Published online Sep 6, 2019. doi: 10.12998/wjcc.v7.i17.2567
Peer-review started: April 12, 2019
First decision: May 31, 2019
Revised: June 30, 2019
Accepted: July 20, 2019
Article in press: July 20, 2019
Published online: September 6, 2019
Processing time: 150 Days and 22.8 Hours
Fascia iliaca compartment block is a technique that blocks three nerves, similar to a 3-in-1 nerve block. This block provides analgesia for patients undergoing lower limb surgery, and is a simple technique that is easy to implement. Here, we report a case of fascia iliaca compartment block in a patient with myocardial infarction who underwent emergency middle thigh amputation.
A 78-year-old female patient weighing 38 kg with gangrene and occlusive peripheral atherosclerosis of the right leg underwent an emergency middle thigh amputation. The patient had a history of hypertension, coronary heart disease, cerebral infarction, anterior wall myocardial infarction, and had recently undergone percutaneous coronary intervention consisting of coronary angiography and right coronary artery stent implantation. Considering the patient's condition, an ultrasound-guided fascia iliaca compartment block combined with general anesthesia was implemented for amputation. The fascia iliaca compartment block provided analgesia for the operation, and reduced the dosage of general anesthetics. It also alleviated adverse cardiovascular effects caused by pain stress, and ensured the safety of the patient during the perioperative period. This block also provided postoperative analgesia. The patient had a good prognosis, and was subsequently discharged from hospital.
Fascia iliaca compartment block provides surgical analgesia. It also alleviates adverse cardiovascular effects, and ensures patient safety during the perioperative period.
Core tip: Ultrasound-guided fascia iliaca compartment block combined with general anesthesia can provide better intraoperative analgesia for thigh surgery, reduce the dosage of general anesthetics, and alleviate the adverse cardiovascular effects caused by pain stress. In this case report, we describe the effects of fascia iliaca compartment block in a patient with myocardial infarction who underwent an emergency middle thigh amputation. Use of this block ensured the safety of the patient during the perioperative period.
- Citation: Ling C, Liu XQ, Li YQ, Wen XJ, Hu XD, Yang K. Ultrasound-guided fascia iliaca compartment block combined with general anesthesia for amputation in an acute myocardial infarction patient after percutaneous coronary intervention: A case report. World J Clin Cases 2019; 7(17): 2567-2572
- URL: https://www.wjgnet.com/2307-8960/full/v7/i17/2567.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i17.2567
Thigh surgery presents a challenging clinical problem commonly encountered by medical staff. Traditional analgesia for thigh surgery involves opioids and regional nerve blockade, which have been demonstrated to be effective. Emergency surgery is often encountered in the elderly, and presents special demands for the anesthesi-ologist. Fascia iliaca compartment block is a technique that blocks three nerves similar to a 3-in-1 nerve block. The fascia iliaca space has the iliopsoas muscle behind, the fascia iliaca in front, and the fascia lata covering the superficial fascia of the fascia iliaca. The femoral nerve, the lateral femoral cutaneous nerve, and the obturator nerve are located below the fascia iliaca at the pelvic segment. The fascia iliaca compartment block is used to block these three nerves to meet the needs of lower limb analgesia and anesthesia. From references[1,2], we know that fascia iliaca compartment block can provide superior analgesia and decreased opioid consumption with minimal side effects. It can be deployed in a relatively quick fashion after a small amount of training, and can be executed with high success rates under ultrasound guidance. Compared with general anesthesia, fascia iliaca compartment block combined with general anesthesia reduces the dosage of general anesthetics required, stabilizes the hemodynamics, and improves postoperative analgesia. Here, we report a case of fascia iliaca compartment block in a patient with myocardial infarction who underwent emergency middle thigh amputation.
Shortness of breath and dyspnea for 10 d.
A 78-year-old female patient weighing 38 kg was diagnosed with acute non-ST segment elevation myocardial infarction 10 d previously in another hospital, which manifested as chest pain, shortness of breath and dyspnea, and was treated with tracheal intubation, ventilator-assisted ventilation and vasodilation. Serum troponin concentration was 0.7 ng/mL. The patient was transferred to the intensive care unit (ICU) at our hospital.
Hypertension and coronary heart disease for 15 years, cerebral infarction for 8 years, and anterior wall myocardial infarction for 5 years.
The patient had decreased blood pressure, increased heart rate and fever, characterized by septic shock, cardiogenic shock, and blood oxygen saturation (SpO2) fluctuations above 97% when tracheal intubation was connected to the ventilator. The lungs demonstrated thick breath sounds, and the lower lungs showed slight moist rale. Her heart rate was 100 bpm, the heart sound was low and blunt, and there was no noise in each valve area. Dry necrosis of the right lower foot and visible scattered ecchymoses were observed.
The serum creatine kinase-MB concentration was 25.8 ng/mL, and the white blood cell count was 24.25 × 109/L.
The bedside digital radiography chest X-ray showed double lung infection. Color Doppler ultrasound showed moderate mitral regurgitation and mild aortic regurgi-tation.
Non-ST segment elevation acute myocardial infarction, right leg gangrene, and right leg peripheral arterial occlusive disease.
In the ICU, the patient had been given imipenem and cilastatin sodium for anti-infection, as well as dopamine and norepinephrine as anti-shock treatment. Three days previous, the patient had undergone percutaneous coronary intervention (PCI) consisting of coronary angiography and right coronary artery stent implantation by a cardiologist. The coronary angiography showed that there was no obvious stenosis in the left main coronary artery, 70%-80% stenosis in the middle part of the anterior descending artery, 80% stenosis in the opening of the circumflex artery, and 90% stenosis in the proximal part of the right coronary artery. The patient was diagnosed with right coronary artery dominant type and three-vessel coronary lesions. Considering the patient's condition, a stent was implanted in the right coronary artery, and the effect of vascular opening was good. Following PCI, the patient's body temperature further increased (38.5-39 ºC), and the white blood cell count was 33.74 × 109/L. The right lower extremity showed dry skin necrosis and scattered ecchymoses. The right middle iliac artery showed occlusion. The patient had an endotracheal tube in place and presented with fever, and the SpO2 was over 97% with medium flow oxygen inhalation. Following multi-disciplinary team consultation, the patient was scheduled for mid-thigh amputation.
The patient was conscious and entered the operating room with a tracheal catheter in place. Dopamine was pumped continuously at 5 µg/kg per min, and norepi-nephrine was pumped at 0.06 µg/kg per min into the right internal jugular vein. The patient’s non-invasive blood pressure was 95/45 mmHg, heart rate was 98 bpm, and SpO2 was 99%. A left radial artery puncture catheter was used to monitor arterial blood pressure. The anesthesia system was connected to the tracheal catheter to assist ventilation.
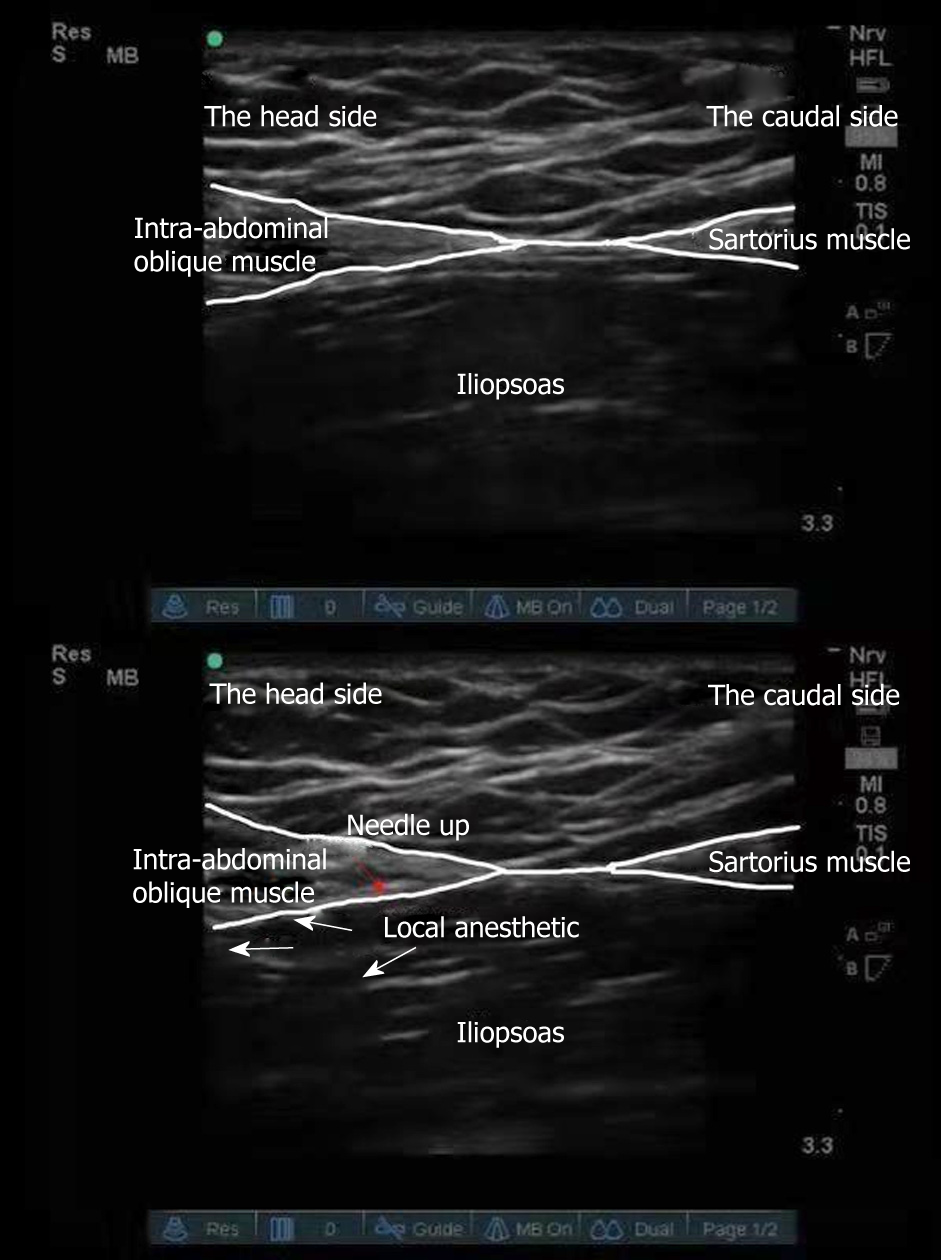
Ultrasound-guided right-side improved fascia iliaca compartment block was used for surgical analgesia. The procedures were as follows: The ultrasound probe was vertically placed on the outer third of the inguinal ligament to identify the hourglass sign in the obliquus internus abdominis, sartorius muscle and iliopsoas muscle[3] (Figure 1). The in-plane technique was used to implant the needle from the tail end to the head of the patient to reach the deep surface of the fascia iliaca. Local anesthetics (0.33% ropivacaine hydrochloride 30 mL) was injected into the space between the obliquus internus abdominis and iliopsoas muscle. The anesthetic plane was tested by acupuncture after 5 min and 10 min to ensure the block effect. After blocking, midazolam 2 mg, sufentanil 10 µg, cisatracurium 6 mg and etomidate 6 mg were intravenously injected to induce anesthesia, and 1% sevoflurane inhalation anesthesia-maintained anesthesia.
The operation duration was 65 min. The bispectral index was maintained between 45 and 60. Vasoactive drugs were used to regulate blood pressure and heart rate. Vital signs were stable during the perioperative period. The Critical Care Pain Observation Tool (CPOT) score can be used to assess pain in critically ill patients with no hypnotic, opioid-based analgo-sedation[4,5], the CPOT score was 2 at 6 h after surgery, and the Ramsay sedation score was 3. The effect of postoperative analgesia was satisfactory. Two days after the operation, inflammatory indicators improved, and tracheal intubation was removed.
No serious adverse cardiovascular events occurred during the perioperative period, and the patient was subsequently discharged.
The incremental risk of noncardiac surgery on adverse cardiac events among post-stent patients is highest in the initial 6 mo following stent implantation, and stabilizes at 1.0% after 6 mo[6,7]. From references[8], in the case of emergency surgery, it is particularly important for anesthesiologists to prevent, monitor and treat myocardial ischemia during surgery.
Our patient suffered from an acute myocardial infarction approximately 2 wk previous, and had undergone PCI. Due to vascular occlusion and necrosis of the right lower extremity, the patient presented with septic shock, and underwent both tracheal intubation and artificial ventilation. She also had multiple organ dysfunction. It was necessary to perform an urgent right lower extremity amputation to eliminate the source of infection. For amputation patients, intraspinal anesthesia is the preferred method of anesthesia. However, this patient was administered anticoagulation therapy after PCI, and coagulation function was abnormal; thus, intraspinal anesthesia was unsuitable.
As this patient had suffered from a recent acute myocardial infarction and her cardiac function was poor, it was crucial to maintain stable circulation, as well as a balance between oxygen supply and demand during surgery. If only general anesthesia was selected, deep anesthesia would be required. Anesthetic agents can depress myocardial contraction[9]. A large dosage of general anesthetics would aggravate myocardial depression and induce adverse cardiac events. Krych et al[10] reported that the quality of perioperative analgesia provided by the fascia iliaca blockade was excellent, and resulted in both low opioid consumption and a high quality of pain relief. Ultrasound-guided fascia iliaca compartment block provided the perfect analgesia, and decreased the consumption of general anesthetics, which avoided cardiac and circulatory function depression. This was caused by deep general anesthesia and the stress reaction caused by light anesthesia. Considering the patient's condition, ultrasound-guided fascia iliaca compartment block combined with general anesthesia was employed for amputation.
The fascia iliaca space has the iliopsoas muscle behind, the fascia iliaca in front, and the fascia lata covering the superficial fascia of the fascia iliaca[11-13]. The femoral nerve, the lateral femoral cutaneous nerve, and the obturator nerve are located below the fascia iliaca at the pelvic segment[14]. Fascia iliaca compartment block is used to block these nerves to meet the needs of lower limb analgesia and anesthesia. It is used for anesthesia and analgesia of the hip, knee and thigh[15,16]. Ultrasound-guided fascia iliaca compartment block can be divided into parallel puncture of the inguinal ligament, and improved vertical puncture of the inguinal ligament. In a parallel puncture of the inguinal ligament, drugs spread to the lower part of the inguinal ligament, while the modified fascia iliaca compartment block technique under real-time ultrasound guidance and local anesthetics spread to the head[17,18]. As the distribution of the femoral nerve, lateral femoral cutaneous nerve and obturator nerve is concentrated above the inguinal ligaments, the number of local anesthetics needed in the improved vertical method is reduced. Due to infection, the patient required emergency amputation, and the improved vertical method of fascia iliaca compartment block combined with general anesthesia was adopted.
Ultrasound-guided fascia iliaca compartment block provided analgesia for surgery, and reduced the dosage of general anesthetics. It also alleviated adverse cardio-vascular effects caused by pain stress, and ensured the safety of the patient during the perioperative period. The fascia iliaca compartment block also provided postoperative analgesia. The patient had a good prognosis and was subsequently discharged from the hospital.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ueda H S-Editor: Dou Y L-Editor: Filipodia E-Editor: Xing YX
| 1. | Haines L, Dickman E, Ayvazyan S, Pearl M, Wu S, Rosenblum D, Likourezos A. Ultrasound-guided fascia iliaca compartment block for hip fractures in the emergency department. J Emerg Med. 2012;43:692-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 72] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 2. | Bullock WM, Yalamuri SM, Gregory SH, Auyong DB, Grant SA. Ultrasound-Guided Suprainguinal Fascia Iliaca Technique Provides Benefit as an Analgesic Adjunct for Patients Undergoing Total Hip Arthroplasty. J Ultrasound Med. 2017;36:433-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 3. | Singh H, Jones D. Hourglass-pattern recognition simplifies fascia iliaca compartment block. Reg Anesth Pain Med. 2013;38:467-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Frandsen JB, O'Reilly Poulsen KS, Laerkner E, Stroem T. Validation of the Danish version of the Critical Care Pain Observation Tool. Acta Anaesthesiol Scand. 2016;60:1314-1322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Kotfis K, Zegan-Barańska M, Strzelbicka M, Safranow K, Żukowski M, Ely EW; POL-CPOT Study Group. Validation of the Polish version of the Critical Care Pain Observation Tool (CPOT) to assess pain intensity in adult, intubated intensive care unit patients: the POL-CPOT study. Arch Med Sci. 2018;14:880-889. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 6. | Holcomb CN, Graham LA, Richman JS, Rhyne RR, Itani KM, Maddox TM, Hawn MT. The incremental risk of noncardiac surgery on adverse cardiac events following coronary stenting. J Am Coll Cardiol. 2014;64:2730-2739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 63] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 7. | Smith BB, Warner MA, Warner NS, Hanson AC, Smith MM, Rihal CS, Gulati R, Bell MR, Nuttall GA. Cardiac Risk of Noncardiac Surgery After Percutaneous Coronary Intervention With Second-Generation Drug-Eluting Stents. Anesth Analg. 2019;128:621-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Fleisher LA, Fleischmann KE, Auerbach AD, Barnason SA, Beckman JA, Bozkurt B, Davila-Roman VG, Gerhard-Herman MD, Holly TA, Kane GC, Marine JE, Nelson MT, Spencer CC, Thompson A, Ting HH, Uretsky BF, Wijeysundera DN. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;130:e278-e333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 204] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 9. | Ren X, Schmidt W, Huang Y, Lu H, Liu W, Bu W, Eckenhoff R, Cammarato A, Gao WD. Fropofol decreases force development in cardiac muscle. FASEB J. 2018;32:4203-4213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Krych AJ, Baran S, Kuzma SA, Smith HM, Johnson RL, Levy BA. Utility of multimodal analgesia with fascia iliaca blockade for acute pain management following hip arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2014;22:843-847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 11. | Hebbard P, Ivanusic J, Sha S. Ultrasound-guided supra-inguinal fascia iliaca block: a cadaveric evaluation of a novel approach. Anaesthesia. 2011;66:300-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 108] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 12. | Capdevila X, Biboulet P, Bouregba M, Barthelet Y, Rubenovitch J, d'Athis F. Comparison of the three-in-one and fascia iliaca compartment blocks in adults: clinical and radiographic analysis. Anesth Analg. 1998;86:1039-1044. [PubMed] |
| 13. | Deniz S, Atım A, Kürklü M, Çaycı T, Kurt E. Comparison of the postoperative analgesic efficacy of an ultrasound-guided fascia iliaca compartment block versus 3 in 1 block in hip prosthesis surgery. Agri. 2014;26:151-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 14. | Vermeylen K, Soetens F, Leunen I, Hadzic A, Van Boxtael S, Pomés J, Prats-Galino A, Van de Velde M, Neyrinck A, Sala-Blanch X. The effect of the volume of supra-inguinal injected solution on the spread of the injectate under the fascia iliaca: a preliminary study. J Anesth. 2018;32:908-913. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 42] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 15. | Foss NB, Kristensen BB, Bundgaard M, Bak M, Heiring C, Virkelyst C, Hougaard S, Kehlet H. Fascia iliaca compartment blockade for acute pain control in hip fracture patients: a randomized, placebo-controlled trial. Anesthesiology. 2007;106:773-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 213] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 16. | Hards M, Brewer A, Bessant G, Lahiri S. Efficacy of Prehospital Analgesia with Fascia Iliaca Compartment Block for Femoral Bone Fractures: A Systematic Review. Prehosp Disaster Med. 2018;33:299-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 17. | Bang S, Chung J, Jeong J, Bak H, Kim D. Efficacy of ultrasound-guided fascia iliaca compartment block after hip hemiarthroplasty: A prospective, randomized trial. Medicine (Baltimore). 2016;95:e5018. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 18. | Stevens M, Harrison G, McGrail M. A modified fascia iliaca compartment block has significant morphine-sparing effect after total hip arthroplasty. Anaesth Intensive Care. 2007;35:949-952. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 66] [Article Influence: 3.9] [Reference Citation Analysis (0)] |