Published online Jan 26, 2019. doi: 10.12998/wjcc.v7.i2.253
Peer-review started: October 29, 2018
First decision: November 15, 2018
Revised: December 19, 2018
Accepted: December 29, 2018
Article in press: December 30, 2018
Published online: January 26, 2019
Processing time: 89 Days and 23.5 Hours
Biliary papillomatosis (BP) is a rare disease characterized by multiple papillary adenomas in the intrahepatic and extrahepatic biliary tree and has a high risk of malignant transformation. Early diagnosis and treatment for BP are challenges, as it spreads along the biliary tract. A radical resection with an adequate resection margin is advocated in patients with malignant BP.
We report a case of BP with malignant transformation in a 52-year-old female patient who presented with emaciation, severe malnutrition, and a T-tube for biliary drainage that was placed for almost 2 years at the time she visited us. The enhanced magnetic resonance imaging of the upper abdomen revealed a neoplasm with a diameter of 15 cm located in the gallbladder area surrounding the common bile duct where a drainage tube was placed. It was the first case with malignant BP involving multiple organs and the abdominal wall and receiving a radical resection. Plastic surgeons helped close the incision by transferring the rectus muscle and external oblique muscle flap. A diagnosis of papillary carcinoma with diffuse malignant papillomatosis of the biliary duct was given. The postoperative course was uneventful and she was asymptomatic and in good physical condition at 35 mo postoperatively with appropriate chemotherapy.
Aggressive surgical treatment with appropriate chemotherapy is advocated for patients with malignant BP even if multiple organ invasion is present.
Core tip: Biliary papillomatosis (BP) is a rare benign tumour with a high risk of malignant transformation. Here, we report a case with malignant BP involving multiple organs and the abdominal wall and receiving a radical resection.
- Citation: Xiao Y, Zhao J, Wu H, Xie KL, Wan Y, Xu XW, Zhang YG. Surgical treatment of malignant biliary papillomatosis invading adjacent organs: A case report. World J Clin Cases 2019; 7(2): 253-259
- URL: https://www.wjgnet.com/2307-8960/full/v7/i2/253.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i2.253
Biliary papillomatosis (BP), first reported in 1959 by Caroli[1], is a rare disease of the biliary tract characterized by multiple papillary adenomas of the intra- and extra-hepatic biliary tree[2,3]. According to approximately 200 patients reported thus far[4], BP is more prevalent in patients aged 60 or 70 years, and the male to female ratio is approximately 2:1[5]. The pathogenesis of BP remains unclear; however, recurrent infections caused by cholestasis or clonorchiasis likely contribute to chronic inflammation and subsequent mucosal changes, consequently leading to BP[6]. The typical clinical manifestations of BP include recurrent abdominal pain, jaundice and cholangitis due to obstruction of the biliary tract by stones, mucus plugs, tumour detritus, and blood clots[7]. Whereas haemobilia is rare in the setting of BP[8], recurrent infections of the biliary tract may lead to secondary biliary cirrhosis and subsequent liver failure[9-12].
Although it is histologically classified as benign, BP was also considered to be a disease with malignancy potential, as a literature review indicated a high incidence of malignant transformation (approximately 41%)[5,13]. Because BP is a rare tumour that spreads along the biliary tract, early diagnosis, differential diagnosis, and management of the tumour are challenges for surgeons. We report our experience in treating a patient with BP malignant transformation invading adjacent organs and the abdominal wall.
Emaciation and severe malnutrition with a T-tube for biliary drainage placed for almost 2 years.
A 52-year-old female patient presented with emaciation and severe malnutrition and a T-tube for biliary drainage, which was placed for almost 2 years when she walked into our ward. She visited the local hospital 2 years ago because of obstructive jaundice with right epigastric pain for 3 mo. She underwent a cholecystectomy at the local hospital, which revealed a gallbladder filled with tumour-like tissue, leading to the diagnosis of gallbladder adenocarcinoma. A choledochoscopy showed a common bile duct (CBD) filled with adenomatoid tissue. After removing the tumour tissue, T-tube drainage was performed. Two months later, she came back to hospital to pull out the T-tube. A second choledochoscopy showed that the CBD was filled with adenomatoid tissue and biopsy showed severe dysplasia of the biliary papilloma. The patient and her family members felt hopeless and decided not to pursuit any further treatment. However, the patient still survived 2 years later and she came to us for help. She presented with severe malnutrition and recurrent infections with minimum haemoglobin and albumin of 3.7 g/dL and 2.8 g/dL, respectively.
Unremarkable.
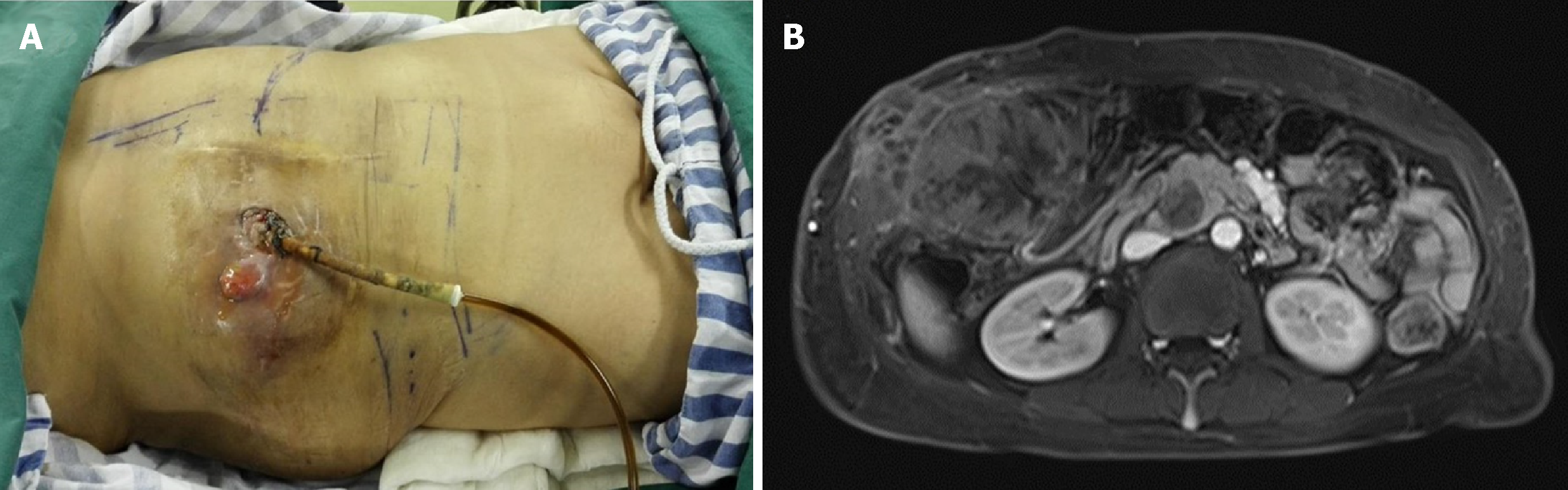
Physical examination showed that the skin surrounding the T-tube appeared with grey-white, hyperplastic granulation tissue with a stench (Figure 1A).
Haematological examination revealed an erythrocyte count of 2.38 × 1012/L and a haemoglobin level of 4.6 g/dL. Liver function tests showed an elevated alanine aminotransferase level of 66 IU/L and asparagine aminotransferase level of 42 IU/L. Bilirubin levels were normal, and hypokalemia was not observed. Tumour marker tests showed that carbohydrate antigen 19-9 was 731.3 U/mL and carcinoembryonic antigen was 4.36 ng/mL. Other tumour markers, including α-fetoprotein and cancer antigen 125, were normal. Tests for hepatitis B and C virus were negative.
The enhanced magnetic resonance imaging (MRI) of the upper abdomen revealed a neoplasm with a diameter of 15 cm locating in the gallbladder area surrounding the CBD where a drainage tube was placed (Figure 1B). The intra-hepatic bile duct was slightly dilated, while the extra-hepatic bile duct was obviously expanded. The skin biopsies suggested atypical glandular tissue which was considered as an adenocarcinoma originating from the biliary system.
We considered that her illness was malignant transformation of BP which was less aggressive than gallbladder adenocarcinoma and had a chance to be resected. Pathological diagnosis after operation was papillary carcinoma with diffused malignant papillomatosis of the biliary duct.
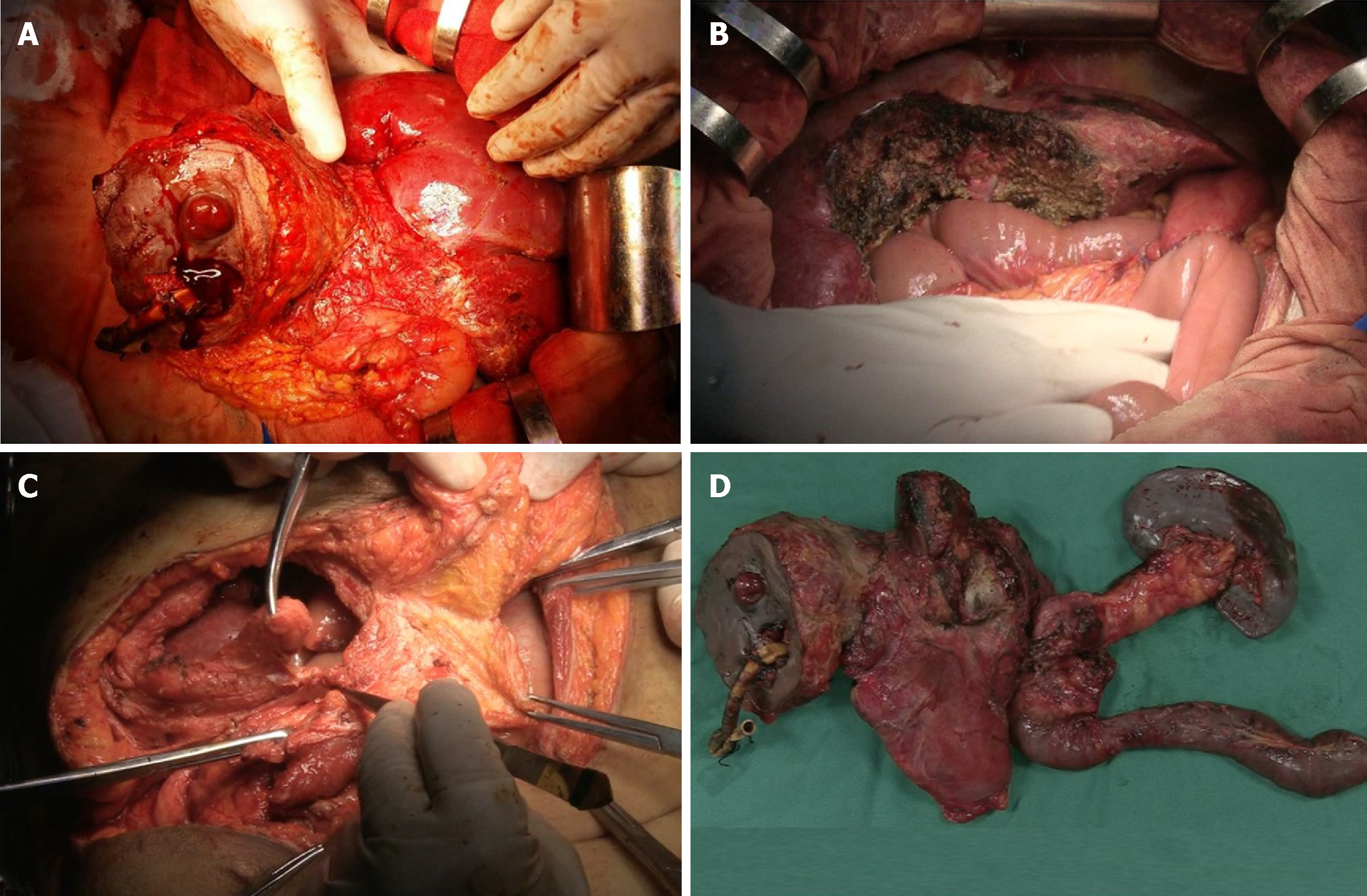
After the patient signed a consent form, an exploratory laparotomy using a left reverse L-shaped incision was performed. First, we dissociated the external oblique and rectus abdominis and reserved the flap. There was a mass with a size of 15 cm × 10 cm growing along the T-tube from the first hepatic portal to the abdominal wall (Figure 2A). Then, we opened the abdominal wall around the T-tube step by step and separated the dense adhesion between the retina, intestines, peritoneum, and liver in the abdominal cavity. The transverse mesocolon and gastrocolic ligament were dissociated. A surgical stapler was used to dissociate the stomach 5 cm away from the pylorus. An anterior approach was used to remove part of segments IVa and V of the liver to expose the left and right hepatic ducts. The CBD, duodenum, and spleen were dissected and removed. The pancreas was also removed because of tumour metastasis. Choledochojejunostomy, gastrointestinal anastomosis, and intestinal anastomosis were performed (Figure 2B). Plastic surgeons helped close the incision by transferring rectus abdominis and external oblique muscle flap (Figure 2C). After surgery, we dissected the specimen (Figure 2D) and found that a mass of grey sloughed-like tumour debris and mucus was discharged from the CBD and pancreatic duct.
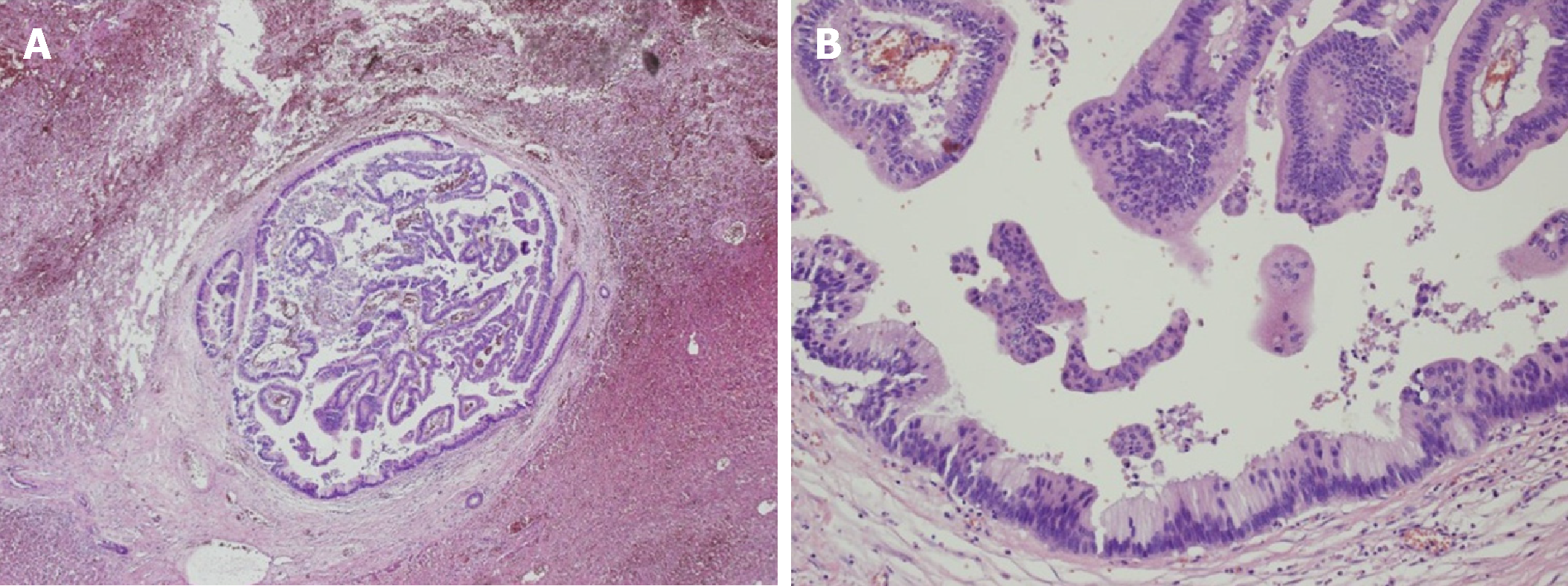
Histologic examination revealed a moderately differentiated carcinoma of the biliary system in the background of BP, and pathological diagnosis was papillary carcinoma with diffused malignant papillomatosis of the biliary duct (Figure 3). The tumour extensively invaded the pancreas, intra-hepatic bile duct, the whole wall of the stomach, and skin epidermis. No lymph node metastasis was found, and resection margins reached R0. The postoperative course was uneventful, and the patient was discharged on postoperative day 13. Two months later, the level of CA-199 decreased to 110.2 U/mL. She received adjuvant chemotherapy by oral administration of 40 mg tegafur, gimeracil, and oteracil potassium capsules (TGOP; Weikangda; Lunan Pharmaceutical Co., China) twice daily on days 1-28, every 2 wk for 7 months after half a year of radical surgery. However, with this treatment, the level of CA-199 still increased to 261.3 U/mL, which was considered to be a sign of disease progression, even though there was no evidence from a computerized tomography (CT) scan. The oncologist began to treat her by oral administration of 1000 mg capecitabine tablets (Xeloda; Luoshi Pharmaceutical Co., China) twice daily on days 1-14, every 3 wk for 12 mo. Twenty-five months after the surgery, a CT scan revealed metastases to bilateral lungs and MRI showed a metastasis in the abdominal cavity. She began to receive IROX regimen (intravenous injection of 100 mg oxaliplatin on day 1 and 160 mg irinotecan on day 1 followed by oral administration of 1000 mg capecitabine tablets once daily on days 1, every 4 wk) every 3 wk. After seven cycles of IROX regimen, there was no change of the metastases as shown on the CT image of the chest. However, abdominal CT showed the mass in the abdominal cavity increased to 7.8 cm in diameter. Thirty-three months after operation, she took 0.25 g apatinib mesylate tablets (Aitan; Hengrui Pharmaceutical Co., China) once daily. Thirty-five months after operation, most lesions of the pulmonary regressed. The abdominal mass decreased to 5.1 cm in diameter (Figure 4).
The patient was asymptomatic and in good physical condition at 35 mo postoperatively with appropriate chemotherapy.
BP is a rare papillary or villous tumour extending into the hepatic biliary tree. This tumour is mostly seen in middle-aged and elderly patients with a 2:1 ratio of males to females[6,13]. It may demonstrate dysplastic changes, as well as progression to carcinoma in situ and invasive adenocarcinoma[14]. The main clinical symptoms of BP are obstructive jaundice, abdominal pain caused by mucus secretion, and enlarging papilloma or tumour fragments, which eventually leads to biliary cirrhosis and liver failure[6,12,13,15]. However, early diagnosis is a challenge because BP does not present significant symptoms before the bile duct is completely blocked by the tumour. To the best of our knowledge, limited cases have been reported. This case is the first involving multiple organs and receiving a radical resection.
Preoperative diagnosis is usually difficult. It is absolutely difficult to differentiate BP from cholangiocarcinoma. While various diagnostic modalities have been used for the clinical diagnosis of BP, no special diagnostic or radiologic features have been described. Abdominal ultrasound and CT scan may reveal significant dilatation of the intra- and extrahepatic ducts, soft tissue densities in the dilated bile ducts, or thickened and enhanced bile duct walls but have limited use in terms of the differential diagnosis[10,13]. Endoscopic retrograde cholangiopancreatography (ERCP) can be a very useful diagnostic method that has the additional advantage of obtaining tissue for histological analysis[11]. ERCP with cholangioscopy with biopsy could give early diagnosis. Typical endoscopic characteristics include multiple undefined filling defects, irregular bile duct wall, excessive mucus discharge from the ampulla of the Vater, and reduced motility on irrigation. Intraoperative choledochoscopy can provide the extent of the disease involvement, but the final diagnosis must be confirmed by histopathological examination.
BP should be considered as a precancerous lesion with a high malignant potential, histologically ranging from dysplasia to carcinoma with biliary features[13]. In 2004, Lee et al[13] reviewed 58 cases of BP and reported that 83% of adenocarcinomas or mucinomas are malignant transformations from biliary adenomas. Yeung et al[5] reported a transformation rate of 42% in 78 patients, and only 55% of patients could undergo curative resection at diagnosis. In addition, depending on the presence or absence of mucin hypersecretion, BP is classified as one of two types, mucin-hypersecreting or non-mucin-producing. However, there is no significant difference in overall survival between the two types[13].
The treatment of BP is controversial due to a high local recurrence rate and frequent transformation to malignant tumours. It has been reported that when the lesions are localized, radical resection with an adequate resection margin can increase the 5-year survival rate to 81%[11,13]. Liver transplantation (LT) is the only curative treatment for patients with diffused BP[16]. Because the extra-hepatic biliary ducts are only partially removed in LT, a combination of LT and a Whipple operation may represent an effective treatment strategy for diffused lesions. However, LT is subject to insufficient donors and high medical costs, and radical resection is still the first choice for most patients with BP. In the current case, we showed that patients with malignant BP with multiple organs being invaded can also benefit from radical resection.
In conclusion, BP should be considered a premalignant disease with a high malignant potential. Aggressive surgical treatment with appropriate adjuvant chemotherapy is advocated for patients with malignant BP even if multiple organ invasion is present.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): E
P- Reviewer: Ahmed M, Hann HW, Jamali R, Karaca CA S- Editor: Ji FF L- Editor: Wang TQ E- Editor: Wu YXJ
| 1. | CAROLI J. [Papillomas and papillomatoses of the common bile duct]. Rev Med Chir Mal Foie. 1959;34:191-230. [PubMed] |
| 2. | Okulski EG, Dolin BJ, Kandawalla NM. Intrahepatic biliary papillomatosis. Arch Pathol Lab Med. 1979;103:647-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Kim YS, Myung SJ, Kim SY, Kim HJ, Kim JS, Park ET, Lim BC, Seo DW, Lee SK, Kim MH, Min YI. Biliary papillomatosis: clinical, cholangiographic and cholangioscopic findings. Endoscopy. 1998;30:763-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 42] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Gu C, Lin YE, Jin H, Jian Z. Biliary papillomatosis with malignant transformation: A case report and review of the literature. Oncol Lett. 2015;10:3315-3317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Yeung YP, AhChong K, Chung CK, Chun AY. Biliary papillomatosis: report of seven cases and review of English literature. J Hepatobiliary Pancreat Surg. 2003;10:390-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Nakanuma Y, Sasaki M, Ishikawa A, Tsui W, Chen TC, Huang SF. Biliary papillary neoplasm of the liver. Histol Histopathol. 2002;17:851-861. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 34] [Reference Citation Analysis (0)] |
| 7. | Imvrios G, Papanikolaou V, Lalountas M, Patsiaoura K, Giakoustidis D, Fouzas I, Anagnostara E, Antoniadis N, Takoudas D. Papillomatosis of intra- and extrahepatic biliary tree: Successful treatment with liver transplantation. Liver Transpl. 2007;13:1045-1048. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Sen I, Raju RS, Vyas FL, Eapen A, Sitaram V. Benign biliary papillomatosis in a patient with a choledochal cyst presenting as haemobilia: a case report. Ann R Coll Surg Engl. 2012;94:e20-e21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | White AD, Young AL, Verbeke C, Brannan R, Smith A, Prasad KR. Biliary papillomatosis in three Caucasian patients in a Western centre. Eur J Surg Oncol. 2012;38:181-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Vassiliou I, Kairi-Vassilatou E, Marinis A, Theodosopoulos T, Arkadopoulos N, Smyrniotis V. Malignant potential of intrahepatic biliary papillomatosis: a case report and review of the literature. World J Surg Oncol. 2006;4:71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Li Z, Gao C, Zhang X, He Z, Abm K, Biswas S, Niu J, Niu W. Intrahepatic biliary papillomatosis associated with malignant transformation: report of two cases and review of the literature. Int J Clin Exp Med. 2015;8:21802-21806. [PubMed] |
| 12. | Cheng MS, AhChong AK, Mak KL, Yip AW. Case report: two cases of biliary papillomatosis with unusual associations. J Gastroenterol Hepatol. 1999;14:464-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Lee SS, Kim MH, Lee SK, Jang SJ, Song MH, Kim KP, Kim HJ, Seo DW, Song DE, Yu E, Lee SG, Min YI. Clinicopathologic review of 58 patients with biliary papillomatosis. Cancer. 2004;100:783-793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 165] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 14. | Neumann RD, LiVolsi VA, Rosenthal NS, Burrell M, Ball TJ. Adenocarcinoma in biliary papillomatosis. Gastroenterology. 1976;70:779-782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 15. | Jiang L, Yan LN, Jiang LS, Li FY, Ye H, Li N, Cheng NS, Zhou Y. Biliary papillomatosis: analysis of 18 cases. Chin Med J (Engl). 2008;121:2610-2612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Dumortier J, Scoazec JY, Valette PJ, Ponchon T, Boillot O. Successful liver transplantation for diffuse biliary papillomatosis. J Hepatol. 2001;35:542-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |