Published online Sep 26, 2019. doi: 10.12998/wjcc.v7.i18.2864
Peer-review started: May 9, 2019
Revised: July 12, 2019
Accepted: July 27, 2019
Article in press: July 27, 2019
Published online: September 26, 2019
Processing time: 148 Days and 17.5 Hours
Bile duct polyps are difficult to diagnose and are usually excised by open abdominal surgery or snare polypectomy using choledochoscopy via the T-tube sinus tract. However, these two resection methods require the surgeon to open the abdomen and cut the bile duct to place the “T” tube. Moreover, simple snare polypectomy, without submucosal injection, can only remove pedunculated polyps and not flat polyps. Therefore, a new method is required for the excision of bile duct polyps, including flat polyps.
A 63-year-old woman was hospitalized following epigastric pain lasting a month. She had a 30-year history of cholelithiasis and had undergone cholecystectomy because of cholecystolithiasis, and had undergone cholangiolithotomy twice due to choledocholithiasis. Computed tomography (CT) and magnetic resonance imaging showed a communication between the bile duct and duodenal bulb. Inside the communication, CT showed a high-density shadow which was a hypointense lesion in T2 weighted image. The lesion showed no enhancement in T1 weighted image contrast enhanced. Gastroscopy revealed an incarcerated bile duct stone in the anterior wall of the duodenal bulb, which was removed with a basket under gastroscopy. Thereafter, a choledochoduodenal fistula was revealed. Finally, a flat polyp was detected in the lower part of the common bile duct and was removed by endoscopic mucosal resection (EMR) through the fistula. To our knowledge, this is the first reported case of the removal of a bile duct polyp using EMR.
EMR is a safe, effective, and low-cost method for the resection of all bile duct polyps.
Core tip: Bile duct polyps, including flat polyps, can be successfully resected by endoscopic mucosal resection (EMR). This method is safe, effective, and less invasive, with low pain, rapid rehabilitation, and low cost. Based on the literature search, this is the first reported case in the world on the resection of a bile duct polyp using EMR.
- Citation: Yang S, Yang L, Wang XY, Yang YM. Endoscopic mucosal resection of a bile duct polyp: A case report. World J Clin Casesol 2019; 7(18): 2864-2870
- URL: https://www.wjgnet.com/2307-8960/full/v7/i18/2864.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i18.2864
Bile duct polyps are difficult to diagnose by B-mode ultrasonography, computed tomography (CT), and magnetic resonance imaging (MRI); however, bile duct polyps can sometimes be detected during surgery of the biliary tract[1-3]. However, the definitive diagnosis of bile duct polyps requires cholangioscopy or use of the SpyGlass system[2,4-6]. Traditional open abdominal surgery and snare polypectomy by choledochoscopy via the T-tube sinus tract can be used to resect bile duct polyps[2,7]. However, these two methods require the surgeon to open the abdomen and cut the bile duct to place the “T” tube; consequently, these techniques are associated with several limitations, including increased trauma, pain, and cost[8]. Moreover, traditional snare polypectomy, without submucosal injection, can remove only pedunculated polyps of the bile duct, rather than flat polyps[9-11]. Consequently, there is an urgent need to develop a new technique for the removal of bile duct polyps, including flat polyps.
A 63-year-old woman was admitted into our hospital due to epigastric pain lasting one month. The pain radiated to the back and worsened after meals, but the patient did not present with fever, vomiting, or jaundice. In 1989, the patient was diagnosed with cholecystolithiasis following upper abdominal pain and underwent cholecystectomy. The patient was diagnosed with choledocholithiasis in 1991 and 2017, and underwent cholangiolithotomy twice.
Physical examination revealed multiple surgical scars and mild tenderness in the right upper abdomen, with no signs of rebound tenderness.
Routine blood tests, liver function tests, blood amylase, and tumor markers were normal.
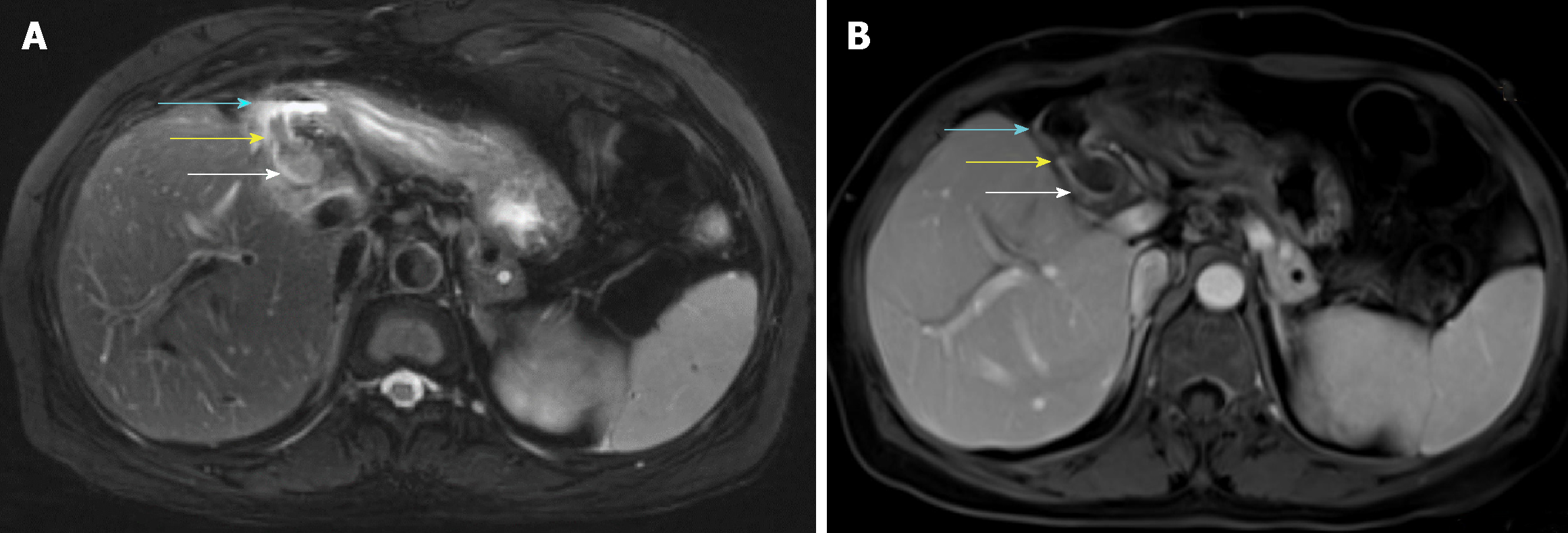
A CT report from the other hospital that the patient previously visited described a communication between the bile duct and duodenal bulb, as well as a high-density shadow inside the communication. On MRI, axial T2 weighted image (Figure 1A) showed dilatation of the bile duct, as well as a fistula connecting the bile duct and duodenal bulb. Inside the fistula, there was a hypointense lesion. Axial T1 weighted image contrast enhanced (Figure 1B) showed no enhancement of the lesion.
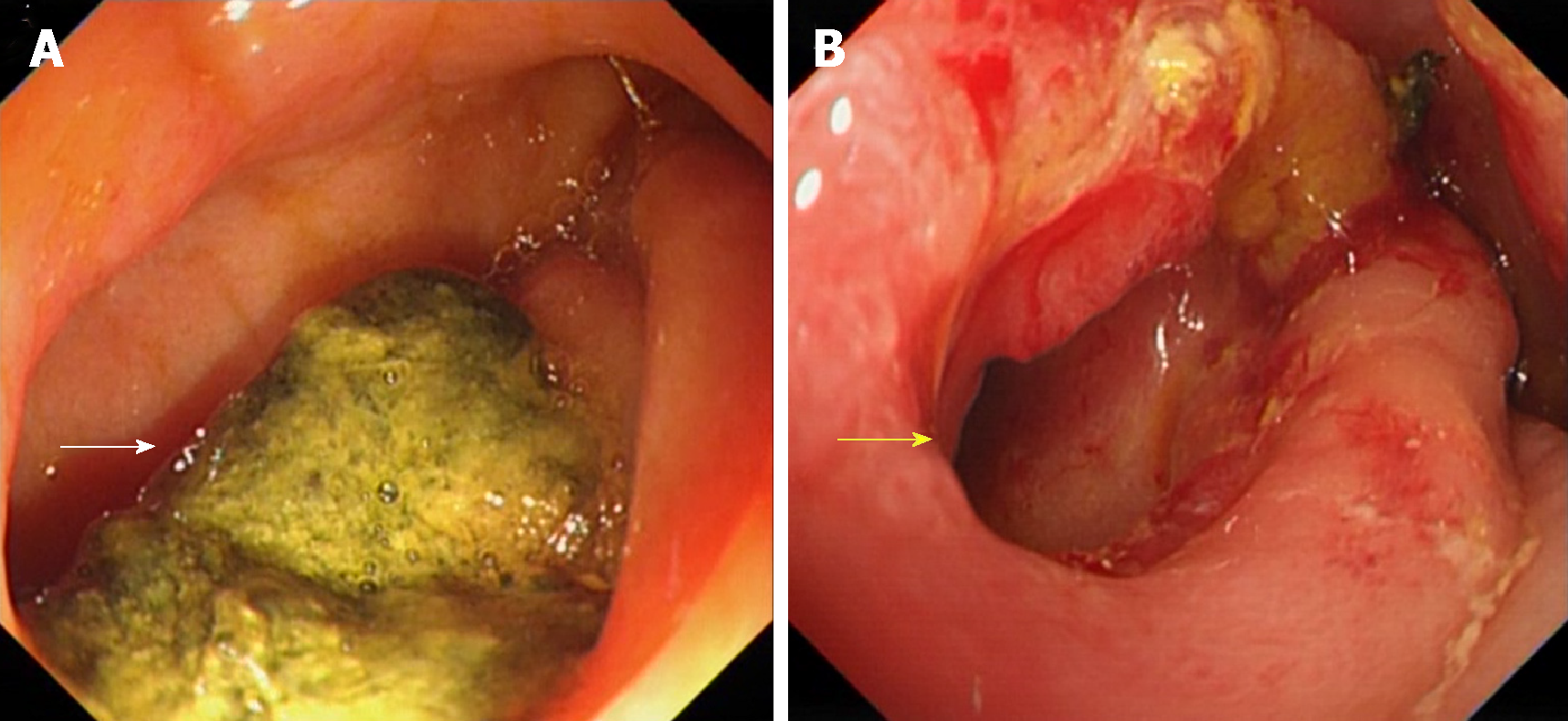
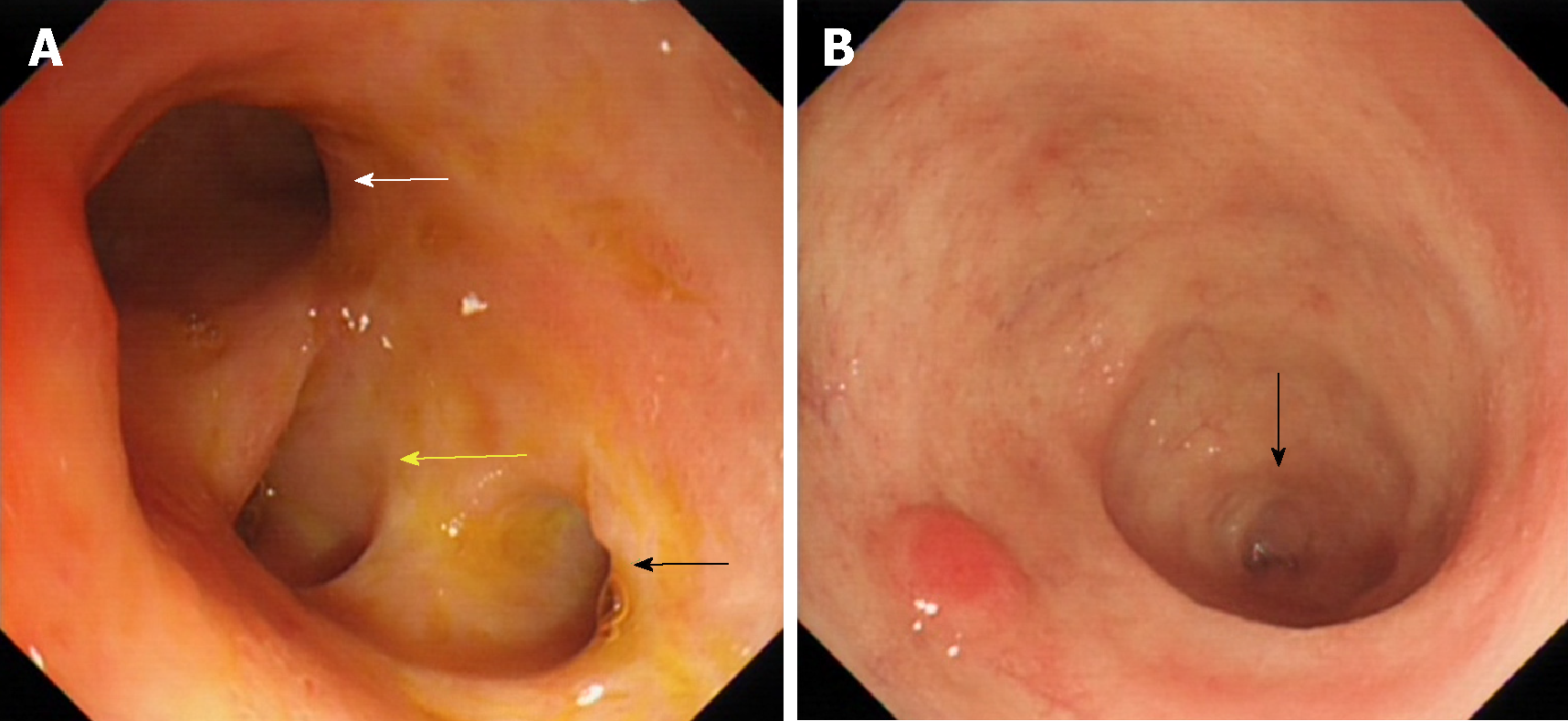
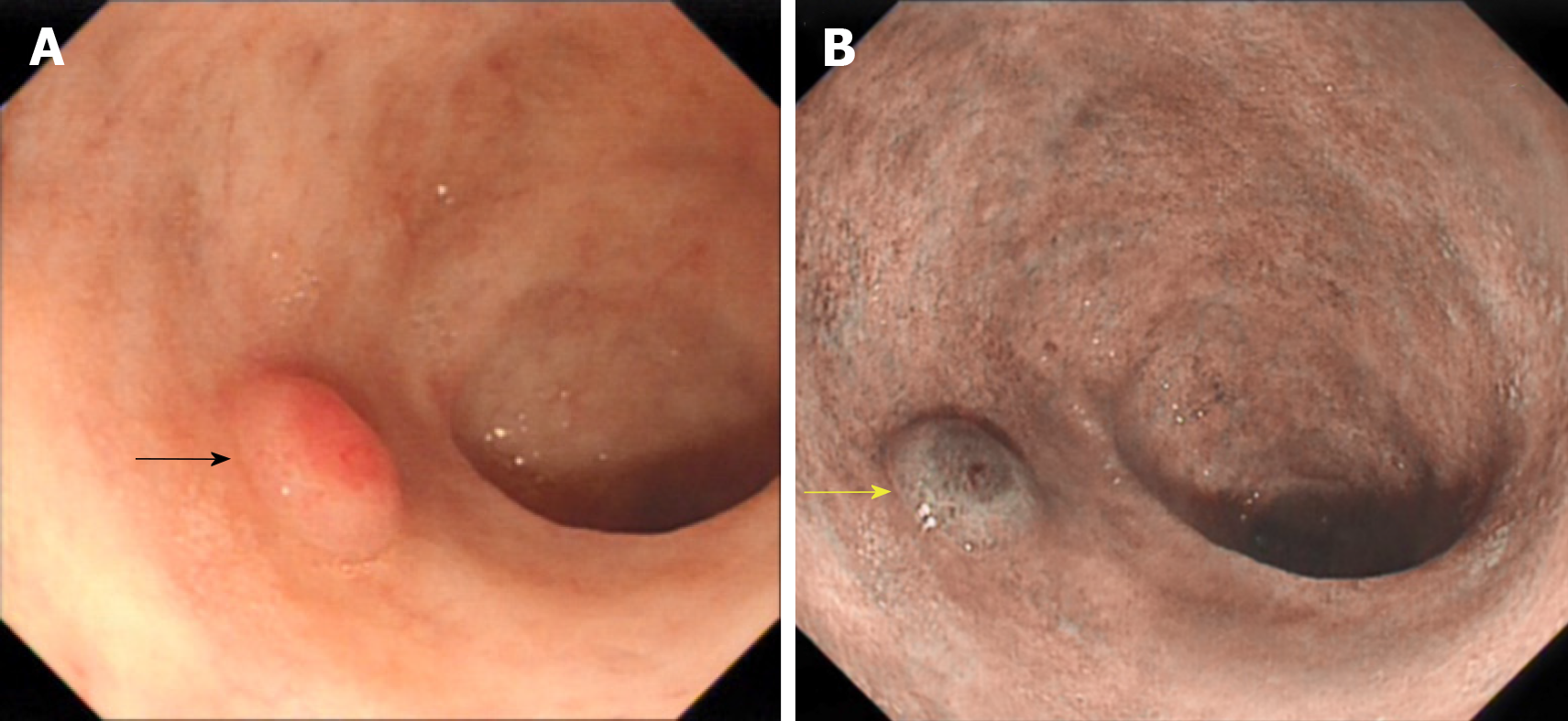
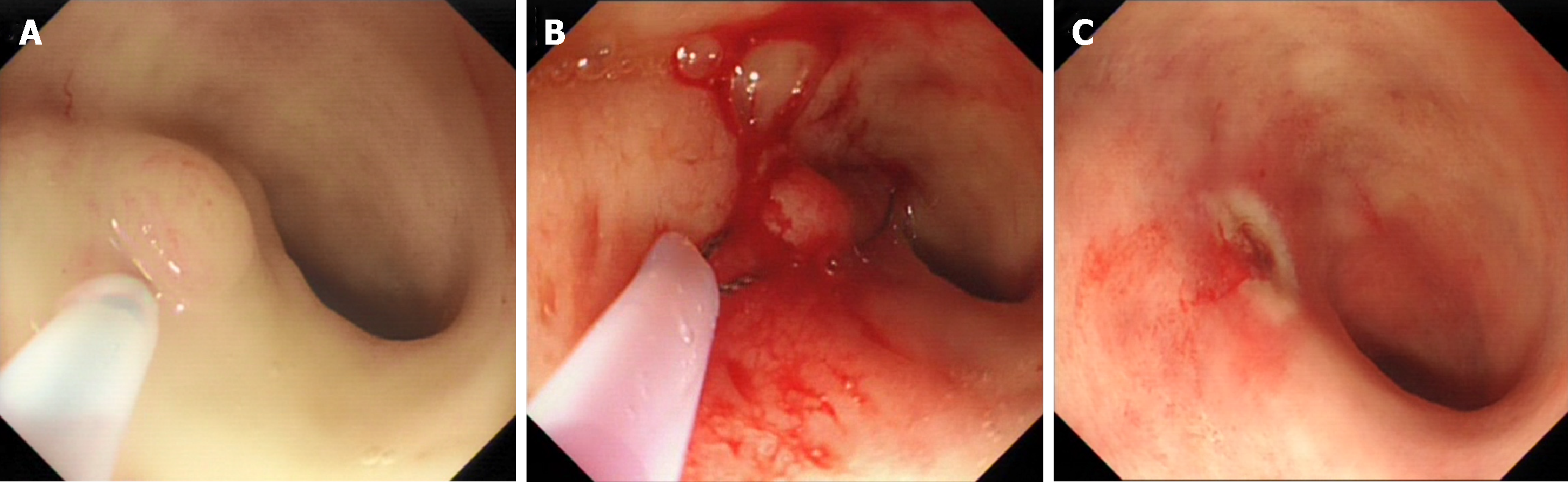
Gastroscopy revealed the presence of a bile duct stone incarcerated in the anterior wall of the duodenal bulb (Figure 2A). After the stone was removed with an MWB-2 X4 Memory Basket (Wilson-Cook Medical Inc., Winston-Salem, North Carolina, United States), we observed a fistula with a proximal diameter of 1.2 cm (Figure 2B). The bile duct in the hilar area was observed when the gastroscope was inserted upwards through the fistula (Figure 3A), and the terminal part of the common bile duct was observed when the gastroscope was inserted downwards (Figure 3B). A 0.4-cm flat protruded lesion was seen in the lower portion of the common bile duct. The surface of the lesion appeared red under white light (Figure 4A) and brown under narrow band imaging (Figure 4B). The descending duodenum and duodenal papilla were normal. Pneumatosis and dilatation of the intrahepatic and extrahepatic bile ducts were noted in the intraoperative plain abdominal radiography. Contrast agent was injected via the gastroscope into the bile duct through the fistula, but the observation was severely interfered due to pneumatosis.
Finally, the patient was diagnosed with choledocholithiasis, a choledochoduodenal fistula (CDF), and a common bile duct polyp.
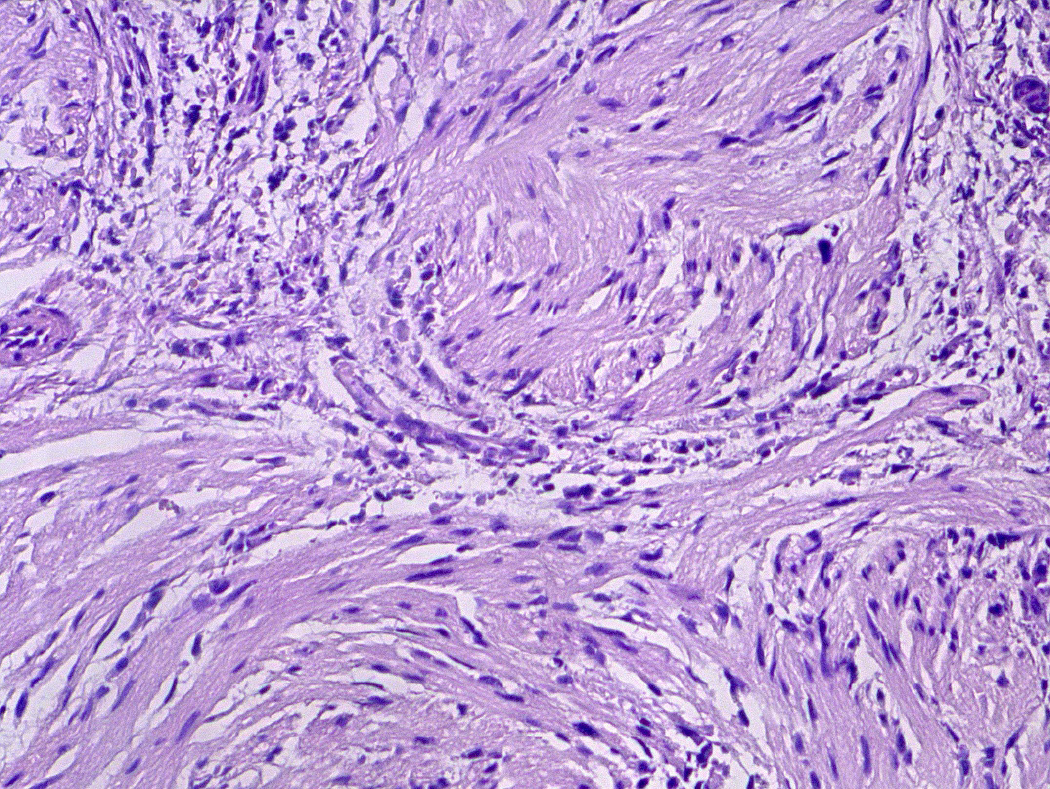
The incarcerated stone in the duodenal bulb was removed using the Memory Basket under gastroscopy. Thereafter, the gastroscope was inserted into the lower part of the common bile duct through the fistula. An Olympus NM-200l-0425 endoscopic injection needle (Olympus Medical Systems Corp., Hachioji-shi, Tokyo, Japan) was used to inject 0.9% normal saline containing epinephrine at a concentration of 1/100000 into the submucosa next to the polyp. Elevation of the lesion (the positive lifting sign) was observed upon submucosal injection (Figure 5A, Video). The lesion was encircled and removed using the OLYMPUS SD-210U-25 Electrosurgical Snare (Olympus Medical Systems Corp., Hachioji-shi, Tokyo, Japan) (Figure 5B and Figure 5C, Video). Finally, the tissue sample was sent for pathological examination; subsequent pathological diagnosis confirmed that it was an inflammatory fibroid polyp (Figure 6).
The patient experienced moderate postoperative abdominal pain, which disappeared 48 h later. No complications, including bleeding, perforation, and pancreatitis, were observed during the hospitalization. The patient was followed for 12 wk without discomfort or complications.
Among many causes of CDF, the most common causes are cholelithiasis, duodenal ulcer, and tumors[12,13]. In this case, the patient had a 28-year history of cholangiolithiasis, but showed no duodenal ulcer or gastrointestinal tumors. Therefore, the CDF in this patient was likely caused by the compression of stones on the bile duct wall and duodenal wall. This long-term compression could lead to necrosis and perforation of both bile duct wall and duodenal wall, resulting in CDF[12,13]. Epigastric pain, fever, and jaundice are common symptoms of CDF, depending on its location, whereas vomiting and diarrhea are relatively rare symptoms[12,13]. Pneumatosis of the bile duct on plain abdominal films and regurgitation of contrast on the upper gastrointestinal series can be observed in some patients[13-15]. In addition, fistulas can be found by CT and MRI in some cases. The fistulous orifice can be observed directly by gastroscopy and the CDF can be further confirmed by cholangiography. Notably, CDF patients with no symptoms or mild symptoms do not require treatment, whereas surgery is needed for those who experience repeated pain, fever, and jaundice[12,16].
Due to the low incidence rate and difficulty in diagnosis, bile duct polyps are rarely reported[2,7,17-19]. The precise cause of bile duct polyps has yet to be elucidated, although it is generally believed that long-term stimulation by cholangiolithiasis and chronic cholangitis is associated with the formation of bile duct polyps[20]. In this case, the patient had a 30-year history of cholelithiasis. Because most bile duct polyps exhibit neoplastic changes and can be cancerous, the early detection and resection of bile duct polyps can reduce the incidence of cholangiocarcinoma[21,22].
Bile duct polyps are often asymptomatic[2]. Bile duct polyps can lead to cholangiolithiasis, which can cause the bile duct to become obstructed; larger bile duct polyps can directly obstruct the bile duct[7,22]. Bile duct obstruction presents with specific symptoms, such as abdominal pain, fever, and jaundice[7]. However, B-mode ultrasound, CT, and MRI are limited in their ability to diagnose bile duct polyps, which are difficult to distinguish from cholangiocarcinomas[4]. Yet, bile duct polyps are often found during biliary surgeries, via choledochoscopy or the SpyGlass system[2-7].
The resection of bile duct polyps can be carried out by open abdominal surgery or snare polypectomy by choledochoscopy via the T-tube sinus tract[2,7]. However, these two methods require the surgeon to open the abdomen, make a cut in the bile duct, and finally place the “T” tube to establish the bile duct sinus tract. This can cause severe trauma and significant pain, and is associated with slow recovery, significant costs, and many other complications[8]. Moreover, simple snare polypectomy by choledochoscopy, without submucosal injection, can only resect pedunculated polyps, not flat polyps[9-11]. Endoscopic mucosal resection (EMR) was initially used for the excision of flat polyps, benign tumors, and early malignant tumors in the stomach and intestine[23]. However, resection of a proliferative lesion in the bile duct using EMR has not been attempted previously. In this case, we successfully resected the bile duct flat polyp through a CDF by gastroscopy with EMR. The patient recovered rapidly and had no postoperative complications. This indicated that this method is safe and effective, and has the advantages of limited trauma, reduced levels of pain, rapid recovery, and low cost. Moreover, to the best of our knowledge, this is the first ever reported case of a bile duct polyp being resected using EMR.
In future, with further miniaturization of the endoscopic needle and snare, we may also be able to use EMR in conjunction with the SpyGlass system to resect flat polyps in the bile duct, benign tumors of the bile duct, and early malignant tumors, thus opening up an exciting new avenue for the resection of proliferative lesions in the bile duct.
We successfully resected a flat polyp of the bile duct through a CDF by EMR under gastroscopy without complications. This is the first ever reported case of a bile duct polyp being resected using EMR. Collectively, our experiences with our patient show that this treatment strategy is safe and effective for the resection of bile duct polyps and offers many advantages over existing techniques, such as reduced levels of trauma and pain, rapid recovery, and reduced costs.
Manuscript source: Unsolicited manuscript
Received: April 29, 2019
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Sugimoto M, Lee HC S-Editor: Dou Y L-Editor: Wang TQ E-Editor: Zhou BX
| 1. | Dusunceli Atman E, Erden A, Ustuner E, Uzun C, Bektas M. MRI Findings of Intrinsic and Extrinsic Duodenal Abnormalities and Variations. Korean J Radiol. 2015;16:1240-1252. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Tang R, Zhao WP, Zhang YN, Tong X, Zeng JP. Cholesterol polyps in the distal common bile duct: a case report. Medicine (Baltimore). 2016;95:e5374. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Hamada Y, Maeshiro K, Nakayama Y, Nitta T. Extrahepatic bile duct polyp mimicking biliary parasitic disease. Endoscopy. 2012;44 Suppl 2 UCTN:E315-E316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Derdeyn J, Laleman W. Current role of endoscopic cholangioscopy. Curr Opin Gastroenterol. 2018;34:301-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 5. | Voiosu T, Ionita M, Voiosu A, Bengus A, Popp C, Mateescu B. Cholangioscopy using the SpyGlass system for a rare cause of obstruction: inflammatory polyp of the common bile duct. J Gastrointestin Liver Dis. 2017;26:111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | D'Souza LS, Korman A, Benias PC, Carr-Locke DL. A novel technique for biliary polypectomy. Endoscopy. 2017;49:E244-E245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Ezaki T, Okamura T, Yoshida Y, Kitamura M, Furuta A, Haratake J, Shirakusa T. A small polypoid lesion in the lower common bile duct: a case study. Endoscopy. 1994;26:271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Parra-Membrives P, Martínez-Baena D, Márquez-Muñoz M, Pino-Díaz V. Does laparoscopic approach impair T-tube-related sinus-tract formation? Surg Laparosc Endosc Percutan Tech. 2013;23:55-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Schwartz MP. Clip-assisted EMR: a new resection technique for treating flat remnants of colonic polyp tissue during piecemeal EMR. VideoGIE. 2018;3:403-405. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Sold M, Kähler G. Improved Techniques for Endoscopic Mucosal Resection (EMR) in Colorectal Adenoma. Viszeralmedizin. 2014;30:33-38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Wallace MB. Endoscopic Removal of Polyps in the Gastrointestinal Tract. Gastroenterol Hepatol (N Y). 2017;13:371-374. [PubMed] |
| 12. | Mallikarjunappa B, Ashish SR. Choledochoduodenal fistula: A rare case report with review of literature. JIMSA. 2013;26:226. |
| 13. | Akaydin M, Demiray O, Ferlengez E, Erozgen F, Ersoy YE, Er M. Importance of Spontaneous Choledochoduodenal Fistulas Detected During ERCP Procedure. Indian J Surg. 2018;80:216-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Dadzan E, Akhondi H. Choledochoduodenal fistula presenting with pneumobilia in a patient with gallbladder cancer: a case report. J Med Case Rep. 2012;6:61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Watanabe Y, Toki A, Todani T. Bile duct cancer developed after cyst excision for choledochal cyst. J Hepatobiliary Pancreat Surg. 1999;6:207-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 145] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 16. | Karincaoglu M, Yildirim B, Kantarceken B, Aladag M, Hilmioglu F. Association of peripapillary fistula with common bile duct stones and cholangitis. ANZ J Surg. 2003;73:884-886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Solakoglu T, Akin E, Yavuz SH, Ersoy O. Endoscopic treatment of a solitary hamartomatous polyp in the intrahepatic biliary duct. Endoscopy. 2013;45 Suppl 2 UCTN:E356-E357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Levy AD, Murakata LA, Abbott RM, Rohrmann CA. From the archives of the AFIP. Benign tumors and tumorlike lesions of the gallbladder and extrahepatic bile ducts: radiologic-pathologic correlation. Armed Forces Institute of Pathology. Radiographics. 2002;22:387-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 106] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 19. | Yang HL, Sun YG, Wang Z. Polypoid lesions of the gallbladder: diagnosis and indications for surgery. Br J Surg. 1992;79:227-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 146] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 20. | Zimmermann A. Reactive bile duct alterations mimicking biliary cancer: inflammatory conditions. Tumors and tumor-like lesions of the hepatobiliary tract. Cham: Springer 2017; 1-17. [DOI] [Full Text] |
| 21. | Kin Y, Nimura Y, Kamiya J, Kondo S, Nagino M. Cholesterosis in bile duct carcinoma. Gastrointest Endosc. 1994;40:92-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 22. | Lee CC, Wu CY, Chen GH. What is the impact of coexistence of hepatolithiasis on cholangiocarcinoma? J Gastroenterol Hepatol. 2002;17:1015-1020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 23. | Larghi A, Waxman I. Endoscopic mucosal resection: treatment of neoplasia. Gastrointest Endosc Clin N Am. 2005;15:431-454, viii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |