Published online Aug 6, 2019. doi: 10.12998/wjcc.v7.i15.2120
Peer-review started: February 27, 2019
First decision: May 31, 2019
Revised: June 22, 2019
Accepted: July 2, 2019
Article in press: July 3, 2019
Published online: August 6, 2019
Processing time: 161 Days and 9.1 Hours
Most major abdominal vascular injuries are caused by penetrating injuries. A common iliac artery occlusion caused by blunt force trauma is rare, and very few cases have been reported. Because of this low incidence, atypical symptoms, and frequent association with other severe injuries, the proper diagnosis tends to be missed or delayed. The gold standard for diagnosis is angiography, and treatment remains a challenge.
We report here the unusual case of a common iliac artery occlusion caused by blunt abdominal compressive trauma, with transection of the small intestine. At presentation, the patient (a 56-year-old man) complained of pain and numbness in the left lower extremity and severe pain in the whole abdomen. Physical examination showed total abdominal tenderness with evidence of peritoneal irritation. The left lower limb was pulseless and cold. Abdominal computed tomography examination revealed digestive tract perforation, and abdominal computed tomography angiography showed left common iliac artery occlusion. The patient was treated successfully by anastomosis of the intestine, percutaneous transluminal angioplasty, and stenting. The patient was followed for more than 11 mo after the operation and showed a good recovery.
Patients with abdominal trauma should be suspected of having major vascular injury. Individualized treatment strategies are needed for this condition.
Core tip: Most major abdominal vascular injuries are caused by penetrating injuries. As a subset of arterial blunt trauma, the percentage of iliac arterial injury is small. Common iliac artery occlusion in blunt trauma is especially uncommon. We report such a rare case here. Furthermore, we review the reported cases in the English literature and provide a discussion on the mechanism of injury, clinical presentation and signs, diagnosis, surgical modalities, and outcome.
- Citation: Zhou YX, Ji Y, Chen J, Yang X, Zhou Q, Lv J. Common iliac artery occlusion with small intestinal transection caused by blunt abdominal trauma: A case report and review of the literature. World J Clin Cases 2019; 7(15): 2120-2127
- URL: https://www.wjgnet.com/2307-8960/full/v7/i15/2120.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i15.2120
Penetrating rather than blunt trauma causes the greatest majority of vascular injuries. As a subset of arterial blunt trauma, the percentage of iliac arterial injury is small. The largest review of these cases in the literature was published by Tuech et al[1], who reviewed 9 patients with common iliac artery occlusion in blunt trauma. We add to these rare cases in the literature by reporting a new case here. Furthermore, we review 7 cases reported between the years of 2001 and 2018, and discuss the mechanism of injury, clinical presentation and signs, diagnosis, surgical modalities, and outcome.
A 56-year-old male steel worker's lower abdomen had been compressed between two forklifts. He was admitted to the People’s Hospital of Jingjiang with pain and numbness in the left lower extremity and severe pain throughout the entire abdomen, especially in the lower abdomen.
The patient had no significant medical history.
The patient had no significant family history.
The patient showed clear consciousness upon presentation. Physical examination showed stable vital signs, including blood pressure of 136/68 mmHg (normal range: 90-140/60-90 mmHg), pulse rate of 95/min (normal range: 60/min-100/min), respiratory rate of 16/min (normal range: 16/min-20/min), and temperature of 37.0 °C (normal range: 36.1°C-37°C). No obvious contusion of the abdominal wall or the left lower limb was noted. He had total abdomen tenderness, with evidence of peritoneal irritation and obvious board-like rigidity of the abdomen. The left lower extremity had good mobility but it was painful and numb, and skin temperature was significantly decreased. Pulsation of the left dorsal pedal artery had disappeared.
Laboratory examination revealed a hemoglobin level of 152 g/L (normal range: 130-175 g/L), white blood cell count of 13.2 × 109/L (normal range: 3.5 × 109/L to 9.5 × 109/L), and neutrophil percentage of 94.6% (normal range: 40%-75%).
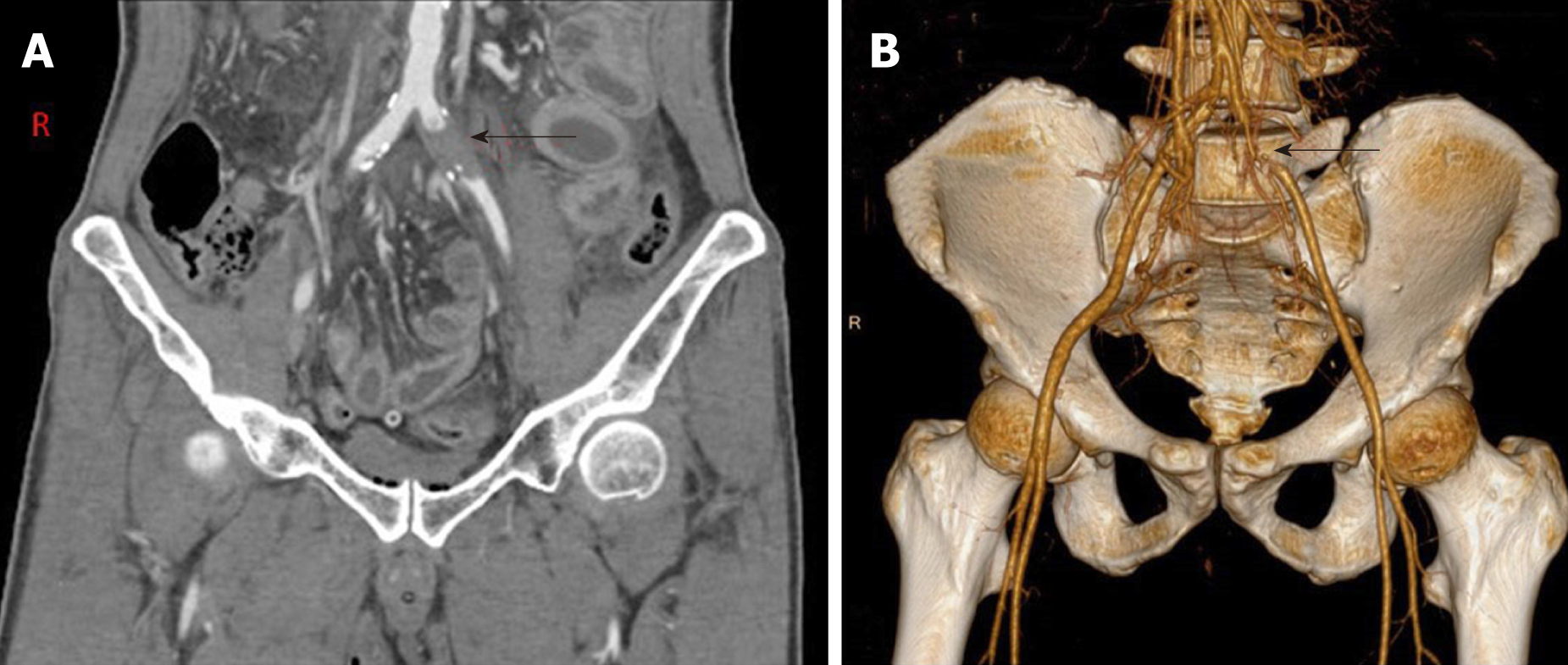
Pre-hospitalization abdominal computed tomography examination had revealed a perforation of the digestive tract. Abdominal computed tomography angiography showed occlusion of the left common iliac artery (Figure 1) and atherosclerosis of the abdominal aorta, bilateral iliac artery, and lower right femoral artery.
Common iliac artery occlusion with transection of the small intestine caused by blunt abdominal trauma.
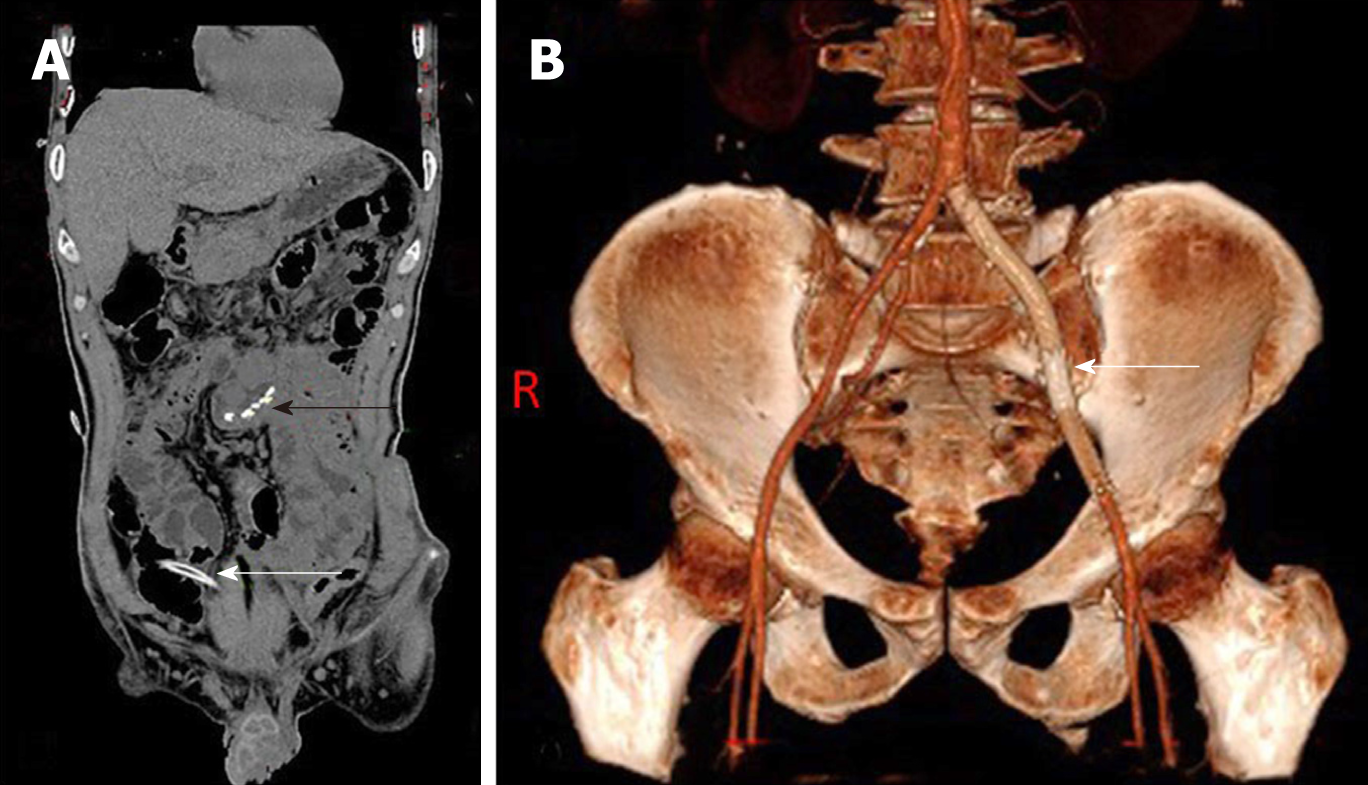
The patient underwent laparotomy under general anesthesia. Surgical findings included transection of the small intestine at about 2 m away from the ileocecus, without bleeding in the mesentery. About 200 mL of pus was found in the pelvic and abdominal cavity. We performed a partial small bowel resection and then a side-to-side small bowel anastomosis using a linear cutting closer (Figure 2A).
The abdominal symptoms of discomfort were completely relieved after the operation; however, the symptom of discomfort in the left leg became more prominent. The patient was immediately transferred to a superior hospital, where arteriography of the left lower extremity was performed, followed by percutaneous transluminal angioplasty with stenting at 4 d later. Unfortunately, the details of those operations were not available.
The postoperative course was uneventful. Physical examination revealed a warm left leg with restoration of pulse and normal sensation. Re-examination by abdominal computed tomography showed good position of the left common iliac artery stent (Figure 2B). The patient was followed for more than 11 mo after the operation and recovered well.
Injury to the common iliac artery secondary to blunt trauma is rare[2-6]. The reported rates of incidence of iliac artery injuries from trauma range from 0.4% to 7.1%[2,7]. The rare nature of this injury is largely due to the vessel’s position in the retroperitoneal location, where it is protected by the bony pelvic girdle[5,6]. A total of only 8 cases, including our case reported herein, are present in the literature[8-14]. We have summarized the data from these cases on age, sex, causes of injury, location, clinical presentation and signs, findings of auxiliary examination, and associated injuries in Table 1. The data on operative delay time, procedure, fasciotomy, and outcomes are summarized in Table 2. The total 8 patients include 7 males and 1 female, with a mean age of 40 years old (range: 9-74 years). The causes of injury were seatbelt syndrome in 3 of the patients, direct compression injury in 4, and car crash in 1. Common iliac artery occlusion occurred on the left and bilateral sides in 2 cases each and on the right in 4. All 8 cases were diagnosed in time. Except for the youngest case among the total 8 and our case, the other 6 cases were treated immediately after admission. Four cases had a good prognosis. For the other 4 cases, 2 died, 1 suffered paralysis in the right leg, and 1 became paraplegic.
| Age (sex) | Cause of injury | Location | Symptom and sign | Auxiliary examination | Associated injuries |
| 44 (M) | Car crash | Right | Cold right lower leg; absent right femoral, popliteal, and pedal pulses; absent left popliteal and pedal pulses | Angiography | Subarachnoid and intraventricular hemorrhage and diffuse axonal injury; subcapsular hematoma of the liver, splenic laceration, comminuted fracture of the left iliac wing, and widening of the left sacroiliac joint; contusion of the mid-abdomen |
| 27 (M) | Crushed between a fork-lift truck and a concrete platform | Bilateral | Cold and loss of motor function for both feet, with the right foot being worse; no femoral or pedal pulse | Doppler scanning; arteriography | Pelvic and right acetabular fracture; retroperitoneal bladder rupture; abdominal wall disruption |
| 74 (F) | Seatbelt injury | Bilateral (aortic bifurcation disruption) | Pulseless and cold | No | Contusion of chest wall and left lung; complete disruption of the lower abdominal muscles; intestinal transection with mesenteric disruption |
| 26 (M) | Abdominal and lumbar spine compression in a metal press | Left | Cold and pale; reduction of power and sensory loss; no pulsation of the femoral artery | ACTA | Contusion of the abdominal wall; retroperitoneal hematoma in the left psoas muscle |
| 9 (M) | Seatbelt-related injury | Right (aortic dissection) | A cold right lower leg | MRA | Intestinal perforation; fractures of the lumbar spine |
| 51 (M) | Abdomen compression by a tractor against a house wall | Right (aortic dissection) | Cold and pale; no palpable artery pulses | ACTA | Traumatic perforations of the ileum and transversal colon |
| 35 (M) | Seatbelt injury | Right | Absent right femoral, popliteal, and posterior tibial pulses | No | Multiple scalp and face lacerations; bowel transections of descending colon and one segment of the small bowel |
| 56 (M) | Lower abdomen compression between two forklifts | Left | Pain; cold and numb; pulsation of the left dorsal pedal artery disappeared | ACTA | Transection of small intestine |
| Operative delay time | Procedure | Fasciotomy | Result |
| < 4 h | Endovascular stenting | No | Died due to complications of brain injury |
| Shortly after admission | Endovascular stenting | Right | Right leg paralysis persisted secondary to severe lumbar plexus nerve injury |
| Shortly after admission | Aortoiliac bypass with spiraled saphenous vein graft | Bilateral | Died due to severe acute respiratory distress syndrome and associated pulmonary sepsis |
| Shortly after admission | Endovascular stenting | No | Good |
| After 4 d | Endovascular stenting | Right | Well-perfused right lower limb with normal pulses but paraplegic |
| Shortly after admission | Use of anterior longitudinal ligament and great saphenous vein graft | No | Good |
| Approximately 3 h | Segmental excision and internal iliac artery patch angioplasty | No | Good |
| After 4 d | Endovascular stenting | No | Good |
The most common mechanisms of injury appear to be direct anteroposterior compressions[6,15], traction from displaced bone fragments[16], and shearing forces, possibly accentuated by use of a seatbelt[17]. In fact, the mechanism of seatbelt syndrome or deceleration injury can also be understood as a type of abdominal compression. A total of 13 patients have been reported with common iliac artery occlusion due to direct anteroposterior compression[1]. We also found 4 cases of direct anteroposterior compression. It would be reasonable to assume then that abdominal compression is the main cause of common iliac artery occlusion. Blunt trauma-induced abdominal aortic injuries most frequently result in intimal tearing. Atherosclerotic disease has been postulated as a predisposing factor for aortic intimal tearing because of intimal weakening and loss of both elasticity and compliance[15,18]. In our patient, abdominal computed tomography angiography examination showed atherosclerosis of the abdominal aorta, bilateral iliac artery, and lower right femoral artery. We can speculate that the occlusion of the left common iliac artery may also have been caused by atherosclerotic plaque rupture. Endometrial tear, atherosclerotic plaque rupture, and intramural hematoma formation can lead to common iliac artery diameter reduction or even occlusion. If the compression force is strong enough, it may lead to transection of the common iliac artery[19].
Because of the low incidence of this injury, its atypical symptoms, and frequent association with other severe injuries, the diagnosis is often missed or delayed. This can cause serious harm to the patients. Therefore, our attention should be focused on proper identification and early diagnosis. The clinical manifestations and signs of acute lower limb ischemia can provide important clues for the diagnosis. It is important to note that acute limb ischemia caused by common iliac artery occlusion from blunt abdominal trauma is rare[2,5] and clinical presentation may be delayed for months or years[6,17]. Tuech et al[1] reported the median operative delay time to be 15 d, ranging from 3 d to 36 years. All of the 8 cases we reviewed (including our own) presented acute lower limb ischemia. This may be the main reason why they were able to receive timely diagnosis and treatment. Except for the youngest patient and our patient among these 8 total cases, the other 6 patients were diagnosed and treated shortly after admission. The youngest and our patient were also diagnosed shortly after admission but the surgery was performed 4 d later. For the former, given the patient's young age and incomplete occlusion with severe multiple injuries, a conservative initial approach was decided. For the latter, we delayed operation due to the incomplete occlusion allowing for a longer observation period.
Most patients present with other injuries, such as traumatic intestinal perforation, pelvic fracture, liver and spleen injury, bladder rupture, and contusion of the thoracoabdominal wall, among others. Treating clinicians should be especially careful with these patients because the signs and symptoms of vascular injury may be obscured by the signs and symptoms of other injury, especially in those patients who do not show acute lower limb ischemia. It is very important to inquire about the patient's detailed medical history and to perform a meticulous physical examination. In addition, it is also necessary to go to the bedside frequently, to observe any changes in the patient’s condition because changes in emergency patients are dynamic.
Angiography is the gold standard for diagnosis and should be performed when there is a clinical doubt. The development of abdominal computed tomography angiography has allowed for three-dimensional reconstruction of the blood vessels and a clearer assessment of the location and extent of damage, which can help surgeons in deciding on the correct treatment strategies. The precondition of angiography is the hemodynamic stability of the patient. It is generally contrain-dicated in a hemodynamically unstable patient with multisystem injury; for these patients, duplex ultrasonography may be helpful. Among the total 8 cases discussed herein, 6 underwent angiography, 3 of which were given the abdominal computed tomography angiography; the 2 other patients did not undergo any blood vessel examination.
Once injury to the common iliac artery has been determined, operative repair is generally indicated. The surgical procedure includes both open and endovascular approaches. Ligation of the iliac artery results in an unacceptable amputation rate of up to 50%[7]. Major vessels should be ligated only when the procedure is considered to be life-saving or in the presence of gross contamination, where subsequent extra-anatomical grafting is possible[2]. The loss of 1.5 cm of vessel is the maximum length that can be dealt with by mobilization and end-to-end anastomosis[2,13]. Furthermore, the vascular wall must be normal before anastomosis and the anastomotic site must be free of tension. Long segment injury may require substitution of a vascular conduit[20].
Autologous vein grafts and synthetic grafts are available. At present it is still debatable which is better - an autologous vein graft or a synthetic graft. Autologous grafting with the hypogastric artery or saphenous vein on injured iliac arteries may give rise to the problems of size discrepancies and time consumption in harvest, making these grafts unfavorable[1,5]. Synthetic grafts are more favorable as they are available in various sizes, but they are not ideal in cases of peritoneal contamination from concomitant bowel perforation. Several articles have provided evidence that polytetrafluoroethylene grafts may be used in the face of substantial contamination and may be resistant to subsequent infection[21,22].
Extra-anatomic bypass and femorofemoral or axillofemoral bypass are alternatives. Endovascular techniques have been used to treat a variety of endovascular diseases[23-26]. The endovascular approach offers benefits in terms of easier access to the target lesion, reduction in blood transfusion requirement, and obviation of the potential need for systemic heparinization[13]. Among the total 8 patients discussed herein, 5 underwent endovascular stenting and the remaining 3 underwent open surgery. Jovanovic et al[11] consider that reinforcement of the posterior aortic wall to the anterior longitudinal ligament should be added to the armamentarium of aortic injury treatment. In our case, the final choice of endovascular therapy may have resulted from consideration of the patient’s hemodynamic stability, absence of vessel rupture, and severe abdominal cavity contamination.
Considering that most patients with this injury present with multiple other severe injuries, it is important to remember that the primary purpose of treatment is to save the patient’s life. Therefore, the principles of simplicity and efficiency must be satisfied when choosing the therapeutic method. Endovascular therapy has the advantages of being minimally invasive, having little effect on the patient, and producing clear effect, all of which conform to the above two principles. Among the total 8 patients discussed herein, 2 did not receive surgery until 4 d after the diagnosis and neither experienced serious repercussions.
Taking into account the information presented in previous literature reviews of this injury, we noted the consequence of short-term ischemic necrosis of the affected limb to be infrequent. Therefore, within the time allowed, the most serious injury endangering the patient’s life should be addressed first, followed by the compression injury of the lower abdomen when the patient's general condition has stabilized. It is important to avoid multi-organ surgery and long anesthesia time associated with a one-stage operation, especially for patients who are elderly, have underlying basic diseases, or are seriously injured. This is consistent with the current damage control theory; however, the premise is to closely observe changes in the patient’s condition. Once the limb is found to have the tendency of ischemic necrosis, immediate surgical intervention should be initiated.
Compartment syndrome should be anticipated after revascularization. Postoperative increase in pain in the distal limb, any evidence of decreased perfusion, increasing neurological signs, or limb swelling warrant fasciotomy without delay[2]. Among the total 8 patients discussed herein, delayed fasciotomy occurred in 3. Certainly, close observation and judicious clinical judgment are necessary in every case.
All patients with abdominal trauma should be suspected of having major vascular injury, especially those with compression injury of the lower abdomen. Taking detailed medical history and performing a meticulous physical examination are necessary. In addition, the patient should be carefully observed to detect any changes in the overall condition. It is especially important to consider the most simple and effective methods first, to minimize the risk of death. Ultimately, however, individualized treatment strategies based on each patient's condition are needed and will improve outcomes.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Schoenhagen P, Ghosh S S-Editor: Dou Y L-Editor: Wang TQ E-Editor: Xing YX
| 1. | Tuech JJ, Villapadierna F, Singland JD, Papon X, Pessaux P, Vergos M. Blunt injury to the common iliac artery. Eur J Vasc Endovasc Surg. 2000;20:47-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Blacklay PF, Duggan E, Wood RF. Vascular trauma. Br J Surg. 1987;74:1077-1083. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Ekbom GA, Towne JB, Majewski JT, Woods JH. Intra-abdominal vascular trauma-a need for prompt operation. J Trauma. 1981;21:1040-1044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Feliciano DV, Bitondo CG, Mattox KL, Burch JM, Jordan GL, Beall AC, De Bakey ME. Civilian trauma in the 1980s. A 1-year experience with 456 vascular and cardiac injuries. Ann Surg. 1984;199:717-724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 96] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Tsai FC, Wang CC, Fang JF, Lin PJ, Kao CL, Hsieh HC, Chu JJ, Chen RJ, Chang CH. Isolated common iliac artery occlusion secondary to atherosclerotic plaque rupture from blunt abdominal trauma: case report and review of the literature. J Trauma. 1997;42:133-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Buscaglia LC, Matolo N, Macbeth A. Common iliac artery injury from blunt trauma: case reports. J Trauma. 1989;29:697-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | DeBAKEY ME, SIMEONE FA. Battle injuries of the arteries in World War II; an analysis of 2,471 cases. Ann Surg. 1946;123:534-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 683] [Cited by in RCA: 532] [Article Influence: 35.5] [Reference Citation Analysis (0)] |
| 8. | Sternbergh WC, Conners MS, Ojeda MA, Money SR. Acute bilateral iliac artery occlusion secondary to blunt trauma: successful endovascular treatment. J Vasc Surg. 2003;38:589-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Aerts NR, Lichtenfels E, Erling N. Seat Belt Syndrome and Aortoiliac Lesion: Case Report and Review of the Literature. Eur J Trauma Emerg Surg. 2007;33:198-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Poon H, Patel A, Vijay S, Downing R. Endovascular repair for left common iliac artery occlusion following blunt trauma without associated bony injury: image in vascular surgery. Vasc Endovascular Surg. 2012;46:179-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Jovanovic M, Radojkovic M, Djordjevic P, Rancic D, Jovanovic N, Rancic Z. Recycling and Reinforcing Intimomedial Flap of the Infrarenal Aorta Using Anterior Longitudinal Ligament in Patients With Acute Trauma With Bowel Injuries. Vasc Endovascular Surg. 2017;51:501-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Mogannam AC, Cubas RF, Gutierrez IM, Astudillo JA, Abou-Zamzam AM. Blunt Traumatic Occlusion of the Common Iliac Artery Repaired With Segmental Excision and Internal Iliac Artery Patch Angioplasty. Ann Vasc Surg. 2017;39:284.e1-284.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Lyden SP, Srivastava SD, Waldman DL, Green RM. Common iliac artery dissection after blunt trauma: case report of endovascular repair and literature review. J Trauma. 2001;50:339-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Papazoglou KO, Karkos CD, Kalogirou TE, Giagtzidis IT. Endovascular management of lap belt-related abdominal aortic injury in a 9-year-old child. Ann Vasc Surg. 2015;29:365.e11-365.e15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Beless DJ, Muller DS, Perez H. Aortoiliac occlusion secondary to atherosclerotic plaque rupture as the result of blunt trauma. Ann Emerg Med. 1990;19:922-924. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Frank JL, Reimer BL, Raves JJ. Traumatic iliofemoral arterial injury: an association with high anterior acetabular fractures. J Vasc Surg. 1989;10:198-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 17. | Nitecki S, Karmeli R, Ben-Arieh Y, Schramek A, Torem S. Seatbelt injury to the common iliac artery: report of two cases and review of the literature. J Trauma. 1992;33:935-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Gupta N, Auer A, Troop B. Seat belt-related injury to the common iliac artery: case report and review of the literature. J Trauma. 1998;45:419-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Ko SY, Tan KH, Cheng-Huang CY, Huang MK, Seow VK, Chen CC. Complete common iliac artery transection: an easily misdiagnosed but fatal complication of blunt abdominal injury. Am J Emerg Med. 2007;25:251-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 20. | Feliciano DV, Mattox KL, Graham JM, Bitondo CG. Five-year experience with PTFE grafts in vascular wounds. J Trauma. 1985;25:71-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 143] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 21. | Landreneau RJ, Lewis DM, Snyder WH. Complex iliac arterial trauma: autologous or prosthetic vascular repair? Surgery. 1993;114:9-12. [PubMed] |
| 22. | Shah DM, Leather RP, Corson JD, Karmody AM. Polytetrafluoroethylene grafts in the rapid reconstruction of acute contaminated peripheral vascular injuries. Am J Surg. 1984;148:229-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 57] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 23. | Ouchi T, Kato N, Nakajima K, Higashigawa T, Hashimoto T, Chino S, Sakuma H. Splenic Artery Aneurysm Treated With Endovascular Stent Grafting: A Case Report and Review of Literature. Vasc Endovascular Surg. 2018;52:663-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 24. | Kaya U, Colak A, Becit N, Ceviz M, Kocak H. Endovascular Stent Graft Repair of Localized Acute Aortic Intramural Hematoma: A Case Report and Literature Review. Eurasian J Med. 2017;49:211-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Zebari S, Huang DY, Wilkins CJ, Sidhu PS. Acute Testicular Segmental Infarct Following Endovascular Repair of a Juxta-renal Abdominal Aortic Aneurysm: Case Report and Literature Review. Urology. 2019;126:5-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 26. | Woo EY, Milner R, Brayman KL, Fairman RM. Successful PTA and stenting for acute iliac arterial injury following pancreas transplantation. Am J Transplant. 2003;3:85-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |