Published online Jul 6, 2019. doi: 10.12998/wjcc.v7.i13.1671
Peer-review started: February 15, 2019
First decision: March 8, 2019
Revised: March 15, 2019
Accepted: May 1, 2019
Article in press: May 1, 2019
Published online: July 6, 2019
Processing time: 144 Days and 2.2 Hours
Innominate artery aneurysms (IAAs) are relatively rare. Endovascular therapy has been an alternative to open surgery in some IAA cases, but open repair is still necessary in complicated cases.
We report a 35-year-old female who suffered from Takayasu’s arteritis. The patient did not get regular treatment, and IAA and right common carotid artery aneurysm developed, which complicated with occlusion of the left carotid artery, subclavian artery, and the initial part of the left vertebral artery. The patient also had moderate aortic valve insufficiency. With inflammation being controlled well, the patient received the surgery for arterial aneurysms of innominate and right common carotid arteries and aortic valve insufficiency. The shunts for cerebral blood supply were designed to protect the brain and the surgery was conducted successfully under extracorporeal circulation.
The case illustrates that open surgery may be appropriate for some complicated IAAs, and brain protection is important.
Core tip: This is a very interesting case of Takayasu’s arteritis, which is a relatively rare reason for innominate artery aneurysm. The patient had innominate artery and right carotid artery aneurysms. The patient also suffered from occlusion of the left carotid artery, subclavian artery, and the initial part of the left vertebral artery. The condition of aortic valve insufficiency also increased the difficulty of the surgery.
- Citation: Wang WD, Sun R, Zhou MX, Liu XR, Zheng YH, Chen YX. A complicated case of innominate and right common arterial aneurysms due to Takayasu’s arteritis. World J Clin Cases 2019; 7(13): 1671-1676
- URL: https://www.wjgnet.com/2307-8960/full/v7/i13/1671.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i13.1671
Innominate artery aneurysms (IAAs) are rare and account for only 3% of supra-aortic arterial aneurysms[1]. The complications of IAA include rupture, embolization, and compression of adjacent structures. Surgery may be recommended in IAA patients to prevent the complications[2]. Endovascular therapy has been an alternative to open surgery in some IAA cases[2,3], but open repair is still necessary in complicated cases. We herein report a successful open surgery for a particular patient with IAA due to Takayasu’s arteritis.
Chest distress and hard breath for about 4 mo.
A 35-year-old woman who suffered from chest distress and hard breath for about 4 mo came to our hospital on June 20, 2018. She was diagnosed with Takayasu’s arteritis 10 years ago and did not get regular treatment. She began to take prednisone orally about half a year ago. An ultrasound scan at local hospital revealed a right carotid aneurysm. The patient came to our hospital and computed tomography angi-ography (CTA) revealed that the innominate and right common carotid arteries formed aneurysms with occlusion of multiple contralateral cervical arteries. Echocar-diography revealed moderate aortic valve insufficiency.
Takayasu’s arteritis for 10 years.
A 3 cm × 1 cm pulsatile mass was found on the right side of the neck, and vascular murmurs could be heard. No left carotid or radial pulse was felt. Diastolic murmurs were heard in the aortic valve area.
Routine blood test and parameters of hepatorenal function and coagulation function were within normal ranges. The white blood count was 6.70 × 109/L, red blood cell count was 4.28 × 1012/L, and hemoglobin was 127 g/L. The cTnI was 0.017 μg/L, and NT-proBNP was 830 pg/mL. The inflammation markers were also in normal limits, with ESR being 12 mm/h, and hsCRP being 0.32 mg/L.
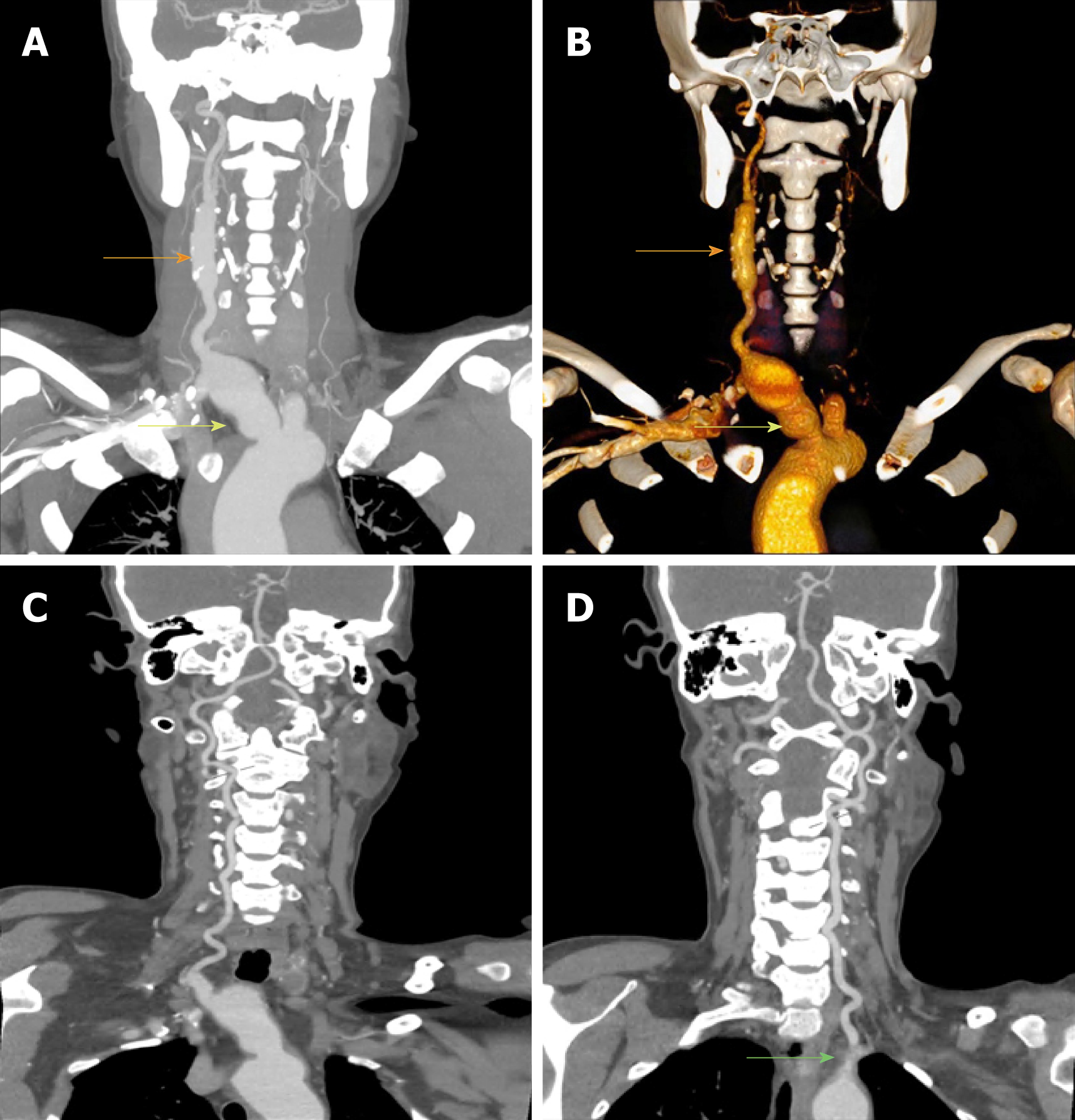
CTA revealed that the innominate and right common carotid arteries formed aneu-rysms (the maximum cross-section diameter was 3.3 cm and 1.6 cm, respectively) (Figure 1). The left common carotid, internal carotid, subclavian artery, and initial part of the left vertebral artery were occlusive. The right vertebral artery displayed well with patency of anterior and posterior communicating arteries.
The patient had innominate and right common carotid artery aneurysms with occlusion of the left common carotid, internal carotid, subclavian, and vertebral arteries. The patient also had aortic valve insufficiency. The etiology was considered as Takayasu’s arteritis.
A multiple disciplinary team (MDT) discussion was performed. The key issues for surgery were considered as below: (1) How to control inflammation during the perioperative period? (2) Should the aortic valve insufficiency be resolved in the same-stage surgery? and (3) The most important question is how to realize cerebral protection?
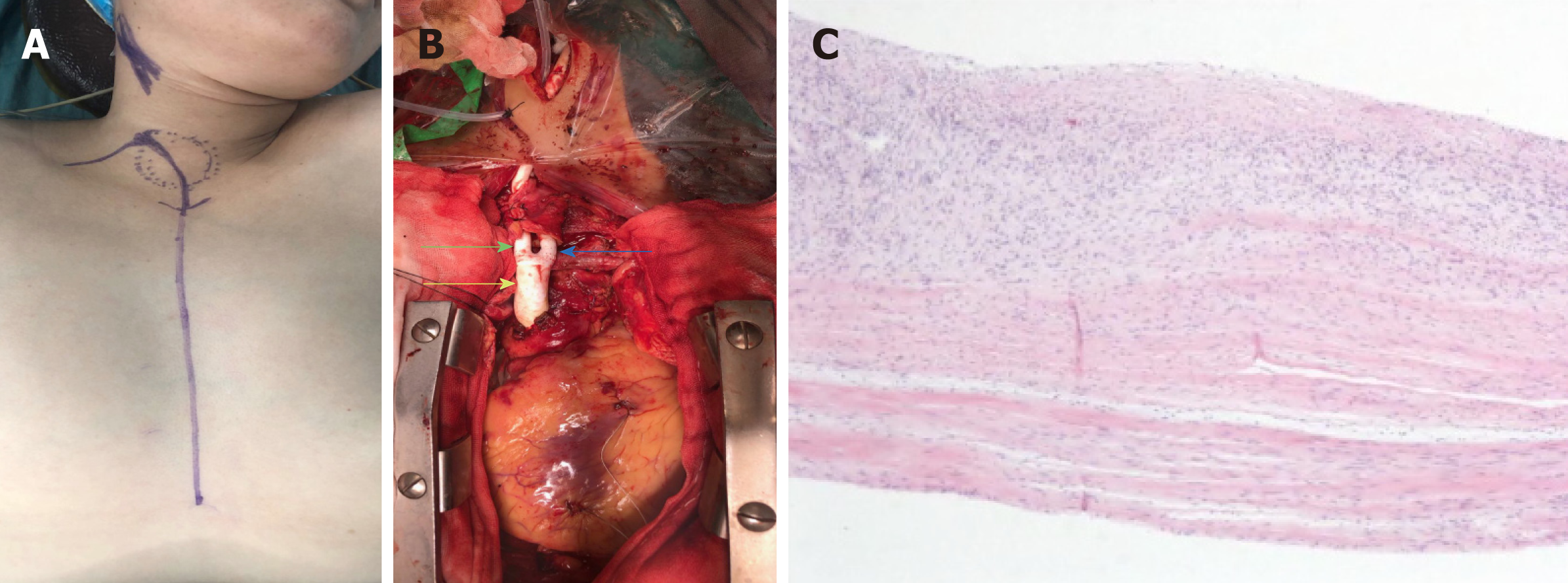
Inflammation was controlled by taking prednisone 10 mg/d orally before operation, and the prednisone was replaced by hydrocortisone on the operation day (50 mg q8h i.v.) and the first postoperative day (100 mg q12h i.v.). The surgery was performed by doctors of Vascular and Cardiac Surgery Department together. Ice-cap was used, and electroencephalogram (EEG) and cerebral oxygen monitoring were performed. Cardiopulmonary bypass was established routinely. Then a Φ 8 mm prosthesis was end-to-side anastomosed with the right axillary artery, and the prosthesis was connected with the outflow tract of an extracorporeal circulation machine. A catheter sheath was placed in the right femoral artery and was also connected with the outflow tract of the extracorporeal circulation machine. Both the two pathways were prepared for aneurysm resection. After performing the aortic valve replacement during cardiac pulmonary bypass, aneurysm resection and vascular reconstruction were conducted. The end of a 14 mm × 7 mm × 7 mm Y-shape artificial vessel was connected with the aortic arch (end-to-side). Then, the root of the innominate artery was blocked with an aorta side wall clamp, and the innominate artery was cut off at the initial part. The broken end of aorta side was sutured. During this stage, the blood supply for the right carotid and vertebral arteries was from the pathway of the right axillary artery. Whereafter, a shunt tube was placed into the right common carotid artery distally to the carotid aneurysm. The shunt tube was connected to the catheter sheath of the femoral artery using a connecting tube. So the shunt to the right carotid artery was established. Then, the carotid artery was cut off at the distal end of the carotid aneurysm. The innominate and carotid arterial aneurysms were excised. The distal end of the common carotid artery was sutured to one 7 mm end of the artificial vessel. The shunt tube was pulled out at the end of anastomosis. Then, cardiopulmonary bypass was stopped and the distal end of the subclavian artery was connected to another 7 mm end of the artificial vessel. The pathways of the right axillary artery and femoral artery were removed. Then, the incisions were sutured with placement of drain tubes. The final pathology showed chronic inflammation of vascular wall with hyaline and mucinous degeneration of both vascular wall and aortic valve (Figure 2).
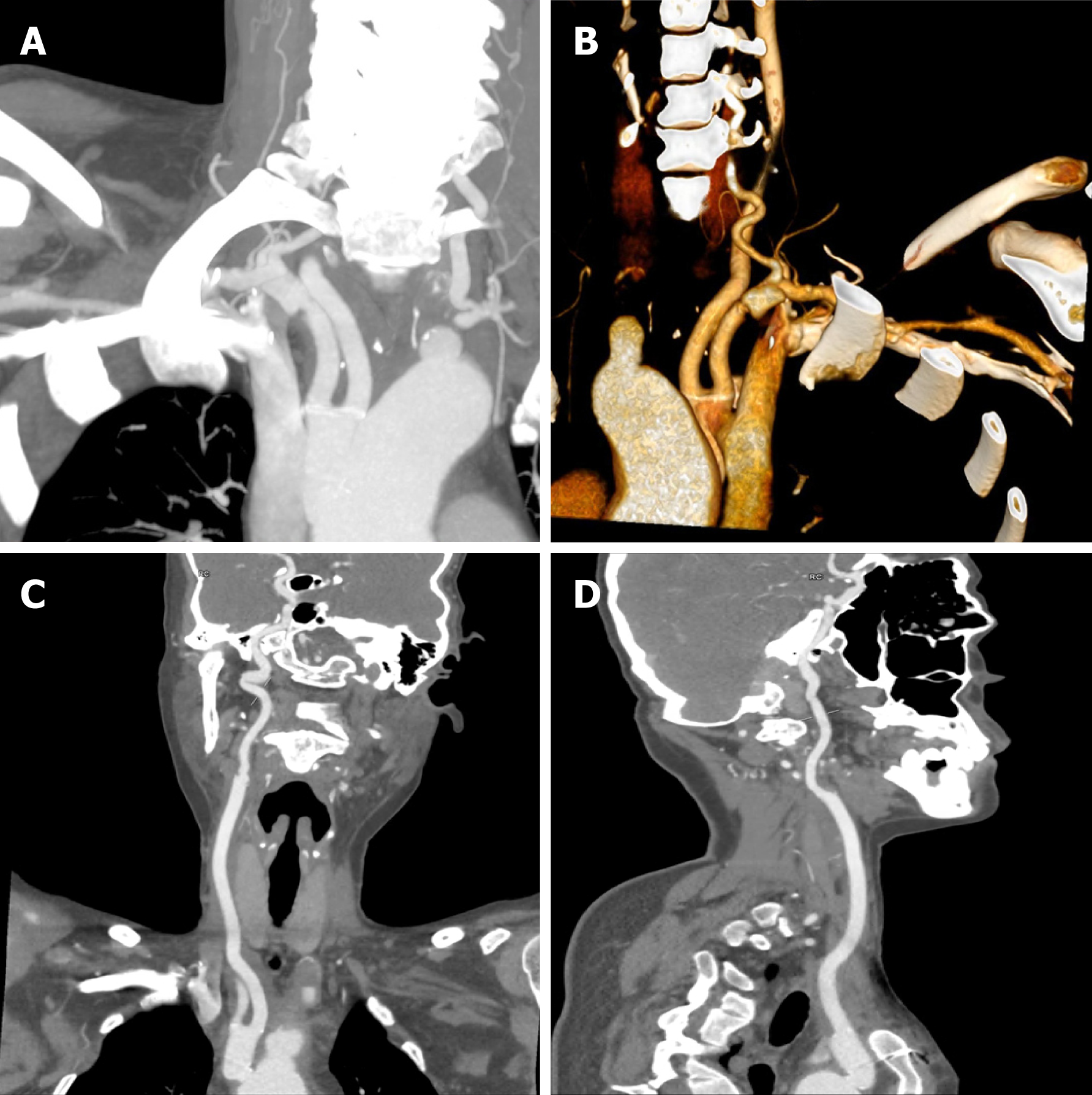
The patient was discharged without complications on the 18th day after operation. The patient had no complaints of dyspnea or chest stufly at one month after discharge from hospital. The CTA revealed patency of artificial innominate and right carotid arteries (Figure 3), and echocardiography presented no relapse of aortic valvular regurgitation. The patient continued treatment of prednisone orally (10 mg daily) and the re-examination of ESR was 12 mm/h.
About 1%-3% of all arterial aneurysms are IAAs[1,4]. IAAs are mainly caused by athero-sclerosis recently, and other causes include infections (syphilis, tuberculosis, etc.), immune diseases (Kawasaki disease, Takayasu’s arteritis, Behçet disease, Marfan syndrome, etc.), angiosarcoma, and trauma[2,5]. Wang et al[3] reviewed the literature and reported that only 8/120 (7.2%) of IAAs resulted from Takayasu’s arteritis. The common clinical manifestations include distal embolization and thrombosis, compression of adjacent structures, and spontaneous rupture[2,6]. The indications for surgery include ruptured and symptomatic aneurysms, and asymptomatic aneurysms with a saccular appearance or a maximum transverse diameter > 3 cm[6].
Kieffer et al[6] divided IAAs into three categories: group A, no involvement of origin of the innominate artery; group B, involvement of origin of the innominate artery but not of the aorta; group C, involvement of both the innominate artery and aorta. And our case should be classified into group B. The different involvement conditions need distinct surgical treatment techniques, including lateral suture of the aorta, patch angioplasty of the aorta, replacement of the ascending aorta, and replacement of the ascending aorta and transverse aortic arch in association with distal elephant trunk prosthesis. Endovascular repair has been a considerable alternative to conventional surgical therapy, which generally needs median sternotomy and even cardiopul-monary bypass. When reviewing the literature, two reports were found to analyze the IAA patients due to Takayasu’s arteritis. Kieffer et al[6] reported 27 IAA patients in 2001, among whom seven were due to Takayasu’s arteritis. Traditional surgical repairs were performed in these patients. The authors mentioned distal bypass graft anastomosis to the right subclavian artery in two patients with extensive right carotid occlusion, and to the right common carotid artery in one with axillosubclavian artery occlusion. Angiletta et al[2] reported a female patient who received stent graft repair for IAA, and the stent was still patent with complete thrombosis of the aneurysmal sac when she came back for reexamination 8 years later.
When considering our patient, it was hard to perform endovascular repair because the patient also had occlusive lesions in the left side. So temporary balloon block of the right side during endovascular therapy was dangerous and might lead to cerebral ischemia. The only way to resolve the problem was to design reasonable temporal shunts. We established two pathways for blood supply to the right carotid and verte-bral arteries successively, and successfully realized brain protection. On the other hand, the patient also had aortic valvular regurgitation which also had indication for treatment, and re-thoracotomy might be much more difficult.
For the etiology of this case is Takayasu’s arteritis, perioperative inflammation control is crucial. Except for emergency conditions, the surgery should be performed until the inflammation is controlled to reduce the risk of complications, including restenosis, thrombosis, anastomotic failure, and pseudoaneurysm formation[2]. The postoperative long-term control of inflammation is also necessary. On the other hand, prompt and regular treatment for Takayasu’s arteritis is important to avoid severe vascular lesions. The patient should receive continuous follow-up to ensure regular anti-inflammatory therapy and to evaluate long-term outcome of the surgery.
In conclusion, we report a rare case of innominate and right common arterial aneur-ysms due to Takayasu’s arteritis which was successfully treated by well-considered surgical strategy. Open surgery may be more appropriate for complicated IAAs such as our case, and brain protection is important during surgery.
Manuscript source: Unsolicited Manuscript
Specialty type: Anesthesiology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kai K S-Editor: Ma YJ L-Editor: Wang TQ E-Editor: Wang J
| 1. | Cury M, Greenberg RK, Morales JP, Mohabbat W, Hernandez AV. Supra-aortic vessels aneurysms: diagnosis and prompt intervention. J Vasc Surg. 2009;49:4-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 44] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Angiletta D, Marinazzo D, Guido G, Fullone M, Pulli R, Regina G. Eight-year follow-up of endovascular repair of a brachiocephalic trunk aneurysm due to Takayasu's arteritis. J Vasc Surg. 2012;56:504-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Wang XL, Guan XL, Jiang WJ, Liu O, Zhang HJ. Innominate artery aneurysm, how to solve it? J Int Med Res. 2017;45:1279-1284. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Chambers CM, Curci JA. Treatment of nonaortic aneurysms in the endograft era: aneurysms of the innominate and subclavian arteries. Semin Vasc Surg. 2005;18:184-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Soylu E, Harling L, Ashrafian H, Anagnostakou V, Tassopoulos D, Charitos C, Kokotsakis J, Athanasiou T. Surgical treatment of innominate artery and aortic aneurysm: a case report and review of the literature. J Cardiothorac Surg. 2013;8:141. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Kieffer E, Chiche L, Koskas F, Bahnini A. Aneurysms of the innominate artery: surgical treatment of 27 patients. J Vasc Surg. 2001;34:222-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 66] [Article Influence: 2.8] [Reference Citation Analysis (0)] |