Published online Jul 6, 2019. doi: 10.12998/wjcc.v7.i13.1634
Peer-review started: January 22, 2019
First decision: March 10, 2019
Revised: May 29, 2019
Accepted: June 10, 2019
Article in press: June 10, 2019
Published online: July 6, 2019
Processing time: 168 Days and 1.6 Hours
Primary hydatid disease in the colon is an extremely rare finding. We performed a systematic review of cases of hydatidosis of the colon published to date.
To systematic review the published papers about hydatidosis of the colon.
Following PRISMA guidelines, we performed an unlimited search for articles on CH in the MEDLINE (PubMed), EMBASE, Cochrane, Latindex and Scielo databases, published in English, Spanish, French, German or Italian between January 1, 1960 and December 15, 2018. The search items were: (Colon) AND [(hydatidosis) OR (hydatid disease) OR (echinococcosis)].
Nine case reports were found [five men, four women, median age 64.55 years (range: 21-81)]. The most frequent clinical manifestation was abdominal pain (8/9) (88.9%). In almost all cases several image studies were carried out, but abdominal computed tomography was the most used (66.7%). Five resections of the colon (62.5%) and three sutures of the fistula between cyst and colon (37.5%) were performed. Four patients did not present post-operative complications, but one died. Postoperative period was recorded for a mean period of 35 months. No recurrences were recorded.
The most frequent symptom was abdominal pain (evidence level 4). Computed tomography was the most frequently used diagnostic imaging technique (evidence level 4). Colectomy was the most appropriate treatment (evidence level 5). All the diagnostic and therapeutic options for hydatid cysts located in colon have a low level of evidence.
Core tip: Hydatidosis of the colon or hydatid cysts causing any clinical problem in colon (fistula, hemorrage or obstruction) is a extremely rare condition. We have performed a systematic review of the literature focusing in epidemiological, diagnostic and therapeutic tips about this topic. We have tried to find explanations about the low incidence of primary hydatidosis of the colon or affecting the colon. No clear explanation about low incidence has been found.
- Citation: Latatu-Córdoba MÁ, Ruiz-Blanco S, Sanchez M, Santiago-Boyero C, Soto-García P, Sun W, Ramia JM. Hydatid cyst of the colon: A systematic review of the literature. World J Clin Cases 2019; 7(13): 1634-1642
- URL: https://www.wjgnet.com/2307-8960/full/v7/i13/1634.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i13.1634
Echinococcal disease is a worldwide parasitic infection caused by the metacestode of genus Echinococcus spp. The infection is commonly caused by E. granulosus[1-3]. According to the World Health Organization, echinococcal disease is endemic in Eastern Europe, Russia, the Middle East, South America and China. The prevalence of infection depends on several factors (low socio-economic status, farming, and uncontrolled and poor hygienic conditions) and varies from 20% to 95%[3]. Human incidence rates in endemic areas reach 50 cases per 100000 persons per year, but this figure represents just a fraction of infected hosts. The revision of public health policies in several countries has substantially reduced the prevalence. Human hydatidosis is an infection that affects primarily liver (65%-75%) and lungs (10%-25%), but other localizations such as peritoneal cavity, spleen, kidneys and brain have also been reported[4].
Within the parasite reproductive cycle, animals such as dogs, foxes and coyotes are definitive hosts and sheep, pigs and other livestock are intermediate hosts. Humans become accidental hosts when eggs are ingested (fecal-oral route). The eggs hatch in the first part of the small intestine to release the oncosphere - the larvae that invade the intestinal mucosa to enter the blood flow. Once they access the portal circulation, they reach the liver (the main affected organ) where most of them are filtered; the remaining larvae continue in the blood flow and reach the lungs (the second most affected organ). They then spread through the blood or lymphatic system to any part of the body where they form what we know as a hydatid cyst.
Primary or secondary hydatidosis of the colon or abdominal hydatid cysts located in other organs that affect the colon is extremely rare[5-13]. This may appear surprising, since the colon can be infected in the oral route or may be involved in patients with disseminated intra-abdominal hydatidosis, liver hydatidosis cysts near the right angle of the colon, or splenic cysts in the left angle; therefore, the number of patients with HC might be expected to be higher than that published. We performed a systematic review of primary hydatidosis of the colon or hydatidosis in other abdominal organs that cause colonic clinical symptoms in an attempt to measure the real incidence of CH and to account for its apparently low frequency.
Following PRISMA guidelines, we performed an unlimited search for articles on CH in the MEDLINE (PubMed), EMBASE, Cochrane, Latindex and Scielo databases, published in English, Spanish, French, German and Italian between January 1, 1960 and December 15, 2018. The search items were: (Colon) AND [(hydatidosis) OR (hydatid disease) OR (echinococcosis)]. The inclusion criteria were any type of article that included patients diagnosed with hydatidosis affecting any location of the colon. Case reports were not excluded.
The selected studies were evaluated, and patients were defined as those with diagnosis of hydatidosis located primarily in the colon or in other organs that cause any colon disease (fistula, obstruction or bleeding). The following data were included, if available: Clinical analytical and intraoperative data, and postoperative course.
The articles were included or rejected on the basis of the predefined criteria and the information obtained from the title and summary. Searches for duplicate series were performed. In case of doubt, the article was read in full. The references of the selected articles were also checked, though no additional articles not included in the initial search were eventually found. The quality of the studies included was assessed according to the levels of evidence of the Oxford Center for Evidence-based Medicine
Sixty-two manuscripts were found, but only eleven were related to our topic. Two reports written in Bulgarian and Czech were excluded. Only nine case reports including nine patients were found that met our search criteria. No further papers were found in the search of the references. The data of the nine patients are summarized in Table 1 to 3.
| Ref. | Sex | Age | Abdominal pain | Nausea and vomiting | Fever | Abdominal exploration | Past medical history | Current medical history |
| Sapkas et al[13], 1972 | Male | 70 | Yes | NA | Yes (38-40 °C) | Spherical mass in left upper quadrant | NA | Splenic hydatid cyst |
| Ortiz et al[12], 1987 | Female | 75 | Yes | NA | Yes (38.0 °C) | Epigastric and right upper-quadrant tenderness | Liver hydatid cyst treated with mebendazol | Hematemesis and substernal pyrosis |
| Puras et al[11], 1989 | Male | 81 | Yes | NA | NA | Plastron in inferior hemiabdomen | Liver hydatid cyst; Intestinal obstruction secondary to intestinal adhesions (peritoneal hydatid cyst discovered but not treated); Left inguinal hernia/Amputation of lower left limb due to ischemia | Chronic constipation. Depositions with mucus in recent months. Last 4 d with melenas and abdominal pain |
| Leviav et al[10], 1996 | Male | 21 | Yes | NA | NA | NA | NA | Abdominal trauma (soccer) |
| Lo Casto et al[9], 1997 | Female | 59 | Yes | NA | Yes (38.5 °C) | A palpable mass found in the left upper quadrant | Dyspepsia | Anaphylactic reaction 10 d previously |
| Astarcioglu et al[8], 2001 | Male | 61 | Yes | Vomiting | Yes | Abdominal distention | Unremarkable | - |
| Fernández Salazar et al[7], 2005 | Female | 73 | Yes | Vomiting | NA | Splenomegaly and hepatomegaly | Liver hydatid cyst; Intestinal obstruction due to an abdominal plastron with two small hydatid cysts in peritoneum | Anorexia and weight loss |
| Teke et al[6], 2008 | Female | 77 | No | NA | No (36.5 °C) | Mild tenderness in the left upper quadrant, with no rebound, guarding, mass or hepatosplenomegaly | Hypertension, Hysterectomy for uterine myoma | Hematochezia |
| Restivo et al[5], 2010 | Male | 64 | Yes | Nausea and vomiting | No | Diffusely tender without guarding and rebound, no palpable masses | Constipation | Abdominal pain, nausea and vomiting |
Clinical data (Table 1): Five patients were men and four women. Median age was 64.55 years (range: 21-81). The most frequent clinical manifestation was abdominal pain (8/9, 88.9%). One case did not report abdominal pain (11.1%). Three patients presented vomiting, one of whom also presented nausea; no information on nausea or vomiting was reported in the rest of the patients. Four patients had fever, two did not, and no data on fever were available for the remaining three. Two patients presented hematochezia (22.2%), one of them associated with hematemesis, and two other cases hyperactive bowel sounds (22.2%). As regards past medical history, three patients had been previously diagnosed with hydatid disease (33.3%): One of them with liver cysts only, and two with liver and peritoneal cysts.
On physical examination, three patients presented abdominal tenderness (33.3%), one hepatomegaly, one abdominal distention, and two a palpable mass in the left upper quadrant (22.2%). No information was reported in the other patients.
The data on radiological studies are presented in Table 2. Abdominal X-ray was performed in five patients (55.6%), abdominal computed tomography (CT) in six (66.7%), ultrasound scan (US) in four (44.4%), colonoscopy in five (55.6%) and contrast studies in four patients (44.4%). In almost all cases several image studies were carried out; in one case, no imaging studies were performed. Calcifications of the cyst wall were described in four cases, aerial content in five, and cyst liquid in two. Two patients presented dilation of the colon. A fistula between colon and cyst was observed in the radiological studies of four patients. Analytical data are shown in Table 2. Four patients had leukocytosis, one of whom presented eosinophilia and another left deviation. However, no information of leukocyte levels was identified in four cases. Hydatid serology was performed in only two cases and was positive in both.
| Ref. | Leukocytosis | Hydatid Serology | Abdominal X-ray | Ultrasound | CT | Contrast studies | Colonoscopy |
| Sapkas et al[13], 1972 | NA | NA | Calcified splenic cyst | NA | NA | Adhesion cyst-left colon | NA |
| Ortiz et al[12], 1987 | Shift to the left | NA | Elevated right hemidiaphragm | NA | Gas-filled cavity in the right lobe of the liver | Sliding hiatal hernia and fistula extending from the colon to the liver cavity | NA |
| Puras et al[11], 1989 | No (3700/mm3) | Positive | No significant alterations | Intrabdominal cavity of 10.3 × 10.7 cm with cystic appearance | ND | Presence of fistula allows the filling of the hydatid cyst | Sigmoid fistula (3 cm) with opening to polycystic cavity at 23 cm from anal margin |
| Leviav et al[10], 1996 | NA | NA | NA | NA | NA | NA | - |
| Lo Casto et al[9], 1997 | Eosinophilia (20%) | NA | NA | Large oval mass with well-defined wall and a complex echo pattern. Hyperechoic tracts inside the wall with acoustic shadowing | Mass originated from the liver extending from left hemidiaphragm to sacro-iliac joint, situated between left transverse and descending segments of colon, partially calcified and with mixed density content (liquid with bubbles and air-fluid level) | NA | NA |
| Astarcioglu et al[8], 2001 | Yes (21000 /mm3) | Positive | Dilated right and transverse colon; Left colonic obstruction | Dilated colonic segments and ascites | NA | NA | NA |
| Fernández Salazar et al[7], 2005 | NA | NA | Large lobulated calcification of liver cyst with aerial content | Calcified cystic lesion (8.5 cm) in right hepatic lobe | Right hepatic lobe hypertrophy, 8 cm cystic cavity with calcified wall with intra and perilesional air | Hepatic cystic cavity filled with contrast in communication with the colon at the level of the hepatic angle | In hepatic angle, a blackish hemispherical stone structure inside which it was possible to access through a notch |
| Teke et al[6], 2008 | Yes (18600/mm3) | NA | NA | NA | Ruptured cystic lesion (5.4 cm × 5.6 cm) in the inferior pole of the spleen. Hyperdense material filling the left colon and multiple cystic lesions in the abdominopelvic region. Gas in the cystic cavity | Extravasation of contrast at the level of splenic hilus and colon’s splenic flexure | Failed to show the source of the bleeding due to active major bleeding |
| Restivo et al[5], 2010 | NA | NA | NA | NA | Colonic distention caused by a 6-cm intraluminal ovoidal cystic mass with peripheral calcification in the sigmoid colon | NA | The cyst was stuck to the mucosa (sigma) |
Intraoperative and postoperative finding are included in Table 3. One patient refused surgery. The intraoperative findings in the remaining eight demonstrated that seven had a fistula between the hydatid cyst and the colon, located in liver (4), spleen (2) and peritoneum. The last patient had a sigmoid obstruction due to several peritoneal cysts located in mesosigma. The fistulized cysts were found in several locations: in the left colon in four patients (a splenic hydatid cyst fistulizing the left colon in two, a ruptured cyst in splenic flexure leading to peritonitis in one, and a hydatid cyst in the left hepatic lobe, communicating with the left colon, in the other); three patients presented a cyst in the right colon (two of them communicating with the right-hepatic lobe and the other entirely in the colonic lumen); one patient had two peritoneal cysts (the larger one fistulized to the colon and the other isolated).
| Ref. | Intraoperative findings | Surgical procedure | Postoperative period morbidity | Pathology | Postoperative albendazole | Follow-up |
| Sapkas et al[13], 1972 | Giant splenic cyst. Communication splenic cyst to colon | Left colectomy with splenectomy (total cystectomy). Colo-colonic terminal anastomosis | 2nd d: Low blood pressure, tachycardia, cyanosis in limbs, death | Isolated mesosigmoidal hydatid cyst | NA | Exitus on second postoperative day |
| Ortiz et al[12], 1987 | Liver cyst. Communication liver cyst to colon | Excision of 5 cm of the colon wall surrounding the fistulous hole and closure of the colonic defect | NA | Calcified cystic lesion in right hepatic lobe with colonic fistula | NA | NA |
| Puras et al[11], 1989 | Two peritoneal cysts of 6 and 10 cm. The larger one fistulized to colon | Total cystopericystectomies and sigmoidectomy with terminal anastomosis | Evisceration with wound closure surgery | Hydatid cyst | NA | NA |
| Leviav et al[10], 1996 | Ruptured cyst in splenic flexure of colon with peritonitis | Resection of splenic flexure plus proximal colostomy. Partial cystectomy of liver cysts | First week: Fever (39 ºC). Subphrenic abscess | Splenic hydatid cyst invading the colon's splenic flexure | NA | No relapse. Followed-up during 12 yr |
| Lo Casto et al[9], 1997 | Hydatid cyst originating from left lobe of the liver fistulized to the left colon | Partial cystectomy and suture of the colonic fistula | NA | Ruptured cyst in splenic flexure of colon with peritonitis | High-dose albendazole (6 mo) | No more surgeries required |
| Astarcioglu et al[8], 2001 | Multiple obstructing hydatid cysts in the colon serosal tissue and mesosigmoid (1.5 - 6 cm ø) | Hartmann’s procedure with 15 cm of resected colonic segment | Uneventful | Peritoneal hydatid cysts fistulized to sigmoidal colon | 200 mg/d oral albendazole | Free of disease 4 mo |
| Fernández Salazar et al[7], 2005 | NA | Refused surgical treatment | NA | Calcified splenic cyst fistulizing left colon | Antiparasitic treatment but not specified | Good evolution 6 months after discharge |
| Teke et al[6], 2008 | Disseminated abdominopelvic hydatid cysts, in the inferior pole of the spleen, and invading the colon's splenic flexure. Fistula between splenic hydatid cyst and colon's splenic flexure, (1 cm) | En-bloc excision of the spleen and splenic flexure of the colon | Uneventful | Hydatid cyst communicating with colon through a fistula | Three 28-d cycles of albendazole therapy | The patient was discharged on the seventh postoperatived |
| Restivo et al[5], 2010 | Large fistula between the hepatic flexure and the liver | Partial cystectomy + suture colon | NA | Hydatid cyst in the right lobe of the liver fistulized in the right colon | NA | At 15-month follow up the patient was well and CT scan and colonoscopy showed a closure of the hepatic-colonic fistula |
Several surgical procedures were performed: Left colectomy with splenectomy and colo-colonic terminal anastomosis (1), resection of five centimeters of the colon wall surrounding the fistulous hole and suture of colonic wall (1), total cystoperi-cystectomies and sigmoidectomy with terminal colon anastomosis (1), resection of splenic flexure plus proximal colostomy (1), partial cystectomy and suture of the colonic fistula (1), Hartmann's procedure with 15 cm of resected colonic segment (1), and en bloc excision of the spleen and splenic flexure of the colon (1) and partial cystectomy + colon suture (1). In summary, there were five resections of the colon and three sutures of the fistula between cysts and colon.
Four patients did not present postoperative complications. One presented fever (39 ºC) and a subphrenic abscess and another presented an evisceration that was repaired surgically performing wound closure alone. One of the patients had low blood pressure, tachycardia and cyanosis in limbs, leading to death on post-operative day 2. No data regarding postoperative outcome were recorded in two cases. In five cases follow-up after the postoperative period was recorded, for a mean period of 35 mo (range: 4-144 mo), and there were no recurrences.
In today’s globalized world, hydatidosis, a disease caused in most cases by Echinococcus granulosus, should be considered both in areas that are endemic and in those that are not. Special attention should be paid to places where contact between definitive hosts and humans are in closer contact: Eastern Europe, Russia, the Middle East, South America and China[3]. The location of cysts in the colon (CH) is very infrequent, and very few cases have been reported.
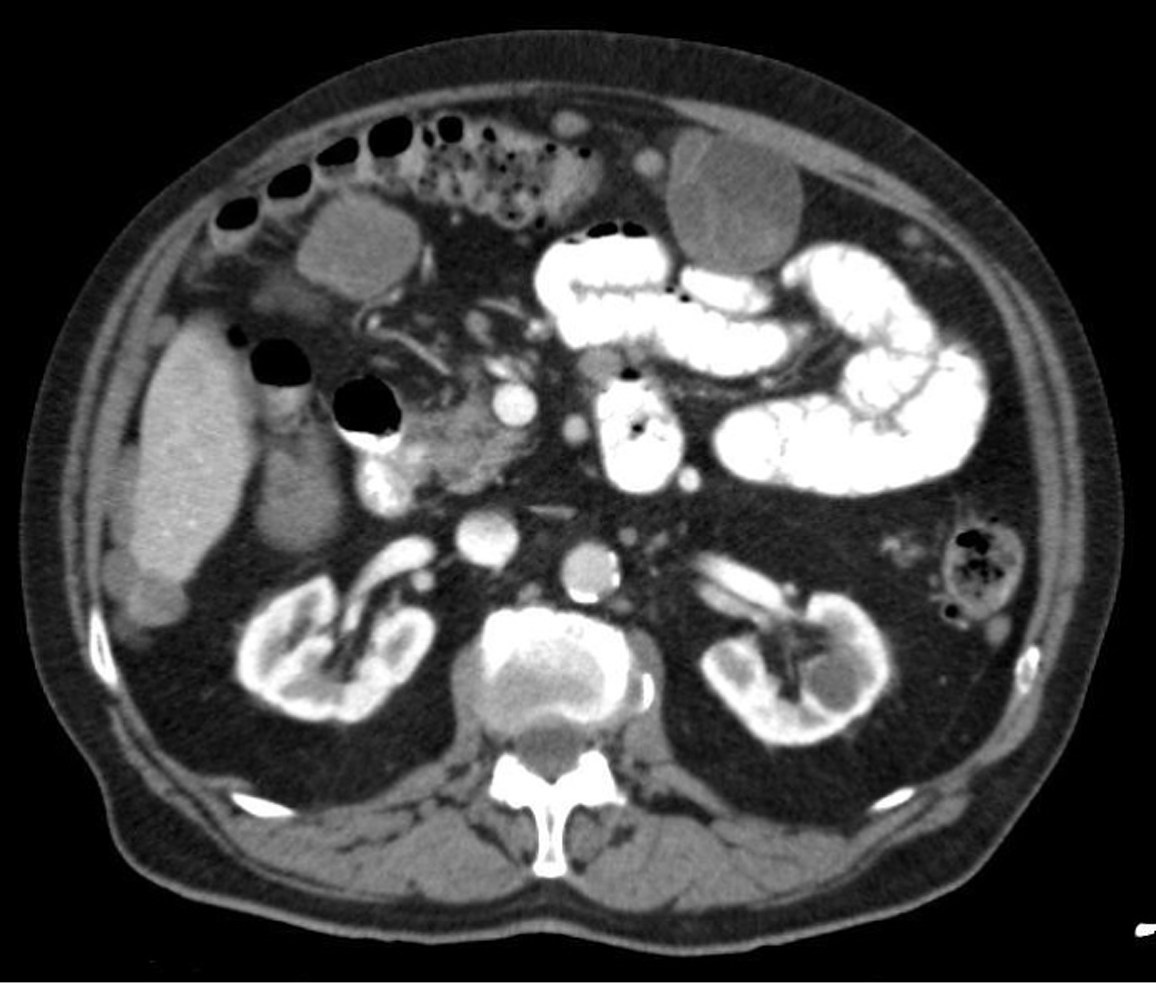
One of our objectives was to account for the low incidence of CH, especially after our PRISMA search yielded only nine published cases. No explanations of this low incidence are available in the literature. The colon is a long organ located near the liver and spleen, and so hydatic cysts located in these organs (especially liver) may invade or erode the colon causing obstruction or fistula. Furthermore, patients with abdominal hydatidosis due to a ruptured cyst, or who present several cysts in the abdominal cavity, may develop CH. Primary CH seems to be exceptional but we do not have any real explanation for its development (as we do for cerebral or spinal hydatidosis); we found only one case in our search. As for the low rates of secondary CH or the involvement of the colon due to cysts in other organs, there are two possible explanations: first, the soft wall of the colon may allow the cyst to push through without eroding, causing very few real fistulas (Figure 1); or second, fistulas may be more frequent than we really think, but are asymptomatic. So, the cyst is emptied through a fistula between the cyst and colon with no or few symptoms. We stress that these are only theories without any support at present.
With regard to the different routes of arrival of the hydatid cyst in the colon, in our nine cases the cyst emerged through a hepatocolonic fistula in 44.4% and through a splenocolonic fistula in 33.3%; there was one case of fistula to the colon in which the initial location of the cyst was the peritoneal cavity, and a single case of an isolated colonic hydatid cyst. The main symptom of CH was abdominal pain in 88.9% of cases, and 44.4% presented fever. To establish the diagnosis of hydatidosis, a combination of tests was performed including abdominal X-ray (55.6%), abdominal computed tomography (66.7%), ultrasound scan (44.4%), endoscopy (55.6%) and contrast studies (44.4%) (Table 2).
The main purpose of this study was to examine the clinical, diagnostic and therap-eutic aspects of hydatid cysts located in the colon. CT seems to be the best diagnostic tool because of the location of the cysts and complications, the possibility of diagnosing fistula between the cyst and the colon, and the possibility of staging other organs in search of more cysts. A wide variety of surgical procedures were used in the eight cases, and so few firm conclusions can be drawn. Resection of the colon or closure of the fistula are the two techniques performed, but because of the small number of cases we cannot conclude which one is better. An open approach by laparotomy is the usual management of this infrequent clinical situation; in any case, the surgeon chooses the technique in the light of the intraoperative findings.
Three main conclusions can be drawn from this study: (1) The most consistent clinical finding is abdominal pain with a medium-low level of evidence (evidence level 4); (2) The most useful diagnostic method is computed tomography, with a medium-low level of evidence (evidence level 4); and (3) The most recommended treatment is colectomy by laparotomy (evidence level 5). The main obstacle to a detailed and evidence-based description of this condition is the lack of clinical cases in the literature. Further research is now needed in order to draw more significant inferences.
No previous systematic reviews about hydatidosis of the colon exist. Very few papers devoted to this topic has been published.
We try to resume previous literature in order to clarify incidence, diagnostic procedures and management of hydatidosis of the colon.
The objectives were not reached. Only few case reports are published so no evidence based medicine could be reached.
We perform a systematic review of the literature following PRISMA guidelines.
No real data about incidence. Abdominal pain is the most common symptom. CT is the best diagnostic tool. Colectomy or suture of the fistula are the surgical procedures usually performed.
No evidence based medicine data about the topic was obtained. No clear data about if there is a low incidence of hydatidosis of the colon or a huge number of undiagnosed cases because they are asymptomatic. We suggest that low incidence perhaps occur due to the soft wall of the colon could be pushed without causing clinical symptoms. Resuming the previous literature let readers know some data about previous cases and their management.
Only prospective multicentre studies made in endemic areas could let us know more about this unfrequent topic.
Manuscript source: Invited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: Spain
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Shahriari B, Giorgio A S-Editor: Dou Y L-Editor: A E-Editor: Liu JH
| 1. | Eckert J, Conraths FJ, Tackmann K. Echinococcosis: an emerging or re-emerging zoonosis? Int J Parasitol. 2000;30:1283-1294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 242] [Cited by in RCA: 243] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 2. | Thompson RC, McManus DP. Towards a taxonomic revision of the genus Echinococcus. Trends Parasitol. 2002;18:452-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 321] [Cited by in RCA: 328] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 3. | Brunetti E, Kern P, Vuitton DA, Writing Panel for the WHO-IWGE. Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Trop. 2010;114:1-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1108] [Cited by in RCA: 1330] [Article Influence: 88.7] [Reference Citation Analysis (0)] |
| 4. | Mushtaque M, Mir MF, Malik AA, Arif SH, Khanday SA, Dar RA. Atypical localizations of hydatid disease: experience from a single institute. Niger J Surg. 2012;18:2-7. [PubMed] |
| 5. | Restivo A, Zorcolo L, D'Alia G, Cabras M, Casula G. Colonic obstruction caused by calcified hepatic hydatid cyst migrated into the left colon. Endoscopy. 2010;42 Suppl 2:E169-E170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Teke Z, Yagci AB, Atalay AO, Kabay B. Splenic hydatid cyst perforating into the colon manifesting as acute massive lower gastrointestinal bleeding: an unusual presentation of disseminated abdominal echinococcosis. Singapore Med J. 2008;49:e113-e116. [PubMed] |
| 7. | Fernández Salazar L, Matas Gómez V, Calabia del Campo J, Abril Vega C, Bombín Mínguez M. [Hydatidic cyst fistulized to colon]. Rev Esp Enferm Dig. 2005;97:673-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Astarcioglu H, Koçdor MA, Topalak O, Terzi C, Sökmen S, Ozer E. Isolated mesosigmoidal hydatid cyst as an unusual cause of colonic obstruction: report of a case. Surg Today. 2001;31:920-922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Lo Casto A, Salerno S, Grisanti M, Mastrandrea G. Hydatid cyst of the liver communicating with the left colon. Br J Radiol. 1997;70:650-651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Leviav S, Weissberg D. Traumatic rupture of hydatid cysts. Can J Surg. 1996;39:293-296. [PubMed] |
| 11. | Puras A, Fernández L, Gómez A, Roig J, Rodríguez S, Campos A. [Peritoneal hydatidosis with fistulization into the sigmoid colon]. Rev Esp Enferm Apar Dig. 1989;75:403-405. [PubMed] |
| 12. | Ortiz H, Carmona JA, Perez-Cabañas I. Colohepatic fistula due to hydatid disease. Report of a case. Dis Colon Rectum. 1988;31:546-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Sapkas A, Tierris E. [Spectacular complication of a gigantic hydatid cyst of the spleen. Rupture into the colon]. J Chir (Paris). 1972;103:283-286. [PubMed] |