Published online Sep 26, 2019. doi: 10.12998/wjcc.v7.i18.2838
Peer-review started: February 27, 2019
First decision: July 30, 2019
Revised: August 8, 2019
Accepted: August 25, 2019
Article in press: August 26, 2019
Published online: September 26, 2019
Processing time: 209 Days and 17.1 Hours
Femoral shaft fractures are a common type of fracture among adults and have high union rates. However, clinical decisions are difficult to make because of the different types of nonunions. Atrophic nonunion usually requires revision surgery combined with bone grafting. Furthermore, no study of teriparatide administration for femoral atrophic nonunion have been previously reported.
A 60-year-old woman had a right femoral shaft fracture due to a traffic accident, and she immediately underwent closed reduction and internal fixation surgery with an intramedullary nailing. However, after 6 mo of rehabilitation, the fracture site showed no signs of healing, and her condition was diagnosed as atrophic nonunion. Subsequently, teriparatide was administered for 6 mo. Complete union was observed at the fracture site 6 mo after teriparatide discontinued.
The use of teriparatide can be a promising treatment to improve the healing of nonunion fractures.
Core tip: This is the first report describing the treatment of femoral shaft atrophic nonunion after an operative reduction and internal fixation procedure using only teriparatide administration instead of revision surgery. Our data provides an alternative treatment option for patients with atrophic nonunion.
- Citation: Tsai MH, Hu CC. Teriparatide as nonoperative treatment for femoral shaft atrophic nonunion: A case report. World J Clin Cases 2019; 7(18): 2838-2842
- URL: https://www.wjgnet.com/2307-8960/full/v7/i18/2838.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i18.2838
Femoral shaft fractures are some of the most common fractures that account for 5%-6% of long bone fractures in adults. Reamed intramedullary nailing (RIN) is considered the gold standard treatment for femoral shaft fractures[1]. Union rates as high as 98%-99% have been reported with RIN[2-4].
The United States Food and Drug Administration (FDA) defines nonunion as a fractured bone that has not completely healed within 9 mo from injury and that has not shown progression towards healing over 3 consecutive months, as determined from serial radiographs[5]. There are different types of nonunion. Hypertrophic nonunion develops as a result of insufficient mechanical stability and can lead to over-formation of a callus in the area of the fracture. Atrophic nonunion often involves insufficient vascularity of the defect gap and surrounding bone, leading to atrophy of the fracture ends[6].
The multi-factorial causes of delayed fracture healing warrant a specific therapy for each patient. Consequently, the so-called diamond concept has been established. It is composed of five different factors, including osteoconductive scaffolds, vascularity, growth factors, osteogenic cells, and mechanical environment, all of which must be analyzed for therapy. Based on the diamond concept, the first priority for the management of hypertrophic nonunion is to optimize mechanical stability. In the case of unstable osteosynthesis, re-osteosynthesis is necessary to enhance mechanical stability. Furthermore, re-osteosynthesis and additional biological activation of bone regeneration are often necessary for the treatment of atrophic nonunion[6,7]. Based on the current gold standard treatment for atrophic nonunion, revision of fixation with osteoconduction (scaffolds and mechanical environment) and osteoinduction (bone grafts, bone morphogenic protein, and vascularity) is necessary. Nonetheless, we report a patient who was treated with teriparatide, which is a recombinant protein form of parathyroid hormone. It is an effective anabolic agent used in the treatment of some forms of osteoporosis. Teriparatide is also occasionally used off-label to speed fracture healing and has been reported to improve callus volume, mineralization, bone mineral content, rate of successful union, and strength at fracture sites[8]. Furthermore, teriparatide treatment can aid fracture healing in osteoporotic women and people with atypical femoral fracture[9,10].
A 60-year-old woman presented to Dr. Hu’s clinic of our hospital and complaining of pain in her right lower extremity during weight-bearing.
The patient reported persistent pain for the past 6 mo since the operation in April 2016.
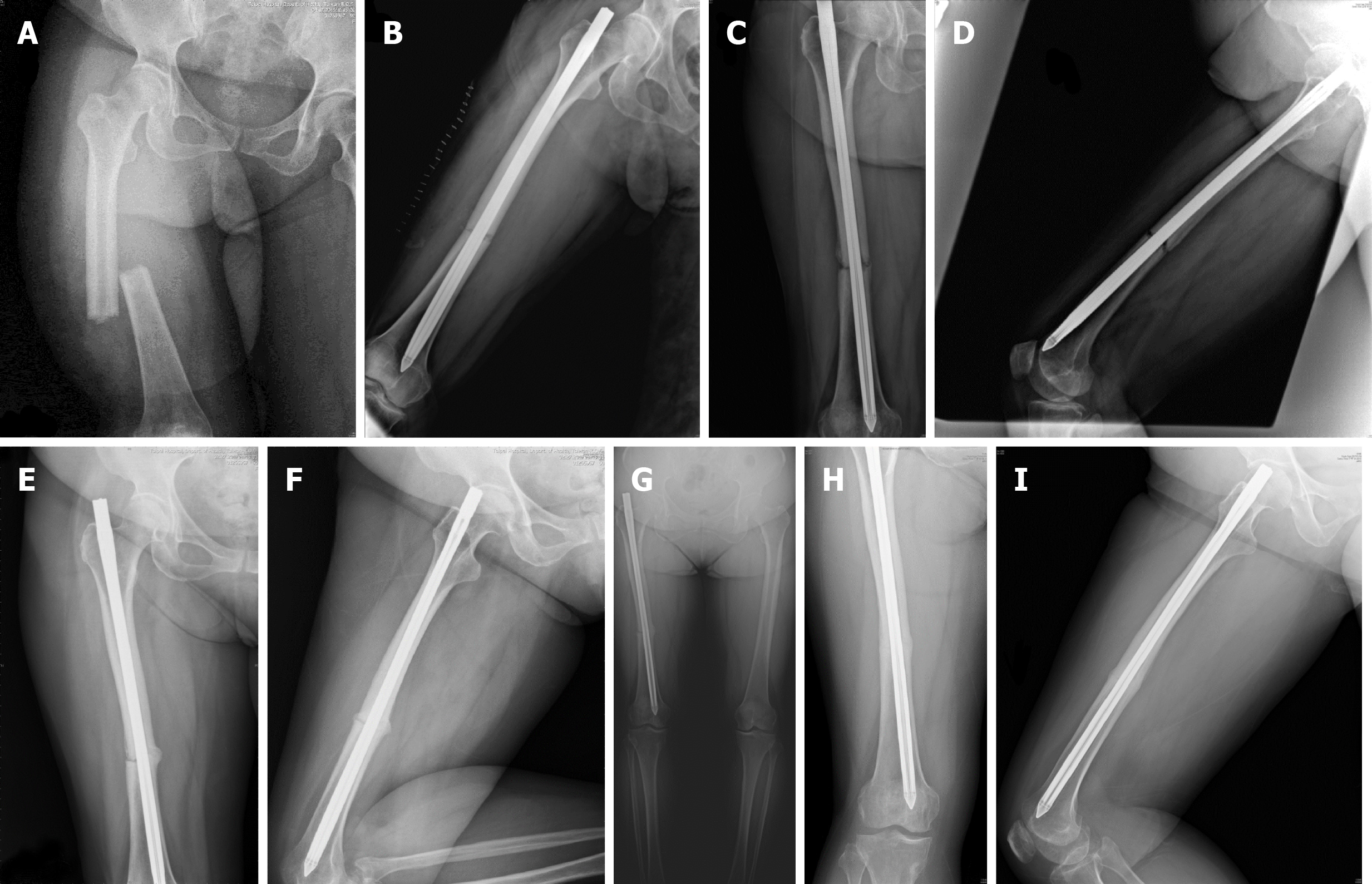
The patient was diagnosed with a right femoral shaft fracture due to a traffic accident, wherein she was the motorbike rider and was hit by a vehicle. She was immediately transported to the emergency room at a local hospital, where the femoral shaft fracture was identified without any other associated injuries; therefore, she underwent surgery consisting of closed reduction and internal fixation with an intramedullary nail (Fixion expandable nail, Disc-O-Tech, Tel Aviv, Israel) in April 2016 (Figure 1A and B).
The patient had a free personal and family history. She also denied long term medication history or glucocorticoid exposure.
On physical examination, the only positive finding was pain in the right lower extremity during weight-bearing over the middle thigh and buttock.
Laboratory examinations included white blood cell counts, C-reactive protein levels, erythrocyte sedimentation rate, serum alkaline phosphatase, parathyroid hormone, creatinine, albumin-corrected calcium, phosphate, and vitamin D level revealed all within normal range.
The final diagnosis of the presented case was right femoral shaft atrophic nonunion.
We carefully discussed treatment options with the patient; she refused to undergo further surgery, such as exchange nailing, augmentation plate fixation, or cancellous bone graft augmentation surgery. Instead, consent was given to an empirical therapy with teriparatide at approved doses for the treatment of osteoporosis (20 μg/d), as an attempt to treat the potential osteoporotic change and the atrophic nonunion of the femur.
After three months, X-ray images showed the presence of bone bridges and a decreased fracture gap between fragments. We also noticed that the treatment had increased the bone density at the fracture site (Figure 1E and F).
Five months after the initiation of the teriparatide treatment, radiographs revealed continuous improvements in fracture gap reduction and bone bridging at the circumferential fracture site (Figure 1G). Thus, the teriparatide treatment was discontinued 1 mo later.
Six months after the discontinuation of teriparatide, complete union was obtained, as observed in the radiographs, along with cortical remodeling (Figure 1H and I). The pain experienced by the patient disappeared, and she returned to normal activity, including returning to her job. No side effects attributable to the drug were observed during the treatment course.
Nonunion of femoral shaft fractures treated by RIN is uncommon. Union rates as high as 98%-99% have been reported with RIN, which is currently the standard management for closed fractures of the femoral shaft[2-4].
Nevertheless, some risk factors have been reported to be related to femoral shaft nonunion, including inaccurate reduction, unstable fixation, infection, alcohol abuse, advanced age, smoking, diabetes mellitus, corticosteroid treatment, use of non-steroidal anti-inflammatory drugs, and osteoporosis[6,11]. However, our patient did not have these risk factors.
Although teriparatide treatment has been reported as a successful treatment option for patients with nonunion of lower extremity fractures, those cases differed from ours in terms of some conditions. First, the patients reported by Lee et al[12], Xiaofeng et al[13] and Yu et al[14] all had some callus formation, as seen in the radiographs; hence, their fractures were classified as hypertrophic nonunions. Furthermore, all of their patients were successfully treated with teriparatide and achieved bone union[12-14]. Secondly, some patients received revision surgery before teriparatide use. One of the three patients reported by Lee et al[12] underwent a reoperation, in which the original 11-mm diameter nail was exchanged for a larger 13-mm nail. The patient reported by Yu et al[14] underwent another surgery, wherein the original intramedullary nail was exchanged for internal fixation using an anatomical plate together with autogenous bone graft. Two patients from Coppola et al[15] also underwent revision surgery: One patient underwent open reduction, fixation, and stabilization of the fracture with a mono-axial fixator supplemented with Allomatrix (Wright Medical Technology, Inc, Arlington, TN, United States), followed by open reduction and internal fixation with a condylar plate; while the other patient underwent open reduction with RIN. Thirdly, the fracture location of some cases also differed from our case. The case from the study by Giannotti et al[16] was an atrophic nonunion without revision surgery; however, the fracture location was over the distal femoral metaphysis. One of the three patients reported by Lee et al[12] had femoral neck fractures. Two patients from Coppola et al[15] experienced tibia and fibular fractures. Fourthly, the duration of teriparatide use also varied. The reported teriparatide treatments at 20 μg/d for 3-9 mo resulted in successful union in all 10 patients without further surgical intervention. All these reported cases showed adequate bone callus over the nonunion site and achieved clinical evidence of solid union[12-16].
Compared to these reported cases, our patient had atrophic nonunion of a femoral shaft fracture at 6 mo post-RIN without revision surgery, and was treated with teriparatideat 20 μg/d for 6 mo. This differed from the other previously reported patients with hypertrophic nonunion, revision surgery, femoral metaphyseal, or neck fracture, all with varied durations of teriparatide treatment. Based on the present review and our case, teriparatide is useful for the treatment of atrophic and hypertrophic nonunion with therapy durations ranging from 3 to 9 mo, regardless of whether revision surgery was performed.
The standard treatment for atrophic nonunion due to failed RIN is augmented plating with transplantation of autologous cancellous bone, or reamer-irrigator-aspirator combined with BMPs[6,17]. Nevertheless, not all cases of nonunion can be treated surgically because of either patient or technical factors. Thus, we reported the use of teriparatide as an alternative treatment to revision surgery for atrophic nonunion of femoral shaft fractures.
Our case demonstrated that atrophic nonunion of simple transverse femoral shaft fracture can be successfully treated with teriparatide for 6 mo, instead of revision surgery. Teriparatide administration can aid in improving the healing of nonunion fractures in patients not willing to undergo surgical intervention. Further well-designed prospective randomized controlled trials with larger patient groups are needed to assess the efficacy of teriparatide for the treatment of patients with nonunion of fractures.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: Taiwan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Francesco SM, Sahoo J, Yan SL, Vieyra JP S-Editor: Dou Y L-Editor: Wang TQ E-Editor: Qi LL
| 1. | Li AB, Zhang WJ, Guo WJ, Wang XH, Jin HM, Zhao YM. Reamed versus unreamed intramedullary nailing for the treatment of femoral fractures: A meta-analysis of prospective randomized controlled trials. Medicine (Baltimore). 2016;95:e4248. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 2. | Brumback RJ, Uwagie-Ero S, Lakatos RP, Poka A, Bathon GH, Burgess AR. Intramedullary nailing of femoral shaft fractures. Part II: Fracture-healing with static interlocking fixation. J Bone Joint Surg Am. 1988;70:1453-1462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 169] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 3. | Winquist RA, Hansen ST, Clawson DK. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. 1984. J Bone Joint Surg Am. 2001;83:1912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 47] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Xia L, Zhou J, Zhang Y, Mei G, Jin D. A meta-analysis of reamed versus unreamed intramedullary nailing for the treatment of closed tibial fractures. Orthopedics. 2014;37:e332-e338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 5. | Brinker M, Bruce D. Nonunions: evaluation and treatment. Browner, Jesse B. Jupiter, Alan M. Levine, Trafton PG editors. Skeletal trauma: basic science, management, and reconstruction. 3 ed. Bruce D. Philadelphia, USA: Saunders; 2003; . |
| 6. | Moghaddam A, Ermisch C, Schmidmaier G. Non-union current treatment concept. Int J Med Educa. 2016;3. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Moghaddam A, Zietzschmann S, Bruckner T, Schmidmaier G. Treatment of atrophic tibia non-unions according to 'diamond concept': Results of one- and two-step treatment. Injury. 2015;46 Suppl 4:S39-S50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 92] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 8. | Babu S, Sandiford NA, Vrahas M. Use of Teriparatide to improve fracture healing: What is the evidence? World J Orthop. 2015;6:457-461. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 38] [Cited by in RCA: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 9. | Lou S, Lv H, Wang G, Zhang L, Li M, Li Z, Zhang L, Tang P. The Effect of Teriparatide on Fracture Healing of Osteoporotic Patients: A Meta-Analysis of Randomized Controlled Trials. Biomed Res Int. 2016;2016:6040379. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 10. | Im GI, Lee SH. Effect of Teriparatide on Healing of Atypical Femoral Fractures: A Systemic Review. J Bone Metab. 2015;22:183-189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 57] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 11. | Bell A, Templeman D, Weinlein JC. Nonunion of the Femur and Tibia: An Update. Orthop Clin North Am. 2016;47:365-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 98] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 12. | Lee YK, Ha YC, Koo KH. Teriparatide, a nonsurgical solution for femoral nonunion? A report of three cases. Osteoporos Int. 2012;23:2897-2900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Xiaofeng L, Daxia X, Yunzhen C. Teriparatide as a nonoperative treatment for tibial and femoral fracture nonunion: A case report. Medicine (Baltimore). 2017;96:e6571. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Yu W, Guo X. Teriparatide treatment of femoral fracture nonunion that autogenous bone grafting failed to heal: a case report. Arch Osteoporos. 2017;12:15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Coppola C, Del Buono A, Maffulli N. Teriparatide in Fracture Non-Unions. Transl Med UniSa. 2014;12:47-53. [PubMed] |
| 16. | Giannotti S, Bottai V, Dell'Osso G, de Paola G, Pini E, Guido G. Atrophic femoral nonunion successfully treated with teriparatide. Eur J Orthop Surg Traumatol. 2013;23 Suppl 2:S291-S294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Somford MP, van den Bekerom MP, Kloen P. Operative treatment for femoral shaft nonunions, a systematic review of the literature. Strategies Trauma Limb Reconstr. 2013;8:77-88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 45] [Article Influence: 3.8] [Reference Citation Analysis (0)] |