Published online Aug 26, 2019. doi: 10.12998/wjcc.v7.i16.2352
Peer-review started: April 23, 2019
First decision: June 12, 2019
Revised: June 18, 2019
Accepted: June 26, 2019
Article in press: June 27, 2019
Published online: August 26, 2019
Processing time: 128 Days and 13.3 Hours
Pancreatic lipomas are thought to be very rare. Lipomas are usually easy to identify on imaging, particularly via computed tomography (CT). But sometimes it’s quite difficult to distinguish a lipoma from a well-liposarcoma without histologic result.
Here, we present a case of pancreatic lipoma in a 59-year-old female. She was asymptomatic and had no medical history of note. CT and magnetic resonance imaging revealed a mass like well-differentiated liposarcoma in the pancreatic head, positron emission tomography/CT showed a low fluorodeoxyglucose uptake and laboratory tests revealed elevated transaminase and carbohydrate antigen-199 levels. Finally, the patient underwent a pancreaticoduodenectomy. Histologically, mature adipocytes were noted in the bulk of the tumor. Accordingly, the pathologic diagnosis of the pancreatic neoplasm was lipoma. To our knowledge, this case is the first example of a suspected well-differentiated liposarcoma that was actually a pancreatic lipoma. We also highlight the radiological features distinguishing a pancreatic lipoma from a pancreatic liposarcoma and briefly review the literature.
Pancreatic lipomas show no obvious gender bias and most commonly occur in the head of the pancreas, of which the maximum diameters are often less than 5 cm, and small, asymptomatic non-compressed lipomas require follow-up only. Surgical excision should be considered when the tumor has compressed important tissues or is difficult to distinguish from a liposarcoma, the choice of surgery depends on the intraoperative presentation.
Core tip: Pancreatic lipomas are rare, especially the huge ones. Lipomas are usually easily identified on imaging, particularly via computed tomography. Here we present the first example of a suspected well-differentiated liposarcoma on imaging that was actually a pancreatic lipoma. We also highlight the radiological features distinguishing a pancreatic lipoma from a liposarcoma and briefly review the literature.
- Citation: Xiao RY, Yao X, Wang WL. A huge pancreatic lipoma mimicking a well-differentiated liposarcoma: A case report and systematic literature review. World J Clin Cases 2019; 7(16): 2352-2359
- URL: https://www.wjgnet.com/2307-8960/full/v7/i16/2352.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i16.2352
Mesenchymal tumors of the pancreas are rare, and are classified by their histological origin; they represent only 1%–2% of all pancreatic tumors[1]. Of these rare tumors, fat-originating tumors (lipomas and liposarcomas) are the rarest. Intrapancreatic lipomas were found in only 0.012% of all patients undergoing routine cross-sectional imaging[2]. A pancreatic lipoma must be distinguished from focal fat replacement, lipomatous pseudohypertrophy, and liposarcoma[3]. For the surgeon, the most important differential diagnosis is liposarcoma, which is generally easily identified on imaging [such as computed tomography (CT)]. Here, we report a huge asymptomatic pancreatic lipoma mimicking a well-differentiated liposarcoma pathologically confirmed after performing the Whipple procedure. Additionally, we found that no systematic retrospective review of pancreatic lipoma status has appeared since 2010[4]. Thus, we reviewed the literature in terms of clinical manifestations and treatments.
A 59-year-old female presented with a pancreatic mass that had been identified during a medical examination 10 d prior.
She was asymptomatic and didn’t undergo any treatment at other hospitals.
The patient had a free previous medical history.
Her medical history and family history were unremarkable.
she was 160 cm tall and weighed 64 kg. Her abdomen was soft and nontender with no palpable mass.
The laboratory data were: Alanine transaminase 95.2 U/L ( reference < 40 U/L); aspartate transaminase 67.2 U/L ( reference < 35 U/L); conjugated bilirubin 7.3 μmol/L ( reference < 6.8 μmol/L); γ-glutamyl transferase 91.4 U/L ( reference < 45 U/L); carbohydrate antigen 19-9 46.0 U/mL ( reference < 39 U/mL); and serum ferritin, 423 ng/mL ( reference < 367.1 ng/mL).
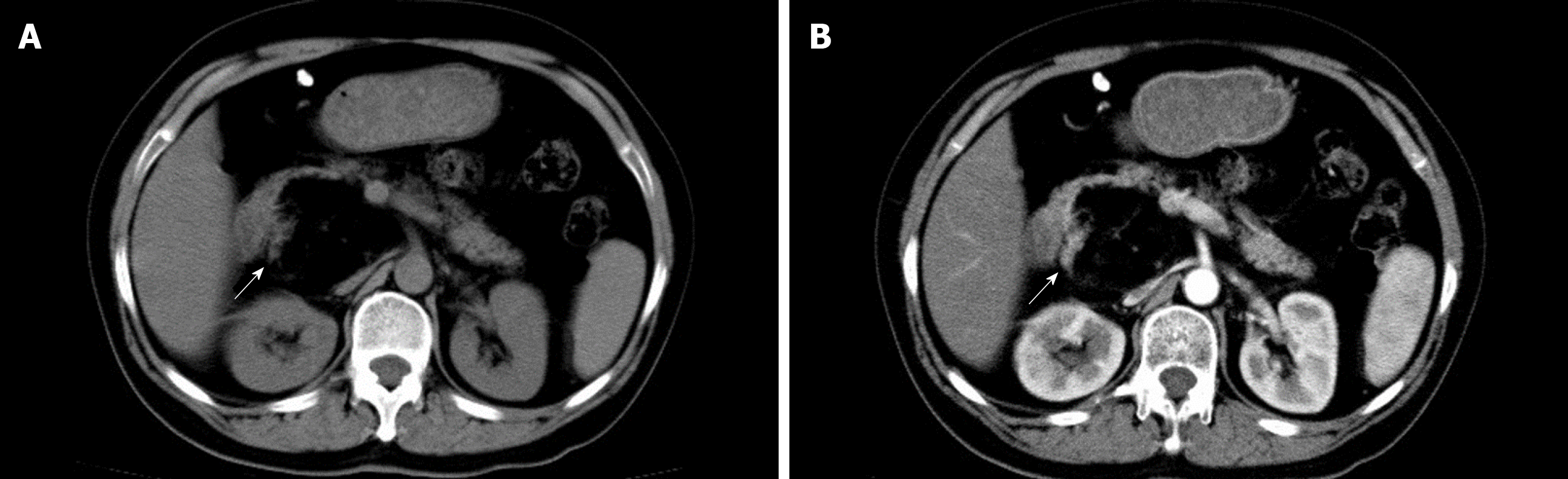
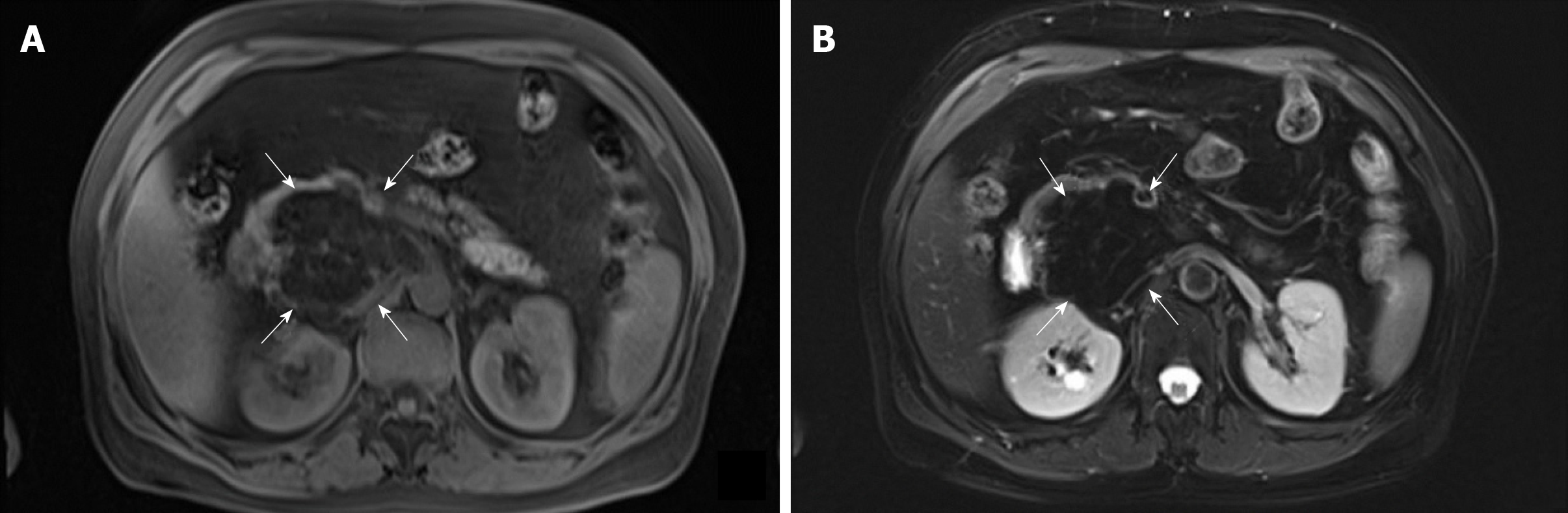
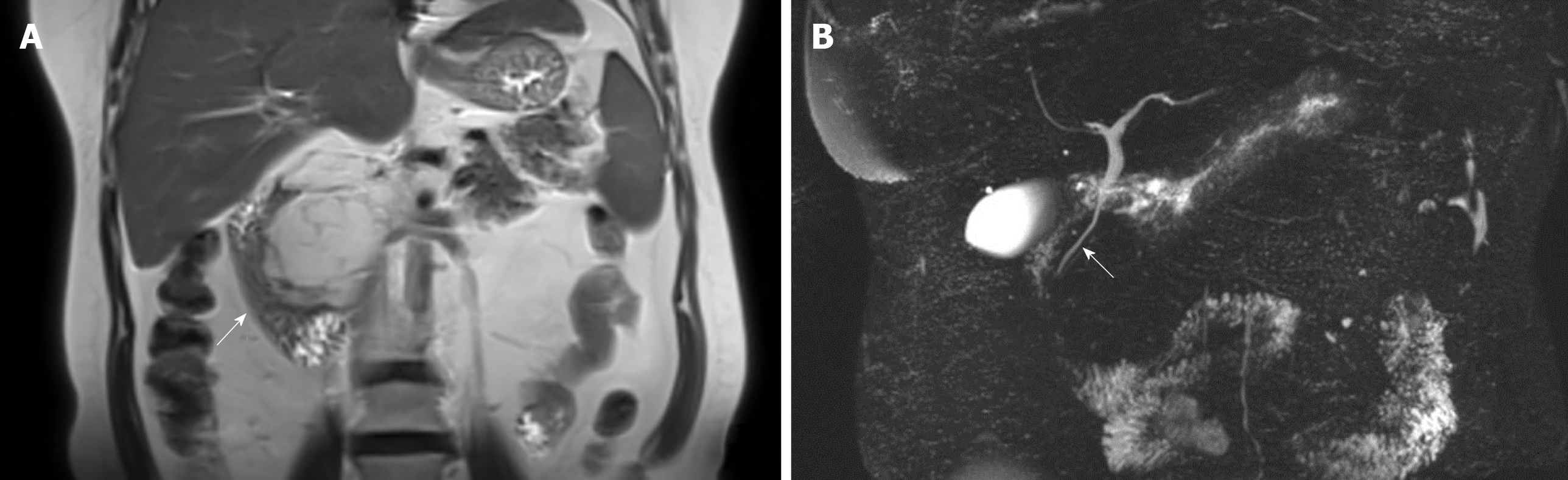
Abdominal ultrasonography revealed a hypoechoic flaky lesion of maximum diameter 5.2 cm in the head of the pancreas. Subsequent contrast-enhanced CT revealed a 6.4 cm × 6.0 cm near-circular heterogeneous fat-containing lesion (−109 ± 19.2 HU on contrast-enhanced CT compared to 47.9 ± 14.9 HU for the liver) in the head of the pancreas (Figure 1). The borders were indistinct and a few fibroreticular septa were evident within the lesion. The surrounding parenchyma was slightly enhanced, and the lesion was not clearly distinguishable from the pancreas. The adjacent tissues were partially compressed, including the head of the pancreas, the duodenum, and certain blood vessels (the inferior vena cava, portal vein, and superior mesenteric artery/vein). The pancreatic duct and intrahepatic bile ducts were not obviously dilated. By reference to the CT data only, we first considered that the mass might be a liposarcoma derived from the retroperitoneum. On magnetic resonance imaging, the mass was of high signal intensity on T2-weighted axial imaging, being isointense to the subcutaneous and intra-abdominal fat. And the fat-suppressed T1- and T2-weighted images revealed signal intensity losses, indicating that the mass was composed principally of adipose tissue (Figure 2). A few fibroreticular septa were evident within the lesion. The boundary between the lesion and the pancreas was unclear. Thus, the mass was most likely a well-differentiated liposarcoma derived from retroperitoneal fat. Magnetic resonance cholangiopancreatography revealed no dilatation or stenosis of the intrahepatic bile duct or pancreatic duct, but the middle and lower parts of the common bile duct were partially compressed. An abnormal 6.2 cm × 6.0 cm circular mixed/fatty signal emanated from the head of the pancreas (Figure 3). On positron-emission tomography/CT, the lesion had the density of fat, exhibited low fluorodeoxyglucose uptake, excluded evident distant metastasis, and was thus thought to be a non-malignant fat-derived tumor first, but it still cannot be distinguished from a well-differentiated liposarcoma.
Given the huge size and the compression of the middle and lower parts of the common bile duct and important blood vessels, we suggested surgery even if the lesion was benign. We planned total surgical excision, but found that the upper part of the mass was tightly connected to the pancreas and could not be completely excised. We feared that complete removal would increase the risk of injury to the pancreatic duct and superior mesenteric vein, which might trigger a major intraoperative hemorrhage and a postoperative pancreatic fistula that could erode the superior mesenteric vein and cause a massive hemorrhage or other complications. Thus, we switched to a pancreatoduodenectomy.
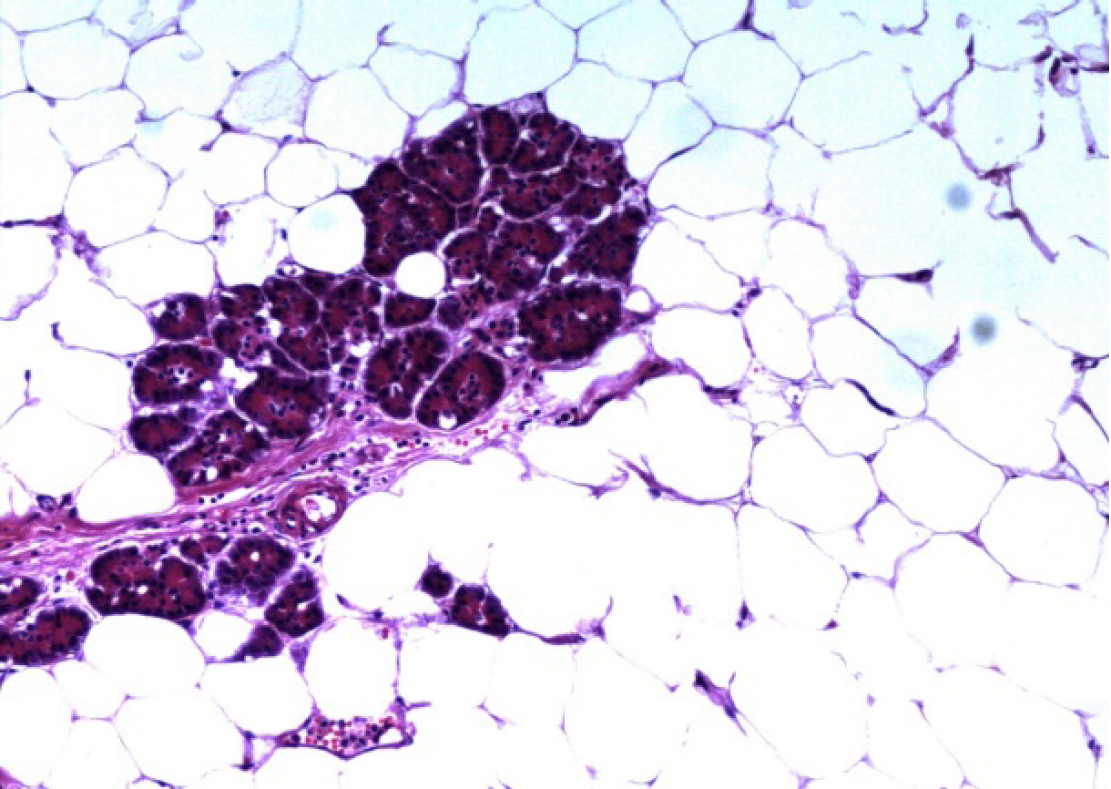
The final pathological examination confirmed a giant lipoma of the pancreas; the largest diameter was 13.0 cm (Figure 4). Two lymph nodes near the pancreas and three around the stomach evidenced chronic lymphadenitis. Pathology also revealed chronic cholecystitis with cholesterol polyps.
Postoperatively, we controlled an elevated blood glucose level, abnormal liver function, and hyperamylasemia, and the patient was discharged to home with a peritoneal drainage tube on postoperative day 25. She followed regularly to the department of general surgery.
In the time since the first report[5], 169 cases of pancreatic lipoma have been reported in 48 articles[1-3,5-49], including 10 in Chinese. Most cases were diagnosed by imaging (such as CT); only 22 were confirmed by pathology, 16 of which underwent surgery and 6 endoscopic ultrasound/fine needle aspiration (FNA). Only 2 patients underwent both FNA and surgery; these exhibited massive vascular compression by the tumor[34] and elevated serum bilirubin and alkaline phosphatase levels[15]. However, the FNA data were not described. Some have argued that pancreatic lipomas are not rare[2,22]. The sexes of 162 of the 169 cases were identified: 87 males and 75 females. Their ages ranged from 11 months to 88 years. Lipomas are most commonly found in the middle-aged and elderly, possibly because they undergo physical examinations more often than do the young. The pancreatic lipoma locations were: The head (n = 70); the head and the uncinate process (n = 1); the uncinate process (n = 15); the head and neck (n = 2); the neck (n = 9); the neck and body (n = 1); the body (n = 30); the body-tail junction (n = 3); the tail (n = 34); and not mentioned (n = 4) . Only a few tumors were of diameter > 50 mm: < 50 (n = 150); 50–100 (n = 9); and > 100 mm (n = 3). Most patients were asymptomatic and required only follow-up or conservative treatment (n = 132); only 16 required operations, including pancreatoduodenectomy (7), tumor enucleation from the head (3), subtotal pancreatectomy and splenectomy (1), pancreatic tail resection (1), biliary bypass (1), and not mentioned (3). In patients who underwent surgery, postoperative complications were mentioned in only two cases; these were an elevated blood glucose level and a pancreatic fistula.
A pancreatic lipoma is a rare solid tumor, the etiopathogenesis of which remains unclear although lipomas located in the pancreatic head have been considered to be adipose tissue trapped during posterior rotation of the ventral pancreatic bud[22,48].
CT is the most useful radiological method to diagnose pancreatic lipoma[4]. The density of a liposarcoma in CT is higher than that of normal fat and benign fatty masses, and indistinct borders[50], thick septa[48,51] , a larger size[48,52] (> 5 cm, and in most cases > 10 cm)[1], calcification[48,52] and rapid growth[48] are significant indicators of malignancy. Features of well-differentiated liposarcoma include large lesion size, presence of thick septa, presence of nodular and/or globular or non-adipose mass-like areas, and decreased percentage of fat composition[52]. A lipoma is usually well circumscribed, of the density of normal fat, homogenous[4], noninvasive[50], stable and devoid of symptoms. However, it is not easy to distinguish a lipoma from a well-differentiated liposarcoma due to the radiographic similarities between these two lesions[4] (Table 1).
| Clinical Manifestation | Cases (n) | Percentage, % | |
| Sex | Male | 87 | 53.7 |
| Female | 75 | 46.3 | |
| Locations of the tumor | Head | 70 | 42.4 |
| Tail | 34 | 20.6 | |
| Body | 30 | 18.2 | |
| Uncinate process | 15 | 9.1 | |
| Neck | 9 | 5.5 | |
| Body-tail junction | 3 | 1.8 | |
| Head-neck junction | 2 | 1.2 | |
| Head - uncinate process junction | 1 | 0.6 | |
| Neck and body junction | 1 | 0.6 | |
| Tumor size, mm | < 50 | 150 | 92.6 |
| 50-100 | 9 | 5.6 | |
| > 100 | 3 | 1.9 | |
| Treatment | Follow-up or conservative treatment | 132 | 89.2 |
| Pancreatoduodenectomy | 7 | 4.7 | |
| Tumor enucleation in head | 3 | 2.0 | |
| Subtotal pancreatectomy with a splenectomy | 1 | 0.7 | |
| Pancreatic tail resection | 1 | 0.7 | |
| Biliary bypass | 1 | 0.7 | |
| Type of surgery not mentioned | 3 | 2.0 |
To our knowledge, our case is the first example of a suspected well-differentiated liposarcoma that was actually a pancreatic lipoma. The tumor of our present patient was around 6.2 cm × 6.0 cm in dimensions, indistinct from the pancreas, contained a few fibroreticular septa, and the surrounding parenchyma was slightly enhanced. We first thought that the mass was a well-differentiated liposarcoma derived from the retroperitoneum. Despite that positron emission tomography/CT showed low fluorodeoxyglucose uptake, the diagnosis was still uncertain. Thus, given the huge size and the compression of the middle and lower parts of the common bile duct and important blood vessels, we suggested surgery even if the lesion was benign. We planned total surgical excision, but found that the upper part of the mass was tightly connected to the pancreas and could not be completely excised. We feared that complete removal would increase the risk of injury to the pancreatic duct and superior mesenteric vein, which might trigger a major intraoperative hemorrhage and a postoperative pancreatic fistula that could erode the superior mesenteric vein and cause a massive hemorrhage or other complications. Thus, we switched to a pancreatoduodenectomy.
Pancreatic lipoma seems to exhibit no gender bias, is usually diagnosed via CT or other imaging methods, and most commonly occurs in the head of the pancreas. The maximum diameter is often less than 5 cm. Generally, small, asymptomatic non-compressed lipomas require follow-up only. Very few cases exhibit significant short-term changes, but the lipoma may grow in the long term[25]. Patients may elect to undergo trans-duodenal core needle biopsy if the tumor is difficult to identify on imaging. Surgery is recommended if a malignancy is in play. However, it is sometimes difficult to distinguish lipomas from well-differentiated liposarcomas[53]. A combination of FNA data and MDM2 genetic analysis improves the liposarcoma detection rate[54,55]. In addition, short-term close follow-up may identify patients with enlarging lesions that require surgery. Compressive lesions, such as that of our present case, require excision; the choice of surgery varies by the intraoperative presentation.
In summary, pancreatic lipomas are rare, especially the huge ones, no obvious gender bias, and most commonly occur in the head of the pancreas. Small, asymptomatic non-compressed lipomas require follow-up only. Surgical excision should be considered when the tumor has compressed important tissues or is difficult to distinguish from a liposarcoma, the choice of surgery depends on the intraoperative presentation.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ozyigit G, Yamagata M S-Editor: Cui LJ L-Editor: Wang TQ E-Editor: Wu YXJ
| 1. | Ferrozzi F, Zuccoli G, Bova D, Calculli L. Mesenchymal tumors of the pancreas: CT findings. J Comput Assist Tomogr. 2000;24:622-627. [PubMed] |
| 2. | Butler JR, Fohtung TM, Sandrasegaran K, Ceppa EP, House MG, Nakeeb A, Schmidt CM, Zyromski NJ. The natural history of pancreatic lipoma: Does it need observation. Pancreatology. 2016;16:95-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Katz D, Hines J, Math K, Nardi P, Mindelzun R, Lane M. Using CT to reveal fat-containing abnormalities of the pancreas. Ajr Am J Roentgenol. 1999;172:393-396. [RCA] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 59] [Article Influence: 2.3] [Reference Citation Analysis (1)] |
| 4. | Zhan HX, Zhang TP, Liu BN, Liao Q, Zhao YP. A systematic review of pancreatic lipoma: how come there are so few cases? Pancreas. 2010;39:257-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Bigard MA, Boissel P, Regent D, Froment N. Intrapancreatic lipoma. First case in the literature. Gastroenterol Clin Biol. 1989;13:505-507. [PubMed] |
| 7. | Agnello K, Gurtoo L, Kumar M, Bain A, Singh A. Pancreatic Lipoma Masquerading As A Cystic Neoplasm. Am J Gastroenterol. 2014;109:297-298. |
| 8. | Aithal Sitharama S, Bashini M, Gunasekaran K, Barathi Subramania D. Pancreatic lipoma: a pancreatic incidentaloma; diagnosis with ultrasound, computed tomography and magnetic resonance imaging. BJR Case Rep. 2016;2:20150507. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Bean MJ, Fishman EK. Focal FDG uptake in a pancreatic lipoma mimicking malignancy. J Comput Assist Tomogr. 2005;29:475-476. [PubMed] |
| 10. | Boglino C, Inserra A, Silvano A, Ciprandi G, Boldrini R, Caione P. [Intrapancreatic lipoma: a case report]. Pediatr Med Chir. 1993;15:397-399. [PubMed] |
| 11. | Bozgeyik Z, Kocakoc E, Koc M. Education and imaging. Hepatobiliary and pancreatic: pancreatic lipoma. J Gastroenterol Hepatol. 2008;23:161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Budzyńska A, Nowakowska-Duława E, Cholewka A, Pilch-Kowalczyk J, Kajor M. Large pancreatic lipoma in a 69-year-old diabetic woman: diagnostic considerations. Prz Gastroenterol. 2014;9:168-171. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Celis Zapata J, Berrospi Espinoza F, Valencia Mariñas HD, Sánchez Lihón J, Abad Licham M, Farías Mejía I. [Pancreatic lipoma: presentation of a case and review of literature]. Rev Gastroenterol Peru. 2008;28:56-59. [PubMed] |
| 14. | Cheng W, Ji AB, and Shi YF. CT findings of pancreatic lipoma: An analysis of 2 cases [in Chinese]. Morden Medicine J China. 2009;11:31-32. |
| 15. | De Jong SA, Pickleman J, Rainsford K. Nonductal tumors of the pancreas. The importance of laparotomy. Arch Surg. 1993;128:730-734; discussion 734-736. [PubMed] |
| 16. | Deschner B, Gandhi J, Deneve JL, Dickson PV, Clark I, Glazer ES. Symptomatic Pancreatic Lipoma. J Gastrointest Surg. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Di Maggio EM, Solcia M, Dore R, Preda L, La Fianza A, Rodino C, Campani R. Intrapancreatic lipoma: first case diagnosed with CT. AJR Am J Roentgenol. 1996;167:56-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 21] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Di Matteo FM, Shimpi L, Pandolfi M, Rabitti C, Fabio C, Gabbrielli A, Costamagna G. EUS diagnosis of pancreatic lipoma: a case report. Gastrointest Endosc. 2006;64:146-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Erdem LO, Erdem CZ, Comert M. Intrapancreatic lipoma and Morgagni hernia: a previously unrecognized association. Dig Dis Sci. 2004;49:1962-1965. [PubMed] |
| 20. | Fan JD. Pancreatic lipoma: a case report [in Chinese]. Chin J Radiol. 1995;29:427-428. |
| 21. | Gao T, Hou KY. Pancreatic lipoma: a case report [in Chinese]. Chin J Gen Surg. 1996;5:50. |
| 22. | Hois E, Hibbeln J, Sclamberg J. CT appearance of incidental pancreatic lipomas: a case series. Abdominal Imaging. 2006;31:332. [RCA] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Itai Y, Saida Y, Kurosaki Y, Kurosaki A, Fujimoto T. Focal fatty masses of the pancreas. Acta Radiol. 1995;36:178-181. [PubMed] |
| 24. | Kanemoto A, Toyama N, Noda H, Konishi F. A case of pancreatic lipoma: CT examination. Nihon Shokakibyo Gakkai Zasshi. 2007;104:1387-1391. [PubMed] |
| 25. | Kawahata S, Kawakami H, Kubota Y. A Case of Pancreatic Lipoma With Morphological Change During Long-Term Follow-up. Pancreas. 2017;46:e66-e67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | Kishan TV, Pavithra S, Sri Bhuvana N, Kotha VK, Moorthy RS. A rare tumour of pancreas in an incidentally discovered pancreatic lipoma. Med J Armed Forces India. 2015;71:S138-S140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 27. | Lee JY, Seo HI, Park EY, Kim GH, Park DY, Kim S. Histologic confirmation of huge pancreatic lipoma: a case report and review of literatures. J Korean Surg Soc. 2011;81:427-430. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 28. | Lee SY, Thng CH, Chow PKh. Lipoma of the pancreas, a case report and a review of the literature. World J Radiol. 2011;3:246-248. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 29. | Liu K, Wang J. Pancreatic lipoma: a case report [in Chinese]. J. Hepatopancreatobil Surg. 2011;23:255. |
| 30. | Liu W, Ji M, Lu F. Pancreatic lipoma: A case report [in Chinese]. Chinese Computed Medical Imaging. 2010;16:178-179. [DOI] [Full Text] |
| 31. | Magenta Biasina A, Curti A, Bonifacio C, Soldi S, Cornalba GP. CT diagnosis of pancreatic lipoma: a case report and Literature review. Radiol Med. 2002;104:367-369. [PubMed] |
| 32. | Merli M, Fossati GS, Alessiani M, Spada M, Gambini D, Viezzoli A, Di Maggio E, Vailati A, Breyer S, Paltro R, Zonta A. A rare case of pancreatic lipoma. Hepatogastroenterology. 1996;43:734-736. [PubMed] |
| 33. | Pausawasdi N, Apisarnthanarak P, Pongpaibul A, Charatcharoenwitthaya P. Pancreatic lipoma diagnosed by EUS-FNA. Gastrointest Endosc. 2012;76:668-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 34. | Raut CP, Fernandez-del Castillo C. Giant lipoma of the pancreas: case report and review of lipomatous lesions of the pancreas. Pancreas. 2003;26:97-99. [PubMed] |
| 35. | Ryan MF, Hamilton PA, Smith AJ, Khalifa M. Radiologic features of pancreatic lipoma. Can Assoc Radiol J. 2003;54:41-44. [PubMed] |
| 36. | Sato K, Takagi H, Ishibashi A, Koyama Y, Mori M. Small pancreatic lipoma: case report and literature review. Hepatogastroenterology. 2007;54:1582-1584. [PubMed] |
| 37. | Secil M, Igci E, Goktay AY, Dicle O. Lipoma of the pancreas: MRI findings. Comput Med Imaging Graph. 2001;25:507-509. [PubMed] |
| 38. | Si S, Zhang TP, Dong J, Chen G Zhao YP. Pancreatic lipoma: a case report [in Chinese]. Chin J Hepatobiliary Surg. 2010;16:219-220. [DOI] [Full Text] |
| 39. | Stadnik A, Cieszanowski A, Bakoń L, Grodzicka A, Rowiński O. Pancreatic lipoma: An incydentaloma which can resemble cancer - analysis of 13 cases studied with CT and MRI. Pol J Radiol. 2012;77:9-13. [PubMed] |
| 40. | Suzuki R, Irisawa A, Hikichi T, Shibukawa G, Takagi T, Wakatsuki T. Pancreatic lipoma diagnosed using EUS-FNA. A case report. JOP. 2009;10:200-203. |
| 41. | Tana C, Mezzetti A, Schiavone C. Extremely rare case of acute edematous pancreatitis associated with an incidental pancreatic lipoma. Ultraschall in der Medizin-European J Ultrasound. 2013;34. [DOI] [Full Text] |
| 42. | Wang ZB, Tai S, Sun DS, Cui YF. Surgical removal of pancreatic lipoma: a case report [in Chinese]. China Morden Doctor. 2011;49:114. |
| 43. | Xu QW, Liu LM. Pancreatic lipoma: a case diagnosed by CT [in Chinese]. Chinese J Medical Imaging Technology. 2001;17:815. [DOI] [Full Text] |
| 44. | Yan W, Dorsey J, Williams V, Pawa S. A Rare Case of Pancreatic Lipoma Diagnosed by Endosonographically Guided Fine Needle Aspiration. Am J Gastroenterol. 2013;108:268. |
| 45. | Katz D, Nardi P, Hines J, Barckhausen R, Math K, Fruauff A. Lipomas of the pancreas. AJR. Am J Roentgenol. 1998;170:1485-1487. |
| 46. | Li XQ, Jin EH, Zhang BB. Study of CT and MRI diagnosis for the pancreatic lipomas [in Chinese]. CT Theory and Applications. 2014;23:601-610. |
| 47. | Su C, Liu JG, Wei CK, Wang QB. Laparoscopic surgery for removal of pancreatic lipoma: A case report [in Chinese]. J Taishan Medical College. 2018;39:340-341. [DOI] [Full Text] |
| 48. | Karaosmanoglu D, Karcaaltincaba M, Akata D, Ozmen M, Akhan O. Pancreatic lipoma computed tomography diagnosis of 17 patients and follow-up. Pancreas. 2008;36:434-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 49. | Barutcu O, Cihangiroglu M, Yildirim T, Kayaselcuk F, Noyan T. Fat containing unusual tumor of the pancreas. Eur Radiol. 2002;12:770-773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 50. | Waligore MP, Stephens DH, Soule EH, McLeod RA. Lipomatous tumors of the abdominal cavity: CT appearance and pathologic correlation. AJR Am J Roentgenol. 1981;137:539-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 63] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 51. | Machado MC, Fonseca GM, de Meirelles LR, Zacchi FF, Bezerra RO. Primary liposarcoma of the pancreas: A review illustrated by findings from a recent case. Pancreatology. 2016;16:715-718. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 52. | Kransdorf MJ, Bancroft LW, Peterson JJ, Murphey MD, Foster WC, Temple HT. Imaging of fatty tumors: distinction of lipoma and well-differentiated liposarcoma. Radiology. 2002;224:99-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 325] [Cited by in RCA: 317] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 53. | O'Donnell PW, Griffin AM, Eward WC, Sternheim A, White LM, Wunder JS, Ferguson PC. Can Experienced Observers Differentiate between Lipoma and Well-Differentiated Liposarcoma Using Only MRI? Sarcoma. 2013;2013:982784. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 49] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 54. | Thway K, Flora R, Shah C, Olmos D, Fisher C. Diagnostic utility of p16, CDK4, and MDM2 as an immunohistochemical panel in distinguishing well-differentiated and dedifferentiated liposarcomas from other adipocytic tumors. Am J Surg Pathol. 2012;36:462-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 164] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 55. | Brisson M, Kashima T, Delaney D, Tirabosco R, Clarke A, Cro S, Flanagan AM, O'Donnell P. MRI characteristics of lipoma and atypical lipomatous tumor/well-differentiated liposarcoma: retrospective comparison with histology and MDM2 gene amplification. Skeletal Radiol. 2013;42:635-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 104] [Article Influence: 8.7] [Reference Citation Analysis (0)] |