Published online Nov 6, 2019. doi: 10.12998/wjcc.v7.i21.3569
Peer-review started: July 23, 2019
First decision: July 31, 2019
Revised: September 1, 2019
Accepted: September 11, 2019
Article in press: September 11, 2019
Published online: November 6, 2019
Processing time: 108 Days and 13.2 Hours
Portopulmonary hypertension (PoPH) is not uncommon in patients waiting for liver transplantation (LT). Severe PoPH has a very high perioperative mortality rate and is still considered a contraindication for LT. Many patients with liver disease require but cannot receive LT due to severe PoPH and eventually died. We report a patient with severe PoPH who underwent successful LT and had near normal pulmonary pressure without drug treatment.
A 39-year-old woman was hospitalized with the chief complaint of jaundice and exertional dyspnea and fatigue. Caroli disease and liver cirrhosis was diagnosed 6 years previously. Her liver disease met the criteria for LT. However, right heart catheterization showed that her mean pulmonary artery pressure was increased at 50 mmHg, pulmonary vascular resistance was 460 dyn∙s/cm5 and pulmonary artery wedge pressure was 20 mmHg, which may have been the reasons for her chief complaint. The patient was diagnosed with severe PoPH and was not listed for LT immediately. After 5 mo of pharmacotherapy, her severe PoPH was moderate, and she underwent successful LT. Pulmonary artery pressure steadily decreased according to post-operative echocardiographic monitoring and drugs have been discontinued for a month.
The safety of LT can be greatly improved by reducing mean pulmonary artery pressure to a low level, and LT may cure PoPH.
Core tip: Peri-operative pharmacotherapy was administered to a patient with portopulmonary hypertension (PoPH) to reduce pulmonary pressure in order to ensure the safety of liver transplantation (LT). LT may eventually cure severe PoPH.
- Citation: Chen XJ, Zhu ZJ, Sun LY, Wei L, Zeng ZG, Liu Y, Qu W, Zhang L. Liver transplantation for severe portopulmonary hypertension: A case report and literature review. World J Clin Cases 2019; 7(21): 3569-3574
- URL: https://www.wjgnet.com/2307-8960/full/v7/i21/3569.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i21.3569
Portopulmonary hypertension (PoPH) is characterized by pulmonary hypertension resulting from portal hypertension. It is not uncommon in patients waiting for liver transplantation (LT) and accounts for up to 10.4% in patients with advanced liver disease[1]. The diagnostic criteria for PoPH are portal hypertension (ascites, shunt, splenomegaly, with or without liver disease), mean pulmonary artery pressure (mPAP) > 25 mmHg, pulmonary artery wedge pressure (PAWP) < 15 mmHg and pulmonary vascular resistance (PVR) > 3 WU (240 dyn∙s/cm5)[2].
PoPH is classified into three levels based on mPAP: 25-35 mmHg indicates mild PoPH, 35-45 mmHg indicates moderate PoPH and more than 45 mmHg indicates severe PoPH. The pathogenesis of PoPH is still unclear. High dynamic circulation, an imbalance of endothelial vasoactive substances and portosystemic shunt may all be risk factors. Studies have shown that female gender or having an autoimmune liver disease increase the risk of PoPH[3]. A previous history of portosystemic shunt also increases the risk of PoPH[4]. There is no significant correlation between the severity of liver disease and PoPH. The prognosis in untreated PoPH patients is poor, and the 5-year survival rate can be as low as 14%, which is independent of the severity of portal hypertension and Child-Pugh grade[5].
LT can significantly improve the prognosis of PoPH patients; it was reported that the survival rate can reach 85.7% based on an average follow-up period of 7.8 years[6]. However, the risks involved in surgery rise sharply with increased PAP. The mortality following LT is reported to be 100% in patients with severe PoPH if mPAP ≥ 50 mmHg[7]. Therefore, mPAP ≥ 50 mmHg is regarded as an absolute contraindication for LT (mPAP ≥ 45 mmHg in some centers)[8,9]. However, the safety of LT can be greatly increased by reducing PoPH to a mild level by the administration of preoperative medication.
This study describes the diagnosis and treatment of a patient in our center with severe PoPH who underwent successful LT followed by a decrease in PAP without the need for long-term drug treatment.
A 39-year-old woman consulted our center with the complaints of intermittent abdominal pain for 7 years and exertional dyspnea with fatigue for 1 wk.
Seven years previously, she experienced intermittent abdominal pain. After visiting local hospitals, Caroli disease was diagnosed, but the disease has not been treated up to now. Approximately 1 wk before presenting at our center, she had gradually developed exertional dyspnea and limb weakness.
The patient had no other significant medical history. History of hypertension, diabetes, coronary heart disease and other chronic disease was denied.
The patient had no significant personal and family history.
Physical examination showed liver disease face with mild jaundice, poor nutrition, abdominal swelling and hepatosplenomegaly. She had mild tenderness in the right upper abdomen.
Laboratory examinations on admission revealed a hemoglobin level of 85 g/L, platelet count of 25 × 109/L, white blood cell count of 4.83 × 109/L and showed alanine aminotransferase 17 U/L, albumin 18.8 g/L, total bilirubin 135.80 µmol/L with direct bilirubin 78.75 µmol/L and creatinine 67.2 µmol/L. Her prothrombin time was 16.50 s, and the international normalized ratio was 1.43. Combined with imaging examination, her Child-Pugh score was C.
Abdominal ultrasonography and computed tomography revealed liver cirrhosis, portal hypertension with collateral circulation, splenomegaly, esophageal and gastric varices and ascites. Transthoracic echocardiography showed an estimated PAP of 132.94 mmHg.
Right heart catheterization (RHC) was further performed, and the measurements showed mPAP was 50 mmHg, PAWP was 20 mmHg and PVR was 460 dyn∙s/cm5. Portal pulmonary hypertension was suspected in this patient although her PAWP did not meet the diagnostic criteria. The patient had no previous history of heart disease or pulmonary disease. Her PAWP of 20 mmHg may have been due to poor liver function and fluid overload. Considering the high risk associated with LT, the patient was treated with Remodulin 0.825 ng/kg/min by subcutaneous infusion pump, which was increased by 0.4125 ng/kg/min every 2 d. In addition, diuretics were simultaneously added to reduce volume load. Two months later, RHC showed mPAP of 46 mmHg, PAWP of 9 mmHg and PVR of 470 dyn∙s/cm5. The patient was diagnosed with severe PoPH.
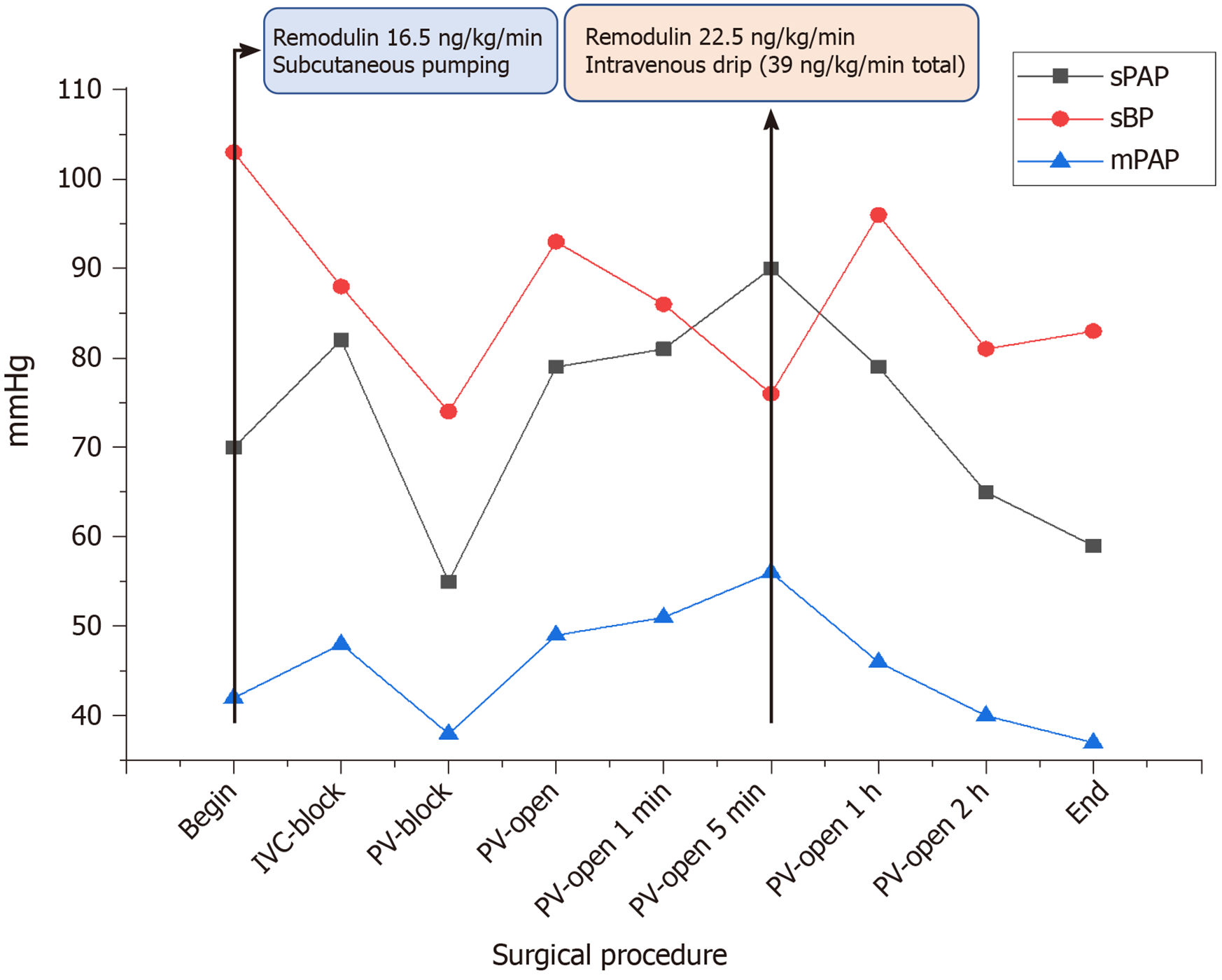
Remodulin was adjusted to 8.25 ng/kg/min, and tadalafil 30 mg/d was added. Three months after dose adjustment, RHC showed that mPAP had decreased to 37 mmHg, PAWP to 21 mmHg and PVR to 175 dyn∙s/cm5. PoPH was moderate, and she was placed on the transplant list because of her good response to drug therapy. The patient underwent LT 6 mo after treatment. Subcutaneous infusion of Remodulin was continued during surgery. The patient was stable in the beginning of surgery, but her PAP rose sharply exceeding the systemic circulation systolic pressure 5 min after the portal vein was opened. An emergency intravenous drip of Remodulin 15 ng/kg/min was administered and gradually increased to 22.5 ng/kg/min. This was combined with a continuous subcutaneous infusion of Remodulin, and the maximum dose was 39 ng/kg/min. The PAP decreased gradually, and systemic circulation pressure returned to normal (Figure 1). The operation was successfully completed.
Tadalafil was discontinued immediately after surgery and Remodulin was continued. Echocardiography was performed once every 1 mo or 2 mo to guide drug dose reduction to approximately 2 ng/kg/min/mo. The patient had good compliance, good drug tolerance and no serious side effects. One year after surgery, she completely discontinued medication and her systolic PAP fluctuated below 40 mmHg, which was near normal.
There are many reports on patients with PoPH treated by pharmacotherapy until LT can be performed. But few studies have focused on severe PoPH, and few patients with severe PoPH can totally discontinue medication[10-12]. We describe a patient with severe PoPH who successfully underwent LT and recovered well. The trend in perioperative pulmonary artery pressure changes and drug administrations are shown in Table 1.
| Before operation | After operation | |||||||
| 6 mo | 4 mo | 1 mo | 1 mo | 3 mo | 6 mo | 12 mo | 14 mo | |
| Remodulin1 (ng/kg/min) | 0.8 | 8.3 | 16.5 | 14.4 | 8.3 | 6.2 | 2.0 Withdraw | None |
| Combined drugs | Furosemide 20 mg qd; Spironolactone 20 mg bid | Tadalafil 30 mg qd | Tadalafil 30 mg qd | None | None | None | None | None |
| sPAP (mmHg) | 81.0 (133 by echocardiography) | 79.0 | 65.0 | 41.1 | 37.1 | 44.5 | 39.2 | 37.4 |
| mPAP (mmHg) | 50 | 46 | 37 | Unavailable2 | ||||
| PAWP (mmHg) | 20 | 9 | 21 | |||||
| PVR (dyn∙s/cm5) | 460 | 470 | 175 | |||||
Due to the high incidence of PoPH in patients on the LT waiting list and the high perioperative mortality rate, it is necessary to preliminarily evaluate PAP using echocardiography before LT. When pulmonary hypertension is suspected (systolic PAP > 50 mmHg or systolic PAP > 30 mmHg accompanied by symptoms of pulmonary hypertension), RHC should be carried out in a timely manner to confirm the diagnosis. When a patient is diagnosed with moderate to severe PoPH, pharmacotherapy should be initiated. Although prostacyclins, such as iloprost and treprostinil, have anti-platelet effects and may increase the risk of bleeding from esophageal and gastric varices, they are still considered first-line treatment due to their effectiveness. Oral endothelin receptor antagonists, such as bosentan and ambrisentan, with or without phosphodiesterase type 5 enzyme inhibitors, such as sildenafil, tadalafil and vardenafil, have also been shown to be effective[13,14]. Sildenafil monotherapy was reported to be effective in PoPH, but often the treatment lasts longer than a year[15]. That may increase mortality during the LT waiting period. Combining two oral drugs may shorten the treatment time, but it is still more than half a year[16]. Combination with prostacyclins usually can get better results in a shorter time, especially for severe PoPH[17]. A multicenter study carried out in France showed that preoperative combination therapy can significantly reduce perioperative mortality, and whether to use combination therapy was the only independent risk factor affecting prognosis[18]. RHC should be performed regularly to monitor PAP, and mPAP < 35 mmHg could be the criterion for inclusion in the transplantation list[19,20].
Intraoperative monitoring of PAP and the use of targeted drugs to reduce surgical risks are necessary. Intravenous Remodulin can be administered when there is a sharp increase in PAP during surgery. Depressurization drugs should be continued after the operation, and the dose should be reduced gradually. Postoperative PAP can be monitored by non-invasive transthoracic echocardiography.
The long-term prognosis of PoPH is unpredictable. In a United Kingdom study involving 28 patients with PoPH, the 3-year survival rate of five patients with severe PoPH was zero even after LT[21]. Therefore, the indications for LT in patients with PoPH should still be their primary liver disease, while for patients with PoPH alone, especially those with severe PoPH alone, LT is not recommended at present.
When patients with severe PoPH require LT, the success of LT can be greatly improved by reducing mPAP using depressurization pharmacotherapy, and LT may cure PoPH fundamentally.
We would like to thank En-Hui He, Rui-Fang Xu and Zhan-Xiong Yi who contributed to perioperative management and ultrasound monitoring in this patient.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cheungpasitporn W S-Editor: Ma YJ L-Editor: Filipodia E-Editor: Wu YXJ
| 1. | Cartin-Ceba R, Krowka MJ. Portopulmonary hypertension. Clin Liver Dis. 2014;18:421-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 2. | Humbert M, Sitbon O, Chaouat A, Bertocchi M, Habib G, Gressin V, Yaici A, Weitzenblum E, Cordier JF, Chabot F, Dromer C, Pison C, Reynaud-Gaubert M, Haloun A, Laurent M, Hachulla E, Simonneau G. Pulmonary arterial hypertension in France: results from a national registry. Am J Respir Crit Care Med. 2006;173:1023-1030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1271] [Cited by in RCA: 1288] [Article Influence: 67.8] [Reference Citation Analysis (0)] |
| 3. | Krowka MJ, Fallon MB, Kawut SM, Fuhrmann V, Heimbach JK, Ramsay MA, Sitbon O, Sokol RJ. International Liver Transplant Society Practice Guidelines: Diagnosis and Management of Hepatopulmonary Syndrome and Portopulmonary Hypertension. Transplantation. 2016;100:1440-1452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 298] [Article Influence: 37.3] [Reference Citation Analysis (0)] |
| 4. | Kawut SM, Krowka MJ, Trotter JF, Roberts KE, Benza RL, Badesch DB, Taichman DB, Horn EM, Zacks S, Kaplowitz N, Brown RS, Fallon MB; Pulmonary Vascular Complications of Liver Disease Study Group. Clinical risk factors for portopulmonary hypertension. Hepatology. 2008;48:196-203. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 220] [Cited by in RCA: 178] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 5. | Talwalkar JA, Swanson KL, Krowka MJ, Andrews JC, Kamath PS. Prevalence of spontaneous portosystemic shunts in patients with portopulmonary hypertension and effect on treatment. Gastroenterology. 2011;141:1673-1679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 57] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 6. | Swanson KL, Wiesner RH, Nyberg SL, Rosen CB, Krowka MJ. Survival in portopulmonary hypertension: Mayo Clinic experience categorized by treatment subgroups. Am J Transplant. 2008;8:2445-2453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 214] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 7. | Krowka MJ, Plevak DJ, Findlay JY, Rosen CB, Wiesner RH, Krom RA. Pulmonary hemodynamics and perioperative cardiopulmonary-related mortality in patients with portopulmonary hypertension undergoing liver transplantation. Liver Transpl. 2000;6:443-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 431] [Cited by in RCA: 357] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 8. | Savale L, Sattler C, Coilly A, Conti F, Renard S, Francoz C, Bouvaist H, Feray C, Borentain P, Jaïs X, Montani D, Parent F, O'Connell C, Hervé P, Humbert M, Simonneau G, Samuel D, Calmus Y, Duvoux C, Durand F, Duclos-Vallée JC, Sitbon O. Long-term outcome in liver transplantation candidates with portopulmonary hypertension. Hepatology. 2017;65:1683-1692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 69] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 9. | Krowka MJ, Wiesner RH, Heimbach JK. Pulmonary contraindications, indications and MELD exceptions for liver transplantation: a contemporary view and look forward. J Hepatol. 2013;59:367-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 85] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 10. | Sussman N, Kaza V, Barshes N, Stribling R, Goss J, O'Mahony C, Zhang E, Vierling J, Frost A. Successful liver transplantation following medical management of portopulmonary hypertension: a single-center series. Am J Transplant. 2006;6:2177-2182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 89] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 11. | Tan HP, Markowitz JS, Montgomery RA, Merritt WT, Klein AS, Thuluvath PJ, Poordad FF, Maley WR, Winters B, Akinci SB, Gaine SP. Liver transplantation in patients with severe portopulmonary hypertension treated with preoperative chronic intravenous epoprostenol. Liver Transpl. 2001;7:745-749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 59] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Bandara M, Gordon FD, Sarwar A, Knauft ME, Pomfret EA, Freeman RB, Wirth JA. Successful outcomes following living donor liver transplantation for portopulmonary hypertension. Liver Transpl. 2010;16:983-989. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 26] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Khaderi S, Khan R, Safdar Z, Stribling R, Vierling JM, Goss JA, Sussman NL. Long-term follow-up of portopulmonary hypertension patients after liver transplantation. Liver Transpl. 2014;20:724-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 14. | Raevens S, De Pauw M, Reyntjens K, Geerts A, Verhelst X, Berrevoet F, Rogiers X, Troisi RI, Van Vlierberghe H, Colle I. Oral vasodilator therapy in patients with moderate to severe portopulmonary hypertension as a bridge to liver transplantation. Eur J Gastroenterol Hepatol. 2013;25:495-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | Cheng CH, Wang YC, Wu TH, Lee CF, Wu TJ, Chou HS, Chan KM, Lee WC. Sildenafil Monotherapy to Treat Portopulmonary Hypertension Before Liver Transplant. Transplant Proc. 2019;51:1435-1438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Vionnet J, Yerly P, Aubert JD, Pascual M, Aldenkortt F, Berney T, Giostra E, Moradpour D, Schiffer E. Management of Severe Portopulmonary Hypertension With Dual Oral Therapy Before Liver Transplantation. Transplantation. 2018;102:e194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Serrano RM, Subbarao GC, Mangus RS, Montgomery G, Johansen M. Combination therapy for severe portopulmonary hypertension in a child allows for liver transplantation. Pediatr Transplant. 2019;23:e13461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Reymond M, Barbier L, Salame E, Besh C, Dumortier J, Pageaux GP, Bureau C, Dharancy S, Vanlemmens C, Abergel A, Woehl Jaegle ML, Magro P, Patat F, Laurent E, Perarnau JM. Does Portopulmonary Hypertension Impede Liver Transplantation in Cirrhotic Patients? A French Multicentric Retrospective Study. Transplantation. 2018;102:616-622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 19. | Ashfaq M, Chinnakotla S, Rogers L, Ausloos K, Saadeh S, Klintmalm GB, Ramsay M, Davis GL. The impact of treatment of portopulmonary hypertension on survival following liver transplantation. Am J Transplant. 2007;7:1258-1264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 112] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 20. | Bozbas SS, Eyuboglu FO, Arslan NG, Ergur FO, Karakayali H, Haberal M. The prevalence and the impact of portopulmonary hypertension on postoperative course in patients undergoing liver transplantation. Transplant Proc. 2009;41:2860-2863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | Verma S, Hand F, Armstrong MJ, de Vos M, Thorburn D, Pan T, Klinck J, Westbrook RH, Auzinger G, Bathgate A, Masson S, Holt A, Houlihan DD, Ferguson JW. Portopulmonary hypertension: Still an appropriate consideration for liver transplantation? Liver Transpl. 2016;22:1637-1642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |