Published online Sep 26, 2019. doi: 10.12998/wjcc.v7.i18.2658
Peer-review started: June 4, 2019
First decision: July 21, 2019
Revised: August 18, 2019
Accepted: August 27, 2019
Article in press: August 26, 2019
Published online: September 26, 2019
Processing time: 112 Days and 22.9 Hours
Five years have passed since the Japan Narrow Band Imaging Expert Team (JNET) classification was proposed in 2014. However, the diagnostic performance of this classification has not yet been established. We conducted a retrospective study and a systematic search of Medical Literature Analysis and Retrieval System On-Line. There were three retrospective single center studies about the diagnostic performance of this classification. In order to clarify this issue, we reviewed our study and three previous studies. This review revealed the diagnostic performance in regards to three important differentiations. (1) Neoplasia from non-neoplasia; (2) malignant neoplasia from benign neoplasia; and (3) deep submucosal invasive cancer (D-SMC) from other neoplasia. The sensitivity in differentiating neoplasia from non-neoplasia was 98.1%-99.8%. The specificity in differentiating malignant neoplasia from benign neoplasia was 84.7%-98.2% and the specificity in the differentiation D-SMC from other neoplasia was 99.8%-100.0%. This classification would enable endoscopists to identify almost all neoplasia, to appropriately determine whether to perform en bloc resection or not, and to avoid unnecessary surgery. This article is the first review about the diagnostic performance of the JNET classification. Previous reports about the diagnostic performance have all been retrospective single center studies. A large-scale prospective multicenter evaluation study is awaited for the validation.
Core tip: This is the first review of the Japan Narrow Band Imaging Expert Team classification regarding the diagnostic performance. There are three important differentiations: neoplasia from non-neoplasia, malignant neoplasia from benign neoplasia, and deep submucosal invasive cancer (D-SMC) from other neoplasia. The sensitivity in differentiating neoplasia from non-neoplasia was 98.1%-99.8%. The specificity in differentiating malignant neoplasia from benign neoplasia was 84.7%-98.2% and the specificity in differentiating D-SMC from other neoplasia was 99.8%-100.0%. This classification will enable endoscopists to identify almost all neoplasia, to appropriately determine whether to perform en bloc resection or not, and to avoid unnecessary surgery.
- Citation: Hirata D, Kashida H, Iwatate M, Tochio T, Teramoto A, Sano Y, Kudo M. Effective use of the Japan Narrow Band Imaging Expert Team classification based on diagnostic performance and confidence level. World J Clin Cases 2019; 7(18): 2658-2665
- URL: https://www.wjgnet.com/2307-8960/full/v7/i18/2658.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i18.2658
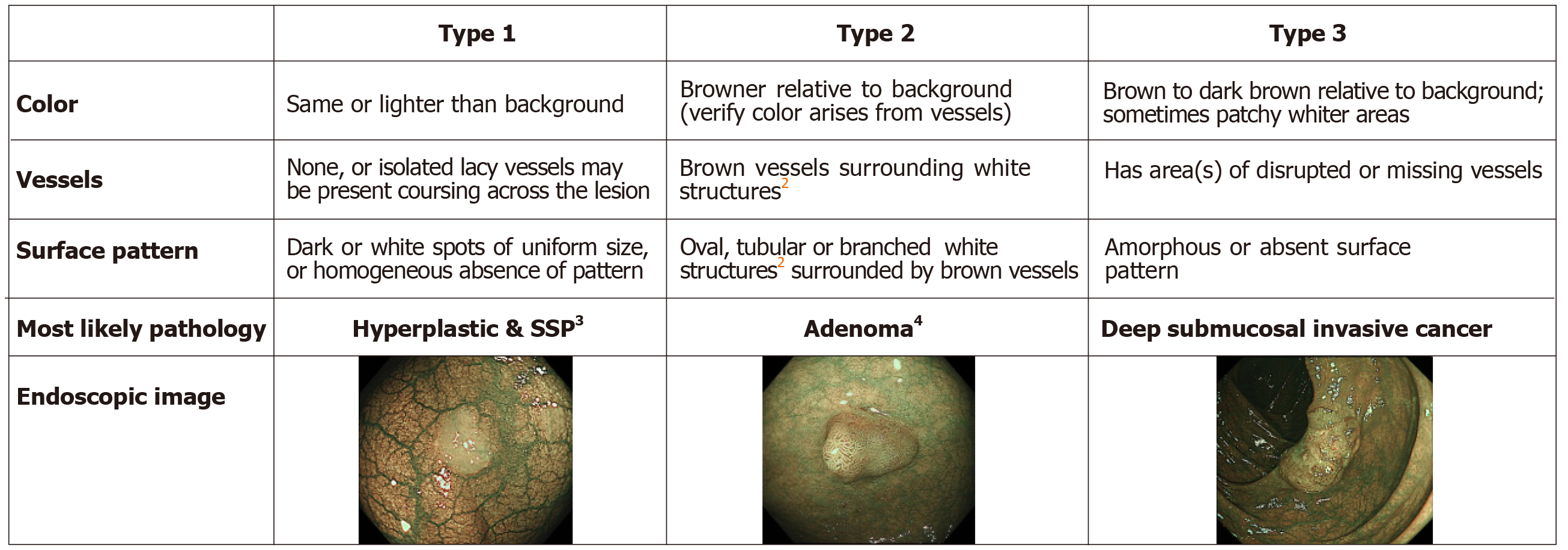
The Sano classification was proposed as the first Narrow Band Imaging (NBI) classification in 2006[1]. Following this, three classifications were proposed in Japan[2-4]. Colon Tumor NBI Interest Group proposed the Narrow Band Imaging International Colorectal Endoscopic (NICE) classification in 2009 (Figure 1). The NICE classification is easily applicable and can be used without magnification. However, previous validation studies revealed two problems with the NICE classification. One was that the confidence rate was reported to be only 50%-75%[5,6] though the diagnostic performance was acceptable in cases with high confidence. This means that the amount of polyps that can be diagnosed by the NICE classification is not high enough. The other problem was that endoscopists could not differentiate malignant neoplasia [high grade intramucosal neoplasia (HGIN) and invasive cancer] from benign neoplasia [low grade intramucosal neoplasia (LGIN)] using the NICE classification. This differentiation is clinically valuable for deciding treatment options because the invasion depth of malignant neoplasia should be evaluated by the specimen obtained en-bloc by endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD). In 2014, the Japan Narrow Band Imaging Expert Team (JNET) classification was published and showed the NBI diagnosis with magnification had the potential to increase the confidence rate and enable endoscopists to differentiate malignant neoplasia from benign neoplasia[7,8].
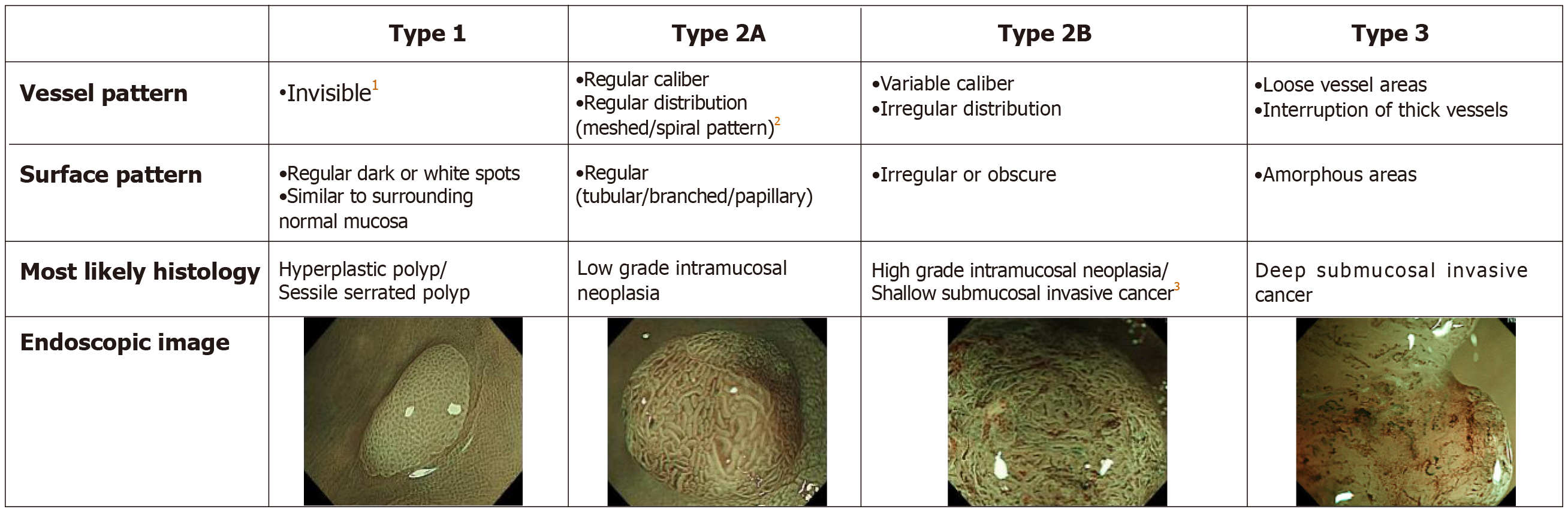
The JNET classification consists of 4 categories; JNET type 1, type 2A, type 2B, and type 3. Each type represnts the histological features of the polyps, and they are categorized by focusing on two specific features, the vessel pattern and the surface pattern (Figure 2). JNET type 1 refers to hyperplastic polyps and sessile serrated polyps. Type 2A refers to LGIN and type 2B corresponds to HGIN or shallow submucosal invasive cancer (S-SMC). Type 3 refers to deep submucosal invasive cancer (D-SMC).
The aim of this review is to reveal the diagnostic performance and the confidence level of the JNET classification. Since there were no previous studies concerning the diagnostic performance and the confidence level of the JNET classification, we analyzed them based on the study data compiled at Sano hospital.
In this review we evaluate the diagnostic performance of the JNET classification and its confidence level (high or low) based on data from the study conducted at Sano Hospital from March 2015 to September 2018, and also those from the systematic review carried out in Medical Literature Analysis and Retrieval System On-Line (MEDLINE) from January 2014 through March 2019.
We investigated the diagnostic performance of the JNET classification including its confidence level (high or low) at Sano Hospital from March 2015 to September 2018. In this study, all colorectal polyps were diagnosed using the JNET classification before endoscopic resection or surgery. NBI magnifying observation was performed by 5 experts and 3 trainees. “High-confidence diagnosis” is defined as a diagnosis that the endoscopist has confidence of more than 90% probability. Both the endoscopic diagnosis and confidence level were recorded in real time during the colonoscopy, and the histopathological diagnosis was reported by an expert pathologist. We evaluated the relation between the JNET type, its confidence level, and the histopathological diagnosis for all polyps as the primary endpoint. The diagnostic performance and the high confidence rate were analyzed based on this data. We evaluated the diagnostic performance in differentiating “neoplasia (type 2A) from non-neoplasia (type 1)”, “Malignant neoplasia (type 2B, 3) vs Benign neoplasia (type 2A)”, and “Deep submucosal invasive cancer (type 3) from other neoplasia (type 2A, 2B)”.
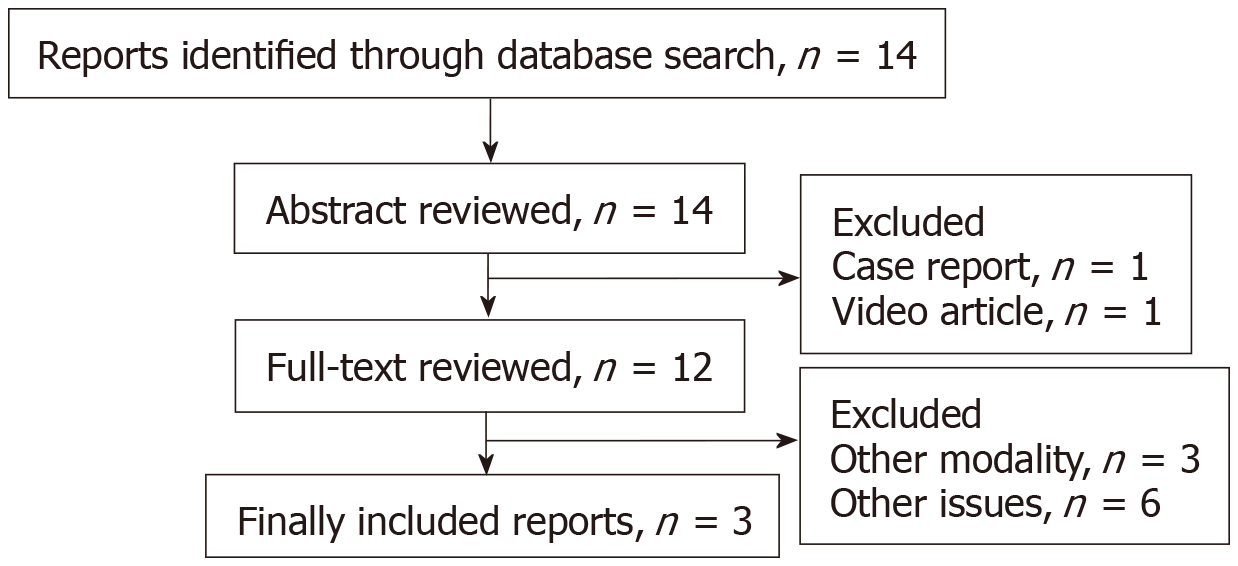
For the purpose of this review, a systematic search was carried out in MEDLINE from January 2014 through March 2019. Keywords included “the Japan NBI Expert Team” or “JNET classification” by two endoscopists. Non-English articles were excluded. Fourteen articles were selected. Non-original articles were also excluded. The full texts of 12 original articles were reviewed. Articles about the diagnostic performance were included. Articles about other modalities and other issues such as study protocol and treatment were excluded. Finally, 3 original articles were selected and included in this study (Figure 3)[9-11].
The authors examined 6138 colorectal polyps which were diagnosed using the JNET classification before endoscopic resection or surgery from March 2015 to September 2018. The histopathological diagnosis of the 6138 polyps were 979 hyperplastic polyps, 244 sessile serrated polyps, 4642 LGIN, 214 HGIN or S-SMC, and 59 D-SMC. Five thousand six hundred twenty-four polyps were diagnosed with high confidence. The high confidence rate was 91.6%. The relation between the JNET classification (with or without confidence level) and the histopathological diagnosis is shown in Table 1. Rate of correspondence between each JNET type and the histopathological diagnosis was 85.4%.
| OA (HC), n | HP, SSP | LGIN | HGIN, S-SMC | D-SMC |
| Type 1 | 653 (564) | 90 (48) | 0 | 0 |
| Type 2A | 570 (440) | 4459 (4289) | 119 (118) | 0 |
| Type 2B | 0 | 93 (42) | 93 (65) | 22 (21) |
| Type 3 | 0 | 0 | 2 (2) | 37 (35) |
Three articles about the diagnostic performance were reviewed in this study. These articles and our study are summarized in Table 2[9-11].
| First author | Cases, n | Participants | Study design | ||
| Sumimoto et al[9] | 2933 | 3 experts | A retrospective analysis | in vivo | Single center |
| Komeda et al[10] | 199 | 3 experts | A retrospective analysis | in vitro | Single center |
| Minoda et al[11] | 40 | 11 experts and 11 non-GI trainees | A retrospective analysis | in vitro | Single center |
| Our study | 6138 | 5 experts and 3 trainees | A retrospective analysis | in vivo | Single center |
Sumimoto et al[9] conducted a retrospective analysis of 2933 colorectal lesions (136 hyperplastic polyps/sessile serrated polyps, 1926 LGIN, 571 HGIN, 87 S-SMC, and 213 D-SMC). The accuracy of type 1, 2A, 2B, and 3 were 99.3%, 77.1%, 78.1%, and 96.6% respectively.
Komeda et al[10] performed a retrospective image evaluation study in 199 colorectal lesions (14 hyperplastic polyps/sessile serrated polyps, 127 LGIN, 22 HGIN, 19 S-SMC, and 17 D-SMC). The accuracy of type 1, 2A, 2B, and 3 were 98.5%, 90.9%, 87.4%, and 94.0%, respectively. They also analyzed of the relation between the macroscopic type and the diagnostic performance. They concluded that the JNET classification was useful for the diagnosis of hyperplastic polyps, sessile serrated polyps, LGIN, HGIIN and D-SMC, but not S-SMC.
Minoda et al[11] conducted a retrospective image evaluation study of 40 colorectal lesions involving 22 doctors (11experts and 11 non-gastrointestinal trainees). The average diagnostic accuracy was 76.6% for the experts and 61.4% for the trainees, though the relation between the JNET classification and the histopathological diagnosis was not disclosed. They concluded that the JNET classification was useful for differentiating malignant polyps from benign ones for every doctor. They also revealed orientation and training were necessary to use this system adequately even for experienced colonoscopists.
The diagnostic performance is important in determining the treatment strategy. In particular, the three differentiations: neoplasia (type 2A) vs non neoplasia (type 1), malignant neoplasia (type 2B, 3) vs benign neoplasia (type 2A), and deep submucosal invasive cancer (type 3) from other neoplasia (type 2A, 2B). The details of each diagnostic performance are shown in Table 3-5. We analyzed the diagnostic performance for each differentiation in our study and the previous reports. Minoda’s report was excluded in these analyses, since necessary details and relations were not disclosed.
| First author | Sumimoto | Komeda | Our study |
| Accuracy, % | 99.0 | 98.0 | 88.8 |
| Sensitivity, % | 99.8 | 99.3 | 98.1 |
| Specificity, % | 87.5 | 85.7 | 53.3 |
| PPV, % | 99.1 | 98.5 | 88.9 |
| NPV, % | 97.5 | 92.3 | 87.9 |
| First author | Sumimoto | Komeda | Our study |
| Accuracy, % | 80.7 | 91.9 | 96.1 |
| Sensitivity, % | 71.9 | 81.0 | 56.4 |
| Specificity, % | 84.7 | 96.9 | 98.2 |
| PPV, % | 67.8 | 92.2 | 62.3 |
| NPV, % | 87.0 | 91.9 | 97.7 |
| First author | Sumimoto | Komeda | Our study |
| Accuracy, % | 96.4 | 93.5 | 99.6 |
| Sensitivity, % | 55.4 | 29.4 | 62.7 |
| Specificity, % | 99.8 | 100.0 | 100.0 |
| PPV, % | 95.2 | 100.0 | 94.9 |
| NPV, % | 96.4 | 93.4 | 99.6 |
The diagnostic performance in differentiating neoplasia (type 2A) from non-neoplasia (type 1) is directly associated with the necessity of endoscopic treatment. Type 2A polyps should be resected by polypectomy. However, it is usually not necessary to resect type1 polyps. The sensitivity, the accuracy and the negative predictive value (NPV) were 98.1%-99.8%, 88.8%-99.0%, and 88.9%-99.1%, respectively. According to this classification, endoscopists can identify almost all neoplasia.
In high confidence cases, counting 93.1% among all polpys, they were high enough to enable “Detect InSpect ChAractrise Resect and Discard strategy”, according to “Preservation and incorporation of valuable endoscopic innovations initiative” from American Society For Gastrointestinal Endoscopy[12,13].
The diagnostic performance in differentiating malignant neoplasia from benign neoplasia is associated with the necessity of en bloc resection. While type 2A polyps can be treated by piecemeal EMR or polypectomy, type 2B polyps should be resected en bloc to obtain a precise histologic diagnosis from the specimen. The accuracy, specificity, and NPV of this diagnosis are 80.7%-96.1%, 84.7%-98.2%, and 87.0%-97.7%, respectively. This is considered beneficial in diagnosing polyps as malignant neoplasm. By using the JNET classification, endoscopist can appropriately determine whether to perform en bloc resection or not.
The diagnostic performance in differentiating deep submucosal invasive cancer from other neoplasia is associated with the necessity of surgical resection. As for this distinction, the specificity was extremely high being 99.8%-100.0%. The JNET classification enables endoscopists to avoid unnecessary surgery for non-invasive neoplasia. In our study, the unnecessary surgeries were only two cases. On the other hand, 10.6%-23.9% of type 2B lesions were D-SMCs, and 0.0%-5.1% of type 3 lesions were S-SMCs. Additional magnifying chromoendoscopy is recommended in cases where it is difficult to differentiate between shallow and deep submucosal invasive cancers.
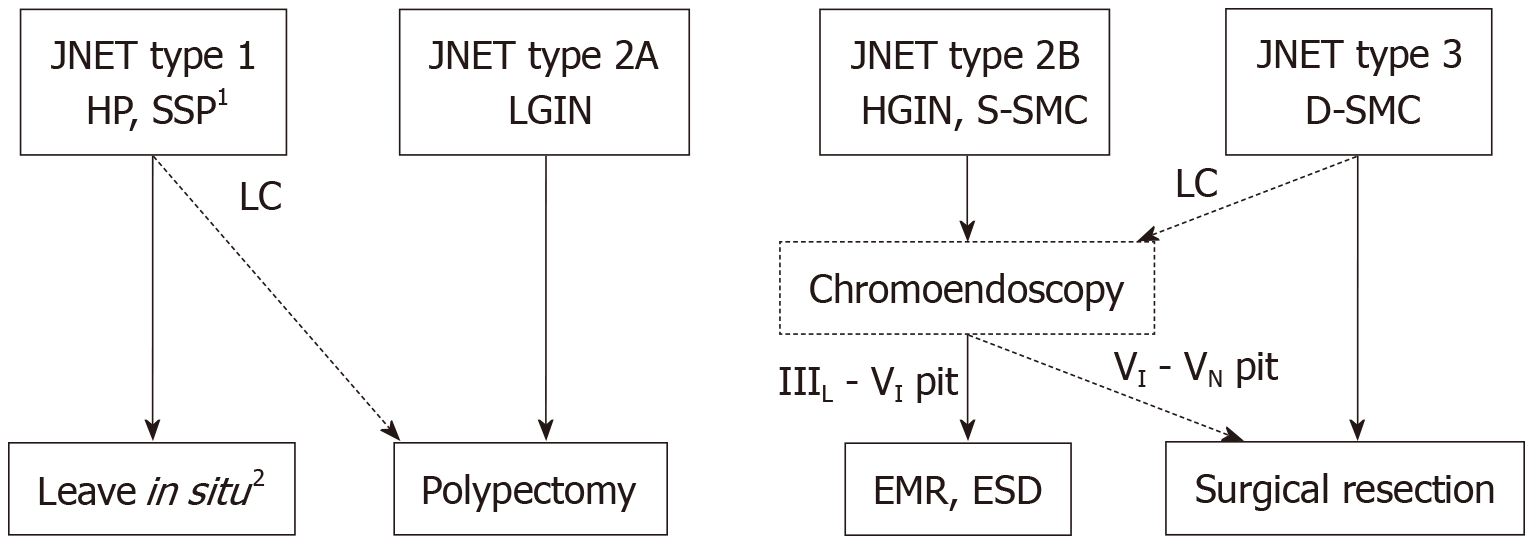
This is the first review concerning the diagnostic performance of the JNET classification taking account of the confidence level. Based on this review, we propose treatment strategy for colorectal localized lesions using the JNET classification with its confidence level (Figure 4).
Type 1 polyps generally do not need resection except for sessile serrated polyps[14]. Type 2A polyps shall be resected by polypectomy or EMR. Utsumi et al[15] reported that additional chromoendoscopy in type 1 and 2A polyps with low confidence prediction did not improve accuracy enough. Therefore, additional chromoendoscopy is considered to be unnecessary in order to differentiate type from type 1.
Whereas type 2A polyps can be resected by piecemeal EMR, type 2B polyps should be resected en bloc by EMR or ESD to obtain a precise histologic diagnosis concerning the invasion depth and determining endoscopic curability. Our review revealed the usefulness of the JNET classification, in that it accurately differentiated malignant polyps (type 2B, 3) from benign (type 2A). It should be noted that 37.3%-70.6% of deep submucosal invasive cancers showed type 2B findings, magnifying chromoendoscopy is recommended before high-risk endoscopic resection for deep submucosal invasive cancer in type 2B polyps, if it is available. Type 3 lesions were diagnosed to be D-SMC with more than 99% specificity in our review, and therefore they are indicated for surgical resection.
The JNET classification is considered to have as high diagnostic performance as the NICE classification. However, there have been no studies directly comparing the JNET classification with the NICE classification. For comparison with the NICE classification, we evaluated the diagnostic performance with high confidence prediction and the high confidence rate in regards to two differentiations; “Neoplasia vs non neoplasia” and “Deep submucosal invasive cancer vs other neoplasia” (Table 6). In both differentiations, the high confidence rate in the JNET classification was significantly higher than that of the NICE classification. It may demonstrate the JNET classification is clearer and easier to use than the NICE classification for the endoscopists. Magnifying observation may increase the high confidence rate of endoscopic diagnosis.
The JNET classification is compatible with the NICE classification in that both classifications are divided into three major categories (type 1, 2, and 3) corresponding to the similar histopathology. The NICE type 2 corresponds approximately to the JNET type 2A and type 2B. Thanks to this similarity, endoscopists using the NICE classification should be able to use the JNET classification easily. A video article explaining typical examples and key points will help to adopt the JNET classification[16].
The limitation in this review is that there were only 3 articles about the diagnostic performance of the JNET classification. The previous studies were all retrospective single center studies. A large-scale prospective multicenter validation study of the JNET classification is awaited in the future. About the comparison the JNET classification with the NICE classification, though it is better to compare in the same endoscopic and histopathologic center, we did not such a comparative trial yet.
We predict that the JNET classification will provide endoscopists with a useful treatment strategy based on precise histopathological predictions and a higher confidence level for optical diagnosis.
The JNET classification enables endoscopists to identify almost all neoplasia, to appropriately determine whether to perform en bloc resection or not, and to avoid unnecessary surgery.
Manuscript source: Invited Manuscript
Specialty type: Medicine, research and experimental
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Eyraud D S-Editor: Tang JZ L-Editor: Filipodia E-Editor: Qi LL
| 1. | Sano Y, Horimatsu T, Fu KI, Katagiri A, Muto M, Ishikawa H. Magnifying observation of microvascular architecture of colorectal lesions using a narrow band imaging system. Dig Endosc. 2006;18 Suppl 1:S44-S51. [RCA] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 80] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 2. | Wada Y, Kudo SE, Kashida H, Ikehara N, Inoue H, Yamamura F, Ohtsuka K, Hamatani S. Diagnosis of colorectal lesions with the magnifying narrow-band imaging system. Gastrointest Endosc. 2009;70:522-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 148] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 3. | Nikami T, Saito S, Tajiri H, Ikegami M. The evaluation of histological atypia and depth of invasion of colorectal lesions using magnified endoscopy with narrow-band imaging. Gastroenterol Endosc. 2009;51:10-19. [DOI] [Full Text] |
| 4. | Hirata M, Tanaka S, Oka S, Kaneko I, Yoshida S, Yoshihara M, Chayama K. Magnifying endoscopy with narrow band imaging for diagnosis of colorectal tumors. Gastrointest Endosc. 2007;65:988-995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 155] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 5. | Hewett DG, Kaltenbach T, Sano Y, Tanaka S, Saunders BP, Ponchon T, Soetikno R, Rex DK. Validation of a simple classification system for endoscopic diagnosis of small colorectal polyps using narrow-band imaging. Gastroenterology. 2012;143:599-607.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 376] [Cited by in RCA: 417] [Article Influence: 32.1] [Reference Citation Analysis (0)] |
| 6. | Hayashi N, Tanaka S, Hewett DG, Kaltenbach TR, Sano Y, Ponchon T, Saunders BP, Rex DK, Soetikno RM. Endoscopic prediction of deep submucosal invasive carcinoma: validation of the narrow-band imaging international colorectal endoscopic (NICE) classification. Gastrointest Endosc. 2013;78:625-632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 282] [Cited by in RCA: 321] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 7. | Sano Y, Tanaka S, Kudo SE, Saito S, Matsuda T, Wada Y, Fujii T, Ikematsu H, Uraoka T, Kobayashi N, Nakamura H, Hotta K, Horimatsu T, Sakamoto N, Fu KI, Tsuruta O, Kawano H, Kashida H, Takeuchi Y, Machida H, Kusaka T, Yoshida N, Hirata I, Terai T, Yamano HO, Kaneko K, Nakajima T, Sakamoto T, Yamaguchi Y, Tamai N, Nakano N, Hayashi N, Oka S, Iwatate M, Ishikawa H, Murakami Y, Yoshida S, Saito Y. Narrow-band imaging (NBI) magnifying endoscopic classification of colorectal tumors proposed by the Japan NBI Expert Team. Dig Endosc. 2016;28:526-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 455] [Cited by in RCA: 403] [Article Influence: 44.8] [Reference Citation Analysis (1)] |
| 8. | Iwatate M, Sano Y, Tanaka S, Kudo SE, Saito S, Matsuda T, Wada Y, Fujii T, Ikematsu H, Uraoka T, Kobayashi N, Nakamura H, Hotta K, Horimatsu T, Sakamoto N, Fu KI, Tsuruta O, Kawano H, Kashida H, Takeuchi Y, Machida H, Kusaka T, Yoshida N, Hirata I, Terai T, Yamano HO, Nakajima T, Sakamoto T, Yamaguchi Y, Tamai N, Nakano N, Hayashi N, Oka S, Ishikawa H, Murakami Y, Yoshida S, Saito Y; Japan NBI Expert Team (JNET). Validation study for development of the Japan NBI Expert Team classification of colorectal lesions. Dig Endosc. 2018;30:642-651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 96] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 9. | Sumimoto K, Tanaka S, Shigita K, Hirano D, Tamaru Y, Ninomiya Y, Asayama N, Hayashi N, Oka S, Arihiro K, Yoshihara M, Chayama K. Clinical impact and characteristics of the narrow-band imaging magnifying endoscopic classification of colorectal tumors proposed by the Japan NBI Expert Team. Gastrointest Endosc. 2017;85:816-821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 110] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 10. | Komeda Y, Kashida H, Sakurai T, Asakuma Y, Tribonias G, Nagai T, Kono M, Minaga K, Takenaka M, Arizumi T, Hagiwara S, Matsui S, Watanabe T, Nishida N, Chikugo T, Chiba Y, Kudo M. Magnifying Narrow Band Imaging (NBI) for the Diagnosis of Localized Colorectal Lesions Using the Japan NBI Expert Team (JNET) Classification. Oncology. 2017;93 Suppl 1:49-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 63] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 11. | Minoda Y, Ogino H, Chinen T, Ihara E, Haraguchi K, Akiho H, Takizawa N, Aso A, Tomita Y, Esaki M, Komori K, Otsuka Y, Iwasa T, Ogawa Y. Objective validity of the Japan Narrow-Band Imaging Expert Team classification system for the differential diagnosis of colorectal polyps. Dig Endosc. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 12. | Ignjatovic A, East JE, Suzuki N, Vance M, Guenther T, Saunders BP. Optical diagnosis of small colorectal polyps at routine colonoscopy (Detect InSpect ChAracterise Resect and Discard; DISCARD trial): a prospective cohort study. Lancet Oncol. 2009;10:1171-1178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 287] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 13. | Rex DK, Kahi C, O'Brien M, Levin TR, Pohl H, Rastogi A, Burgart L, Imperiale T, Ladabaum U, Cohen J, Lieberman DA. The American Society for Gastrointestinal Endoscopy PIVI (Preservation and Incorporation of Valuable Endoscopic Innovations) on real-time endoscopic assessment of the histology of diminutive colorectal polyps. Gastrointest Endosc. 2011;73:419-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 406] [Cited by in RCA: 463] [Article Influence: 33.1] [Reference Citation Analysis (0)] |
| 14. | Sano W, Sano Y, Iwatate M, Hasuike N, Hattori S, Kosaka H, Ikumoto T, Kotaka M, Fujimori T. Prospective evaluation of the proportion of sessile serrated adenoma/polyps in endoscopically diagnosed colorectal polyps with hyperplastic features. Endosc Int Open. 2015;3:E354-E358. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | Utsumi T, Iwatate M, Sunakawa H, Teramoto A, Hirata D, Hattori S, Sano W, Hasuike N, Ichikawa K, Fujimori T, Sano Y. Additional chromoendoscopy for colorectal lesions initially diagnosed with low confidence by magnifying narrow-band imaging: Can it improve diagnostic accuracy? Dig Endosc. 2018;30 Suppl 1:45-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Sano Y, Hirata D, Saito Y. Japan NBI Expert Team classification: Narrow-band imaging magnifying endoscopic classification of colorectal tumors. Dig Endosc. 2018;30:543-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |