of adenomyoma was finally confirmed and no adjuvant therapy was needed.
The overall accuracy for preoperative histopathological diagnosis is 62% for tumors in the papilla of Vater[11]. Diagnosis of adenomyomas of the CBD is usually based on imaging findings and endoscopic biopsy is difficult[5]. CBD dilation is demonstrated by US, CT, and MRCP in the cases of obstructive jaundice[12,13]. Although noninvasive and inexpensive, US-provided diagnosis can be operator-dependent (according to an operator’s experience). CT has a lower sensitivity and accuracy in differentiating adenomyomatosis and gallbladder cancer[14].
Endoscopic retrograde cholangiopancreatography (ERCP), another imaging option, is considered the gold standard for the diagnosis of distal CBD abnormalities[15-17]. However, it may induce severe complications such as post-ERCP pancreatitis[18]. MRCP and EUS are less invasive and useful in diagnosing malignancy and choledocholithiasis in the dilated biliary tree[19,20]. Studies have shown that MRCP and EUS are comparable[20,21]. When MRCP findings are negative in the presence of dilated CBD, EUS provides better visualization of the biliary obstruction because its transducer is close enough to the CBD in the duodenum. Patel et al[23] preferred EUS rather than ERCP as the initial investigation in patients with a probability of choledocholithiasis. Endosonography may also be useful in the evaluation of cholangiocarcinoma[24]. Chon et al[25] considered EUS a key method for investigating biliary disorders of unknown reason.
In our patient, EUS revealed that the lesion was a nodular change with mixed echo, with the bile duct wall being thickened and enhanced. We concluded that it was a benign, non-neoplastic lesion but one not reported in the literature according to the best of our knowledge. There have been no long-term studies reported with large sample size for adenomyomatous hyperplasia of the CBD. The prognosis of the lesion is expected to be similar to that of the gallbladder, based upon the histological similarity[9]. EUS shows adenomyoma of the gallbladder with hyper and mixed echogenecity and the well-preserved multiple-layer pattern of the wall[26], which is similar to the findings in our patient’s mass. We regret that we did not perform fine needle aspiration (FNA) and then ERCP. The sensitivity of EUS-FNA for diagnosis of malignancy is 66%[27]. The sensitivity of ERCP with brush cytology and intra-ductal biopsy is 45% and 48.1%, respectively[27]. De Moura et al[28] reported that EUS-FNA was superior to ERCP with brush cytology for diagnosing malignant biliary strictures. If such was diagnosed definitively as adenomyoma, endoscopic treatments like drainage or local resection should be performed, as they carry less risk for complications than the radical surgical procedure[5,6]. Meanwhile, the method of EUS-guided biliary drainage might be a primary alternative in patients with malignant obstruction[29,30].
EUS is an important diagnostic modality that can help establish the diagnosis of adenomyomatous hyperplasia in patients with dilated CBD and ambiguous MRCP findings. We expect that the EUS image can be a useful choice to diagnose adenomyoma of the distal CBD. Moreover, EUS-FNA biopsy could be taken from the adenomyoma for further histopathological examination.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chandrakesan P, Raisch KP S-Editor: Wang JL L-Editor: Wang TQ E-Editor: Wu YXJ
| 1. | Läuffer JM, Baer HU, Maurer CA, Fröhling S, Scheurer U, Zimmermann A, Büchler MW. Adenomyoma of the distal common bile duct mimicking cholangiocarcinoma. Dig Dis Sci. 1998;43:1200-1204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Colović R, Micev M, Marković J, Zogović S, Colović N, Stojković M. Adenomyoma of the common hepatic duct. HPB (Oxford). 2002;4:187-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Handra-Luca A, Terris B, Couvelard A, Bonte H, Flejou JF. Adenomyoma and adenomyomatous hyperplasia of the Vaterian system: clinical, pathological, and new immunohistochemical features of 13 cases. Mod Pathol. 2003;16:530-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 45] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Kwon TH, Park DH, Shim KY, Cho HD, Park JH, Lee SH, Chung IK, Kim HS, Park SH, Kim SJ. Ampullary adenomyoma presenting as acute recurrent pancreatitis. World J Gastroenterol. 2007;13:2892-2894. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Iwaki K, Shibata K, Ohta M, Endo Y, Uchida H, Tominaga M, Okunaga R, Kai S, Kitano S. Adenomyomatous hyperplasia of the common bile duct: report of a case. Surg Today. 2008;38:85-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Choi JH, Lee SH, Kim JS, Kim J, Shin BS, Jang DK, Ryu JK, Kim YT. A Case of Adenomyomatous Hyperplasia of the Distal Common Bile Duct Mimicking Malignant Stricture. Korean J Gastroenterol. 2016;67:332-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Choi YH, Kim MJ, Han JH, Yoon SM, Chae HB, Youn SJ, Kang MH, Sung R, Choi JW, Park SM. Clinical, pathological, and immunohistochemical features of adenomyoma in the ampulla of vater. Korean J Gastroenterol. 2013;62:352-358. [PubMed] |
| 8. | Singh DK, Rastogi A, Sakhuja P, Gondal R. Adenomyoma of common bile duct arising in a type I choledochal cyst. Indian J Pathol Microbiol. 2011;54:365-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Kim JH, Jeong IH, Han JH, Kim JH, Hwang JC, Yoo BM, Kim JH, Kim MW, Kim WH. Clinical/pathological analysis of gallbladder adenomyomatosis; type and pathogenesis. Hepatogastroenterology. 2010;57:420-425. [PubMed] |
| 10. | Patel S, Slade J, Jakate S. An Unusual Case of Noninvasive Adenocarcinoma Arising in a Localized Adenomyoma of the Gallbladder and Review of Literature. Int J Surg Pathol. 2016;24:341-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Menzel J, Poremba C, Dietl KH, Böcker W, Domschke W. Tumors of the papilla of Vater--inadequate diagnostic impact of endoscopic forceps biopsies taken prior to and following sphincterotomy. Ann Oncol. 1999;10:1227-1231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 62] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 12. | Sotoudehmanesh R, Nejati N, Farsinejad M, Kolahdoozan S. Efficacy of Endoscopic Ultrasonography in Evaluation of Undetermined Etiology of Common Bile Duct Dilatation on Abdominal Ultrasonography. Middle East J Dig Dis. 2016;8:267-272. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Holm AN, Gerke H. What should be done with a dilated bile duct? Curr Gastroenterol Rep. 2010;12:150-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (1)] |
| 14. | Bang SH, Lee JY, Woo H, Joo I, Lee ES, Han JK, Choi BI. Differentiating between adenomyomatosis and gallbladder cancer: revisiting a comparative study of high-resolution ultrasound, multidetector CT, and MR imaging. Korean J Radiol. 2014;15:226-234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 53] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 15. | Chen S, Bacon BR, Berlin JA, Fleischer D, Hecht GA, Loehrer PJ Sr, McNair AE Jr, Mulholland M, Norton NJ, Rabeneck L, Ransohoff DF, Sonnenberg A, Vannier MW. National Institutes of Health State-of-the-Science Conference Statement: ERCP for diagnosis and therapy, January 14-16, 2002. Gastrointest Endosc. 2002;56:803-809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 46] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 16. | Chen WX, Zhang Y, Li YM, Xu GQ, Fang Y, Cai SP. Endoscopic retrograde cholangiopancreatography in evaluation of choledochal dilatation in patients with obstructive jaundice. Hepatobiliary Pancreat Dis Int. 2002;1:111-113. [PubMed] |
| 17. | Rafiullah, Tanimu S. Adenomyomatous hyperplasia of the ampulla of Vater presenting as acute pancreatitis. BMJ Case Rep. 2014;2014:bcr2013203151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Nalankilli K, Kannuthurai S, Moss A. A modern approach to ERCP: maintaining efficacy while optimising safety. Dig Endosc. 2016;28 Suppl 1:70-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Adler DG, Baron TH, Davila RE, Egan J, Hirota WK, Leighton JA, Qureshi W, Rajan E, Zuckerman MJ, Fanelli R, Wheeler-Harbaugh J, Faigel DO; Standards of Practice Committee of American Society for Gastrointestinal Endoscopy. ASGE guideline: the role of ERCP in diseases of the biliary tract and the pancreas. Gastrointest Endosc. 2005;62:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 286] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 20. | Fernández-Esparrach G, Ginès A, Sánchez M, Pagés M, Pellisé M, Fernández-Cruz L, López-Boado MA, Quintó L, Navarro S, Sendino O, Cárdenas A, Ayuso C, Bordas JM, Llach J, Castells A. Comparison of endoscopic ultrasonography and magnetic resonance cholangiopancreatography in the diagnosis of pancreatobiliary diseases: a prospective study. Am J Gastroenterol. 2007;102:1632-1639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 66] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 21. | Tse F, Liu L, Barkun AN, Armstrong D, Moayyedi P. EUS: a meta-analysis of test performance in suspected choledocholithiasis. Gastrointest Endosc. 2008;67:235-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 129] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 22. | Rana SS, Bhasin DK, Sharma V, Rao C, Gupta R, Singh K. Role of endoscopic ultrasound in evaluation of unexplained common bile duct dilatation on magnetic resonance cholangiopancreatography. Ann Gastroenterol. 2013;26:66-70. [PubMed] |
| 23. | Patel R, Ingle M, Choksi D, Poddar P, Pandey V, Sawant P. Endoscopic Ultrasonography Can Prevent Unnecessary Diagnostic Endoscopic Retrograde Cholangiopancreatography Even in Patients with High Likelihood of Choledocholithiasis and Inconclusive Ultrasonography: Results of a Prospective Study. Clin Endosc. 2017;50:592-597. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 24. | De Angelis C, Marietti M, Bruno M, Pellicano R, Rizzetto M. Endoscopic ultrasound in common bile duct dilatation with normal liver enzymes. World J Gastrointest Endosc. 2015;7:799-805. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (1)] |
| 25. | Chon HK, Kim TH. A case of biliary fascioliasis mimicking a common bile duct tumor (with video). Endosc Ultrasound. 2017;6:145-146. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | Kim HJ, Park JH, Park DI, Cho YK, Sohn CI, Jeon WK, Kim BI, Choi SH. Clinical usefulness of endoscopic ultrasonography in the differential diagnosis of gallbladder wall thickening. Dig Dis Sci. 2012;57:508-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 27. | Navaneethan U, Njei B, Lourdusamy V, Konjeti R, Vargo JJ, Parsi MA. Comparative effectiveness of biliary brush cytology and intraductal biopsy for detection of malignant biliary strictures: a systematic review and meta-analysis. Gastrointest Endosc. 2015;81:168-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 372] [Cited by in RCA: 341] [Article Influence: 34.1] [Reference Citation Analysis (1)] |
| 28. | De Moura DTH, Moura EGH, Bernardo WM, De Moura ETH, Baraca FI, Kondo A, Matuguma SE, Almeida Artifon EL. Endoscopic retrograde cholangiopancreatography versus endoscopic ultrasound for tissue diagnosis of malignant biliary stricture: Systematic review and meta-analysis. Endosc Ultrasound. 2018;7:10-19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 90] [Cited by in RCA: 91] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 29. | Baars JE, Kaffes AJ, Saxena P. EUS-guided biliary drainage: A comprehensive review of the literature. Endosc Ultrasound. 2018;7:4-9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 46] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 30. | Ge N, Hu J, Sun S, Linghu E, Jin Z, Li Z. Endoscopic Ultrasound-guided Pancreatic Pseudocyst Drainage with Lumen-apposing Metal Stents or Plastic Double-pigtail Stents: A Multifactorial Analysis. J Transl Int Med. 2017;5:213-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |