Published online Sep 26, 2019. doi: 10.12998/wjcc.v7.i18.2851
Peer-review started: April 8, 2019
First decision: June 10, 2019
Revised: July 26, 2019
Accepted: August 20, 2019
Article in press: August 20, 2019
Published online: September 26, 2019
Processing time: 169 Days and 20 Hours
Pancreaticoduodenal artery (PDA) aneurysms are extremely rare. The complicated clinical presentations and high incidence of rupture make it difficult to diagnose and treat. PDA pseudoaneurysms often rupture into the gastrointestinal tract and result in life-threatening gastrointestinal hemorrhage.
A 69-year-old man was admitted to our hospital due to right upward abdominal pain. A computed tomography (CT) scan demonstrated acute cholecystitis and cholecystolithiasis. Percutaneous gallbladder drainage was performed subsequently. He was discharged after 3 d and readmitted to hospital for cholecystectomy as arranged 1 mo later. A repeat CT scan revealed an emerging enhancing mass between the pancreatic head and the descending duodenum. Then, he suffered hematochezia and hemorrhagic shock suddenly. Emergency percutaneous angiogram was performed and selective catheterization of the superior mesenteric artery demonstrated a pseudoaneurysm in the inferior PDA. Coil embolization was performed and his clinical condition improved quickly after embolization and blood transfusion. He underwent laparoscopic cholecystectomy and was discharged from hospital after surgery under satisfactory conditions.
PDA pseudoaneurysms are uncommon. Acute haemorrhage is a severe complication of pseudoaneurysm with high mortality which clinicians should pay attention to.
Core tip: Pancreaticoduodenal artery (PDA) aneurysms are extremely rare, accounting for only 2% of all visceral artery aneurysms. PDA aneurysms are divided into pseudoaneurysms or true aneurysms. Pseudoaneurysms of the PDA that ruptured into the duodenum causing massive hemorrhage are rare and life-threatening. In this case, the patient was successfully treated with the accurate diagnosis and effective coil embolization. Clinicians should consider the possibility of ruptured pseudoaneurysms in patients with active gastrointestinal bleeding. The familiarity of this disease and appropriate treatments will save lives timely.
- Citation: Xu QD, Gu SG, Liang JH, Zheng SD, Lin ZH, Zhang PD, Yan J. Inferior pancreaticoduodenal artery pseudoaneurysm in a patient with calculous cholecystitis: A case report. World J Clin Cases 2019; 7(18): 2851-2856
- URL: https://www.wjgnet.com/2307-8960/full/v7/i18/2851.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i18.2851
Pancreaticoduodenal artery (PDA) aneurysms are extremely rare, accounting for only 2% of all visceral artery aneurysms[1]. PDA aneurysms are divided into pseudoaneurysms or true aneurysms. PDA pseudoaneurysms have been associated with pancreatitis, abdominal trauma, septic emboli, iatrogenic injuries, penetrating duodenal ulcers, and malignancies[2]. The complicated clinical presentations and high incidence of rupture make it difficult to diagnose and treat. They often rupture into the gastrointestinal tract and result in life-threatening gastrointestinal hemorrhage[3]. Here we report an interesting case of emerging PDA pseudoaneurysm in a patient after percutaneous cholecystostomy.
A 69-year-old man presented to the emergency department with severe right epigastric pain and vomiting.
The patient had experienced right epigastric pain repeatedly in recent 2 years. He has not been checked up in any other hospital before.
He underwent inguinal herniorrhaphy 10 years ago and without other medical history.
A significant personal or family medical history did not exist.
Clinical examination revealed tenderness and rebound pain in the upper abdomen. The Murphy’s sign was positive. A surgical scar of about 4 cm in length can be seen in each of the bilateral inguinal regions.
The results of laboratory examinations are as follows: white cell count, 28.80 × 109/L; neutrophil ratio, 91.99%; aspartate transaminase, 123 U/L; alanine aminotransferase, 104 U/L; glutamyl transpeptidase, 116 U/L; albumin, 27.20 g/L; direct bilirubin, 12.70 μmol/L; C-reactive protein, 217.00 mg/L; CA125 (OVL), 65.03 U/mL; CA199 (GIIUO), 46.30 U/mL; and amylase, 47 U/L.
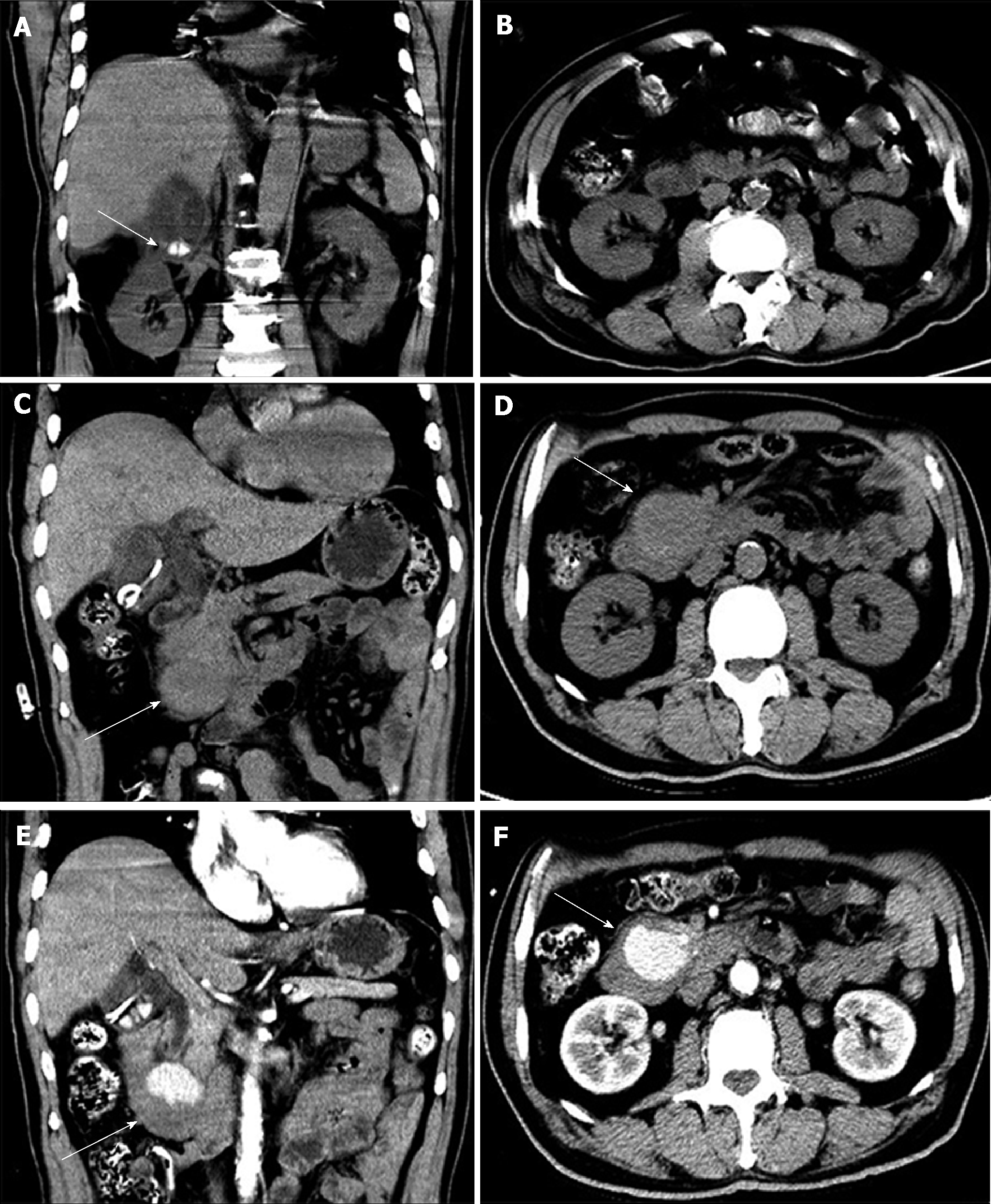
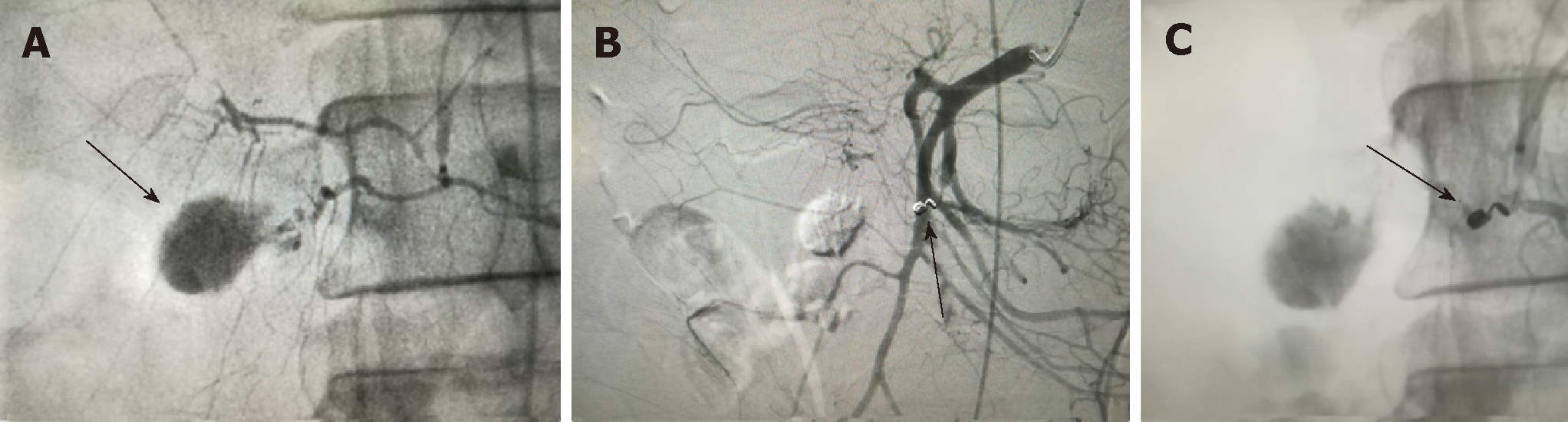
A computed tomography (CT) scan demonstrated acute cholecystitis and cholecystolithiasis (Figure 1A and 1B). In view of the patient’s poor clinical condition, percutaneous gallbladder drainage instead of cholecystectomy was performed subsequently. He was discharged 3 d after percutaneous cholecystostomy and readmitted to hospital for cholecystectomy as arranged 1 mo later. However, a repeat CT scan of the abdomen revealed an emerging 3.8 cm × 3.9 cm × 3.0 cm mass between the pancreatic head and the third portion of the duodenum (Figure 1C and 1D). Contrast-enhanced CT suggested that the enhancing mass was probably a hematoma (Figure 1E and 1F). The patient suffered hematochezia and hemorrhagic shock suddenly the next day after CT scan. Emergency percutaneous angiogram was performed and selective catheterization of the superior mesenteric artery demonstrated a pseudoaneurysm in the inferior PDA (Figure 2A).
Digestive tract hemorrhage, hemorrhage of ruptured PDA pseudoaneurysm, and acute cholecystitis with stones.
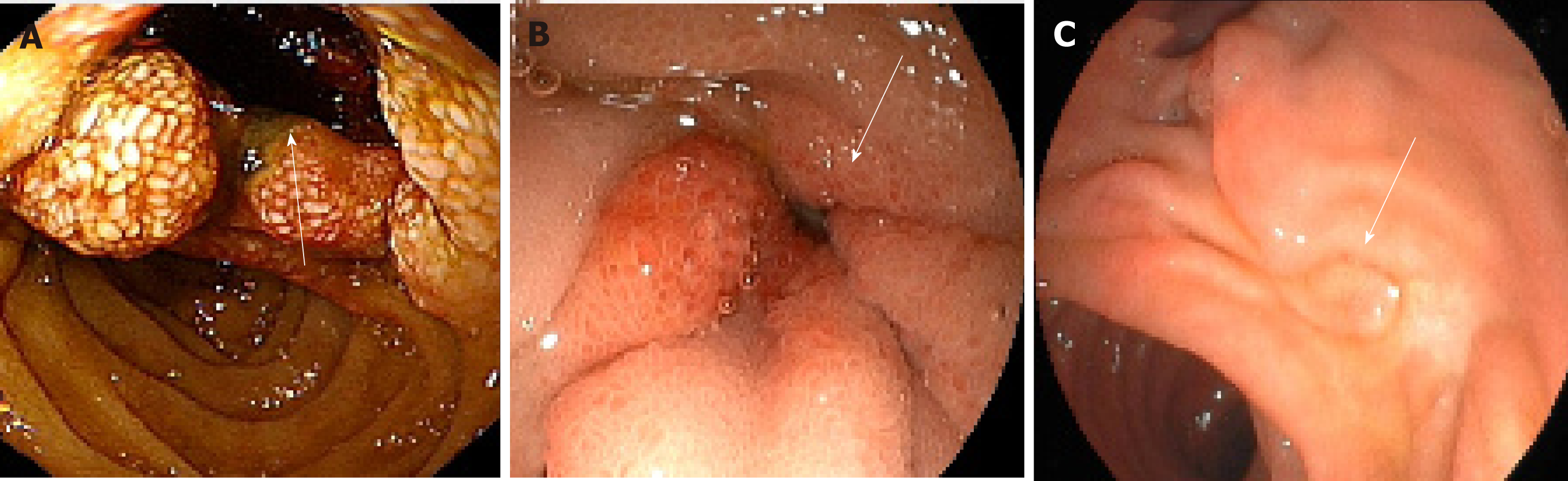
We performed coil embolization successfully (Figure 2B and 2C). The patient recovered well after embolization and blood transfusion. Subsequent gastroduodenal endoscopy revealed a 1.0 cm × 1.2 cm depressed lesion with blood clots in the third portion of the duodenum and the surrounding mucosa of the lesion swelled (Figure 3A). Repeated gastroduodenal endoscopy 5 d later showed that the lesion was reduced distinctly and the mucosa was congestive (Figure 3B). After his clinical condition was stable, he underwent laparoscopic cholecystectomy and was discharged from hospital after surgery under satisfactory conditions.
Two months after discharge, repeated gastroduodenal endoscopy showed that the lesion disappeared and the mucosa recovered (Figure 3C). He has been doing well without further complication for the last 6 mo.
Aneurysms of the splanchnic artery are extremely rare with an incidence of about 0.2% of the population[4]. PDA aneurysms account for 2% of all splanchnic artery aneurysms. They are usually asymptomatic. But when PDA aneurysms rupture, the clinical manifestations may range from non-specific abdominal pain to gastrointestinal hemorrhage and hemorrhagic shock. PDA pseudoaneurysms can occur after pancreatitis, abdominal trauma, septic emboli, iatrogenic injuries, penetrating duodenal ulcers, and malignancies, and they often rupture into the gastrointestinal tract[2,3]. However, true aneurysms of the PDA are usually associated with coeliac axis stenosis, and rupture into the retroperitoneal space[5]. Hemorrhage results from PDA pseudoaneurysms is a fatal complication. The mortality has been reported as greater than 25%[6]. Diagnosis of aneurysms can be made if the presence of an abdominal mass or bruit is found. Abdominal ultrasonography, CT, and magnetic resonance imaging are useful in detecting aneurysms. Angiography plays a vital role and is considered the gold standard for diagnosis of aneurysms. The risk of rupture of PDA aneurysms is not dependent on the size. Hence, it is advocated that all PDA aneurysms, regardless of size, should be treated actively once the diagnosis is established[7].
This case we reported here is really rare. The patient did not have a PDA pseudoaneurysm at first while an emerging PDA pseudoaneurysm was found by accident 1 mo later. It is hard to explain the pathogenesis of PDA pseudoaneurysm in this patient in such a short time. Although most of PDA pseudoaneurysms are due to pancreatitis and trauma, this patient did not exhibit acute or chronic pancreatitis and he did not undergo blunt or penetrating abdominal trauma. The pseudoaneurysms of the cystic artery and hepatic artery secondary to cholecystitis or percutaneous intervention of biliary tract have been reported[8,9]. However, no studies have showed the relationship between calculous cholecystitis or interventional procedures of the biliary tract and PDA pseudoaneurysms.
The major treatments for pseudoaneurysms consist of surgery or angiographic embolisation. Surgery used to be the accepted gold standard for treatment of pseudoaneurysms. Angiography plays a crucial role in making accurate diagnosis, with the additional benefit of therapy in some cases[10]. For example, once the source of hemorrhage is identified on angiography, percutaneous transcatheter angiographic embolization is recommended in hemodynamically stable patients. Compared with surgery, endovascular embolization is a less invasive and shorter procedure with a good success rate and associated with a shorter hospital stay[11]. However, the risk of endovascular interventions should be considered. Reported complications include migration of coils, aneurysmal rupture, aneurysmal reperfusion, inadvertent occlusion of other vessels, and infection[7].
Pseudoaneurysms of the PDA that rupture into the duodenum causing massive hemorrhage are rare and life-threatening. In this case, the patient was successfully treated with the accurate diagnosis and effective coil embolization. Clinicians should consider the possibility of ruptured pseudoaneurysms in patients with active gastrointestinal bleeding. The familiarity of this disease and appropriate treatments will save lives timely.
In conclusion, we have reported a rare case of a patient who did not have a PDA pseudoaneurysm at first while an emerging PDA pseudoaneurysm was found by accident 1 mo after percutaneous gallbladder drainage. The pseudoaneurysms of the PDA ruptured into the duodenum, causing life-threatening hemorrhage. The patient was successfully treated by effective coil embolization. The report of this case may arise awareness among clinicians regarding psuedoaneurysms as a possible cause of gastrointestinal bleeding.
The authors sincerely thank Mr. Yu Zhang for his support and excellent assistance in this work.
Care checklist: The manuscript was prepared and revised according to the CARE 2016 Checklist.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Saliba G, Ricci G S-Editor: Dou Y L-Editor: Wang TQ E-Editor: Zhou BX
| 1. | Moore E, Matthews MR, Minion DJ, Quick R, Schwarcz TH, Loh FK, Endean ED. Surgical management of peripancreatic arterial aneurysms. J Vasc Surg. 2004;40:247-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 79] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 2. | Pasha SF, Gloviczki P, Stanson AW, Kamath PS. Splanchnic artery aneurysms. Mayo Clin Proc. 2007;82:472-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 217] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 3. | al-Jeroudi A, Belli AM, Shorvon PJ. False aneurysm of the pancreaticoduodenal artery complicating therapeutic endoscopic retrograde cholangiopancreatography. Br J Radiol. 2001;74:375-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Zhao J. Massive upper gastrointestinal bleeding due to a ruptured superior mesenteric artery aneurysm duodenum fistula. J Vasc Surg. 2008;48:735-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | de Perrot M, Berney T, Deléaval J, Bühler L, Mentha G, Morel P. Management of true aneurysms of the pancreaticoduodenal arteries. Ann Surg. 1999;229:416-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 101] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 6. | Yanagaki S, Yamamoto Y, Nagasawa T. Ruptured Pseudoaneurysm in the Inferior Pancreaticoduodenal Artery. Intern Med. 2016;55:3233-3234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Tulsyan N, Kashyap VS, Greenberg RK, Sarac TP, Clair DG, Pierce G, Ouriel K. The endovascular management of visceral artery aneurysms and pseudoaneurysms. J Vasc Surg. 2007;45:276-83; discussion 283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 399] [Cited by in RCA: 425] [Article Influence: 23.6] [Reference Citation Analysis (1)] |
| 8. | Tapnio RH, Kolber MK, Shukla PA, Berkowitz E. Transcatheter Embolization of Cystic Artery Pseudoaneurysms Secondary to Acute Cholecystitis. Vasc Endovascular Surg. 2017;51:498-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 9. | Hangai S, Ohata A, Kageoka M, Mori M, Shimura T, Uozaki H, Shimamura T, Watanabe F, Maruyama Y. Successful transarterial embolization for recurrent pseudoaneurysm of the right hepatic artery with acute cholecystitis. Clin J Gastroenterol. 2014;7:164-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Chen HL, Chang WH, Shih SC, Wang TE, Yang FS, Lam HB. Ruptured pancreaticoduodenal artery pseudoaneurysm with chronic pancreatitis presenting as recurrent upper gastrointestinal bleeding. Dig Dis Sci. 2007;52:3149-3153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Leong BD, Chuah JA, Kumar VM, Mazri MY, Zainal AA. Successful endovascular treatment of post-traumatic inferior pancreaticoduodenal artery pseudoaneurysm. Singapore Med J. 2008;49:e300-e302. [PubMed] |