Published online Sep 6, 2019. doi: 10.12998/wjcc.v7.i17.2652
Peer-review started: April 23, 2019
First decision: June 12, 2019
Revised: June 16, 2019
Accepted: June 26, 2019
Article in press: June 26, 2019
Published online: September 6, 2019
Processing time: 137 Days and 9.6 Hours
Hypopharyngeal lipoma is a rare disease that can lead to asphyxiation after aspiration. Sclerotic lipoma in the hypopharynx is an extremely rare histological type. Hypopharyngeal lipoma should be resected in time after diagnosis.
An 86-year-old female patient presented to our department with a long pedunculated mass protruding from her mouth. Until this time, the patient had no dyspnea, dysphagia, or throat discomfort. Physical examination showed stable vital signs and clear consciousness. The pedicel was derived from the posterior wall of the hypopharynx. The tumor was smooth, hyperemic and dark red, about 10 cm long, and 4 cm wide. In order to prevent airway obstruction, the hypopharyngeal tumor was excised in emergent operation. The pharyngeal cavity was exposed by a mouth gag during the operation. A disposable plasma knife was used to completely remove the tumor along the base of the new organism, and no active bleeding occurred. The postoperative pathological results were sclerotic lipoma.
Lipoma in the pharynx is relatively rare. Patients with this condition must be referred immediately to Ear-Nose-Throat specialists and complete surgical excision should be performed as soon as possible to prevent serious complications, such as airway obstruction and death.
Core tip: Sclerotic lipoma in the hypopharynx is extremely rare. We report a case of hypopharyngeal sclerotic lipoma in a female patient. The lipoma was removed with plasma radiofrequency at low temperature under general anesthesia. The patient had no discomfort in the hypopharynx after surgery. The pathologic findings, clinical feature, and treatment of the disease are presented and discussed.
- Citation: Sun Q, Zhang CL, Liu ZH. An extremely rare pedunculated lipoma of the hypopharynx: A case report. World J Clin Cases 2019; 7(17): 2652-2657
- URL: https://www.wjgnet.com/2307-8960/full/v7/i17/2652.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i17.2652
Up to date, less than 100 cases of pedunculated lipoma of hypopharynx have been reported[1]. Most of them are fibrous lipoma, as shown in histopathology. We here report a rare case of sclerotic lipoma. The first case of pedunculated lipoma of hypopharynx was reported by Colchester in 1952 in a patient who died of asphyxi-ation due to sucking in the lipoma[2]. Hypopharyngeal pedunculated lipoma grows slowly and generally has no obvious symptoms. When respiratory aspiration occurs, it can block the upper airway and kill the patient easily. The key to treatment is timely surgical resection.
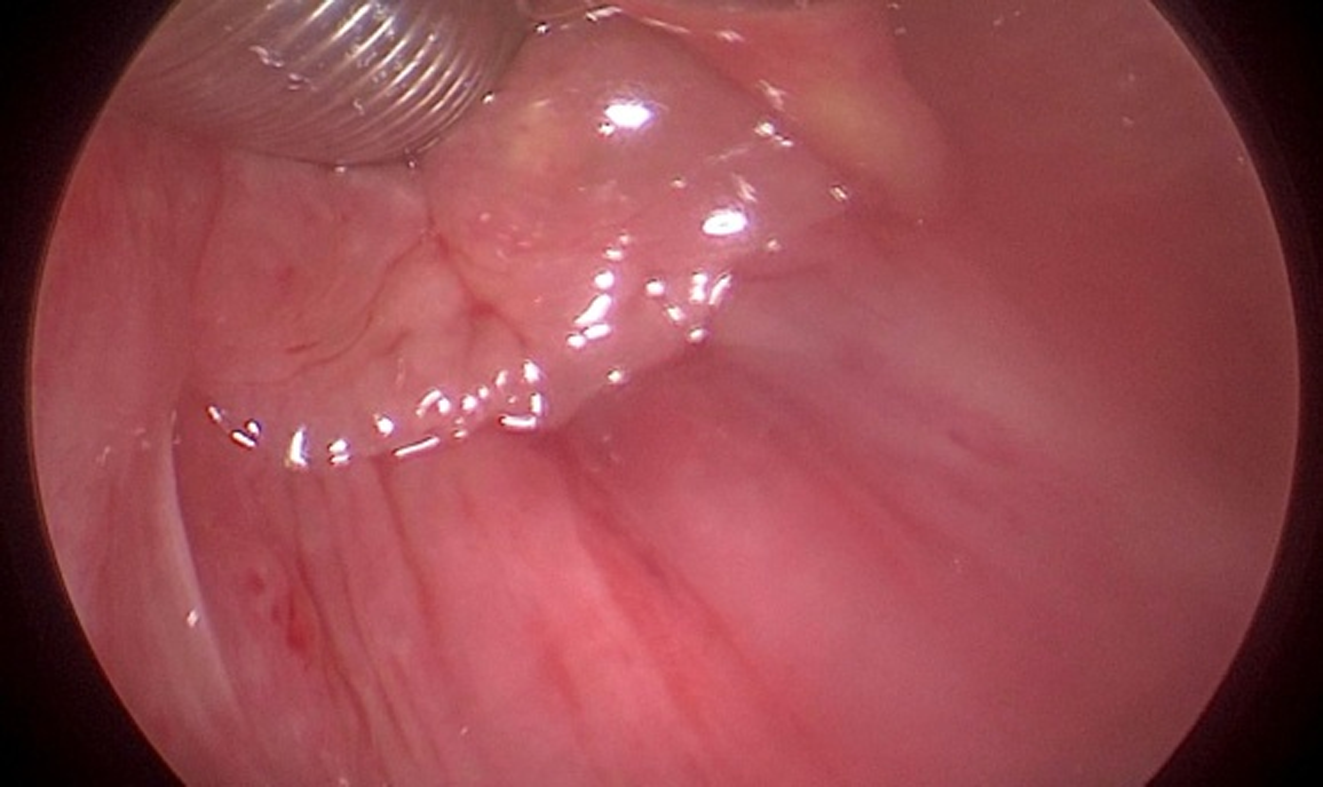
An 86-year-old female patient presented to our department with a long pendulous mass protruding from her mouth (Figure 1).
The patient coughed up the mass in the morning and had no dyspnea or dysphagia until entering the hospital.
She had no history of surgery, chronic diseases, or allergies.
She gave birth to two daughters, both via vaginal delivery, and she had no history of smoking or drinking. There was no similar history in the family.
A thick pendulous mobile mass was hanging outside the mouth, and the root was derived from the back wall of the hypopharynx. The surface of the mass was smooth and hyperemic. Other tests were normal.
No abnormality was found in routine blood tests, biochemical tests, or electro-cardiogram.
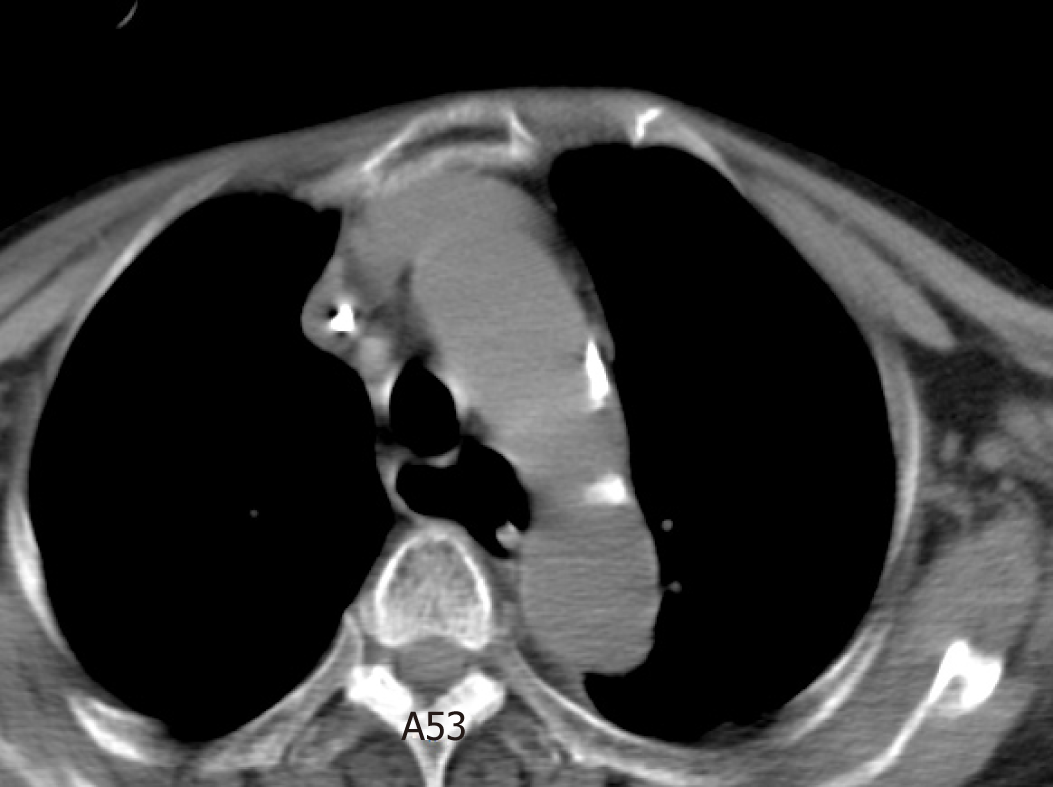
Postoperative chest computed tomography showed widened esophagus.
Sclerotic lipoma in the hypopharynx.
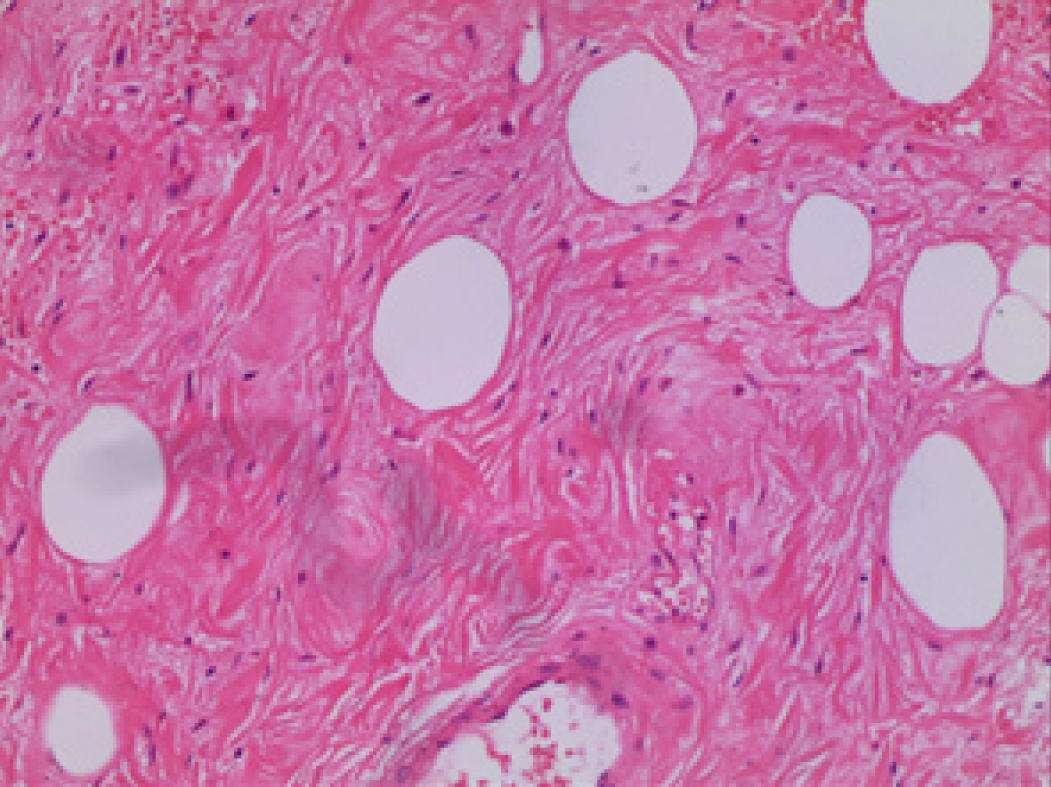
The lipoma was removed with plasma radiofrequency at low temperature under general anesthesia (Figures 2 and 3). The postoperative pathological results were fibrosclerosing lipoma, and immunohistochemistry was positive for vimentin, S100, and CD34 (Figure 4).
Electronic laryngoscopy showed good white membrane growth in the operative area 4 d after surgery. The patient had no discomfort in the hypopharynx.
Lipoma in the pharynx is relatively rare[3], and accounts for 0.6% of the benign tumors of the pharynx[4]. Lipoma is associated with endocrine factors, infection, chronic disease, infection, and heredity[5]. Lipoma of the hypopharynx grows slowly and generally has no obvious symptoms. Only a few patients may present with dys-phagia, reflux foreign body sensation, or cough[6], but sudden airway blockage may occur[7]. Most of the patients do not visit the emergency department for treatment until a rapidly increased abdominal pressure appeared, such as cough, and the tumor came out of the mouth. Our patient, who had no special sensation for a long time, was admitted to the emergency department of our hospital after coughing out the mass. To our surprise, the large tumor did not cause swallowing and breathing difficulties. The reason may be that the narrow peduncle of the lipoma can pass through the pharyngoesophageal sphincter, and the tumor body grows slowly in the esophagus, resulting in expansion of the esophagus. The slow process makes the body adaptable to the tumor in this patient. Enlarged esophagus was seen on postoperative chest computed tomography (Figure 5).
The most serious complication of hypopharyngeal lipoma is asphyxia death. Once the tumor is diagnosed, the patient is likely to suffer from airway obstruction within a short period of time, which should be monitored closely. The first reported patient with hypopharyngeal lipoma died of asphyxia due to aspiration[4]. Therefore, timely surgical treatment is necessary. Currently, there are a variety of surgical approaches. Some authors recommend endoscopic resection for small lesions, while for tumors larger than 2 cm, open surgery is preferred[7]. Others suggest that endoscopic surgery has advantages of quick recovery and less trauma to patients, and endoscopic resection may also be used for larger masses[5,8]. In contrast to previous reports of similar cases, we used the plasma knife as the resection tool. The plasma knife has a good hemostasis function during the operation, keeping the field clear, and low temperature can minimize the damage to the surrounding tissues. Therefore, we recommend the plasma knife as a tool for tumor resection in similar cases. Specific tumor resection should refer to the size, location, and scope of the tumor as well as the experience of the surgeon. Considering that our patient was old and complicated with systemic diseases such as heart disease, we selected the plasma resection combined with endoscopic resection for tumor exposure by mouth gag. After the surgery, the patient was transferred to the ordinary ward and able to take a fluid diet. The patient and her family were satisfied with the treatment effect.
In this case, the pathologic type is sclerotic lipoma, which is a variant type in the pathological classification of lipoma and was first reported by Zelger et al[9] in 1997. It is characterized by spindle cells or fibroblast-like cells and dense intercellular matrix microscopically, in which fat cells are distributed[10]. The structure is similar to fibroma, except that there are different numbers of fat cells in the background of fibrosclerosis. To date, less than 30 cases of sclerotic lipoma have been reported worldwide[11], most of which occur in the limbs and scalp, and no literature has reported one on pharynx.
We report a rare case of hypopharyngeal pedunculated lipoma, and the pathological type is sclerotic lipoma. We recommend timely resection to prevent airway ob-struction and death. Plasma resection is a good option during surgery.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bellan C S-Editor: Cui LJ L-Editor: Filipodia E-Editor: Xing YX
| 1. | Mendez Saenz MA, Villagomez Ortiz VJ, Villegas González MJ, Gonzalez Andrade B, Liñan Arce MA, Soto-Galindo GA, Treviño González JL. Dyspnea and dysphagia associated to hypopharyngeal fibrolipoma: A case report. Ann Med Surg (Lond). 2017;16:30-33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Penfold JB. Lipoma of the hypopharynx. Br Med J. 1952;1:1286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Evcimik MF, Ozkurt FE, Sapci T, Bozkurt Z. Spindle cell lipoma of the hypopharynx. Int J Med Sci. 2011;8:479-481. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Cantarella G, Neglia CB, Civelli E, Roncoroni L, Radice F. Spindle cell lipoma of the hypopharynx. Dysphagia. 2001;16:224-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Acquaviva G, Varakliotis T, Badia S, Casorati F, Eibenstein A, Bellocchi G. Lipoma of Piriform Sinus: A Case Report and Review of the Literature. Case Rep Otolaryngol. 2016;2016:2521583. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Zakrzewski A. Subglottic lipoma of the larynx. (Case report and literature review). J Laryngol Otol. 1965;79:1039-1048. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Sakamoto K, Mori K, Umeno H, Nakashima T. Surgical approach to a giant fibrolipoma of the supraglottic larynx. J Laryngol Otol. 2000;114:58-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Shi HY, Wei LX, Wang HT, Sun L. Clinicopathological features of atypical lipomatous tumors of the laryngopharynx. J Zhejiang Univ Sci B. 2010;11:918-922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Zelger BG, Zelger B, Steiner H, Rütten A. Sclerotic lipoma: lipomas simulating sclerotic fibroma. Histopathology. 1997;31:174-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Wang J, Zhu X. Soft tissue tumor pathology. Beijing: People's Health Publishing House 2017; 484-495. |
| 11. | Laskin WB, Fetsch JF, Michal M, Miettinen M. Sclerotic (fibroma-like) lipoma: a distinctive lipoma variant with a predilection for the distal extremities. Am J Dermatopathol. 2006;28:308-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |