Published online May 26, 2019. doi: 10.12998/wjcc.v7.i10.1230
Peer-review started: January 29, 2019
First decision: February 21, 2019
Revised: March 14, 2019
Accepted: May 10, 2019
Article in press: May 11, 2019
Published online: May 26, 2019
Processing time: 117 Days and 20 Hours
It is rare to find fish bones completely embedded in the wall of the esophagus with endoscopic findings similar to those of submucosal tumors. Most of the patients had the foreign body removed by thoracotomy or thoracoscopy in the past, which resulted in great trauma.
We report a 58-year-old woman who experienced dysphagia for 6 d after eating fish. Cervical computed tomography (CT) and endoscopic ultrasonography (EUS) indicated a fish bone completely embedded in the wall of the esophagus with endoscopic findings similar to those of submucosal tumors. The results of CT reconstruction and EUS suggested that the fish bone was parallel to the longitudinal axis of the esophagus. We performed a longitudinal mucosal incision from the highest point of the uplift by using an Olympus dual knife to find the fish bone. Unfortunately, no fish bone was found, so we extended the incision and endoscopic submucosal dissection (ESD) technique was used to detect and remove the fish bone entirety.
The extraction of fish bone via ESD immediately after the injection of methylene blue into the submucous membrane under EUS guidance to obtain accurate localization of the foreign body may be the best treatment for such patients.
Core tip: It is rare to find the fish bone completely embedded in the wall of the esophagus with endoscopic findings similar to those of submucosal tumors. We report a fish bone that is fully embedded and migrated through the esophageal wall. During the operation, it was found that the fish bone was not directly below the highest point of the mass protuberance. Therefore, it is suggested that submucous injection of methylene blue under endoscopic ultrasonographic guidance can be used to locate the foreign body accurately and reduce the injury of treatment.
- Citation: Wang XM, Yu S, Chen X. Successful endoscopic extraction of a proximal esophageal foreign body following accurate localization using endoscopic ultrasound: A case report. World J Clin Cases 2019; 7(10): 1230-1233
- URL: https://www.wjgnet.com/2307-8960/full/v7/i10/1230.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i10.1230
Fish bones are one of the most common foreign bodies found in the digestive tract. Esophageal foreign bodies are mostly embedded in the narrow part of the esophagus. If not treated in time, sharp foreign bodies may puncture the esophagus and cause serious complications. Patients may have symptoms of odynophagia, dysphagia, hemoptysis, fever, chest pain, and other discomfort. Gastroscopy, computed tomography (CT), X-ray, and other examinations can reveal esophageal foreign bodies. Foreign bodies can be moved by esophageal peristalsis, swallowing food, and normal pleural pressure. A fish bone completely embedded into the esophageal wall which results in a submucosal mass is rare. Therefore, for patients who feel uncom-fortable after eating fish and endoscopic examination suggests a submucosal bulge, the possibility of a fish bone granuloma should be considered. It has been reported in the past that fish bones were often removed from the esophageal wall by thoracoscopy. In this case, we chose endoscopic submucosal dissection (ESD) to remove a fish bone, which was less invasive.
Dysphagia for 6 d.
A 58-year-old woman who experienced dysphagia for 6 d after eating fish was admitted to a local hospital. Endoscopic indication of mucosal damage at the entrance of the pharynx and esophagus was observed, but no fish bone was found in the stomach or esophagus. The patient received anti-inflammatory treatment, but the dysphagia continued without fever, vomiting, or hematemesis. Then the patient presented to our hospital.
The patient denied history of hypertension, diabetes mellitus, viral hepatitis, or tuberculosis. She had no known drug or food allergies. She also denied history of operation, trauma, or blood transfusion.
The patient denied history of drinking and smoking or any family history.
Her temperature was 36.6 °C, heart rate was 61 beats/min with normal rhythm, respiratory rate was 20 breaths/min, and blood pressure was 120/70 mmHg. She had facies dolorosa, but the color of whole body skin and mucous membrane was normal. Rales were not heard in bilateral lungs. No extra or abnormal heart sound, murmurs, or pericardium friction sound was noted. The abdomen was flat and soft, and there was no marked pitting edema in lower extremities.
Routine blood, urine, stool, coagulation, and blood biochemistry tests were all normal.
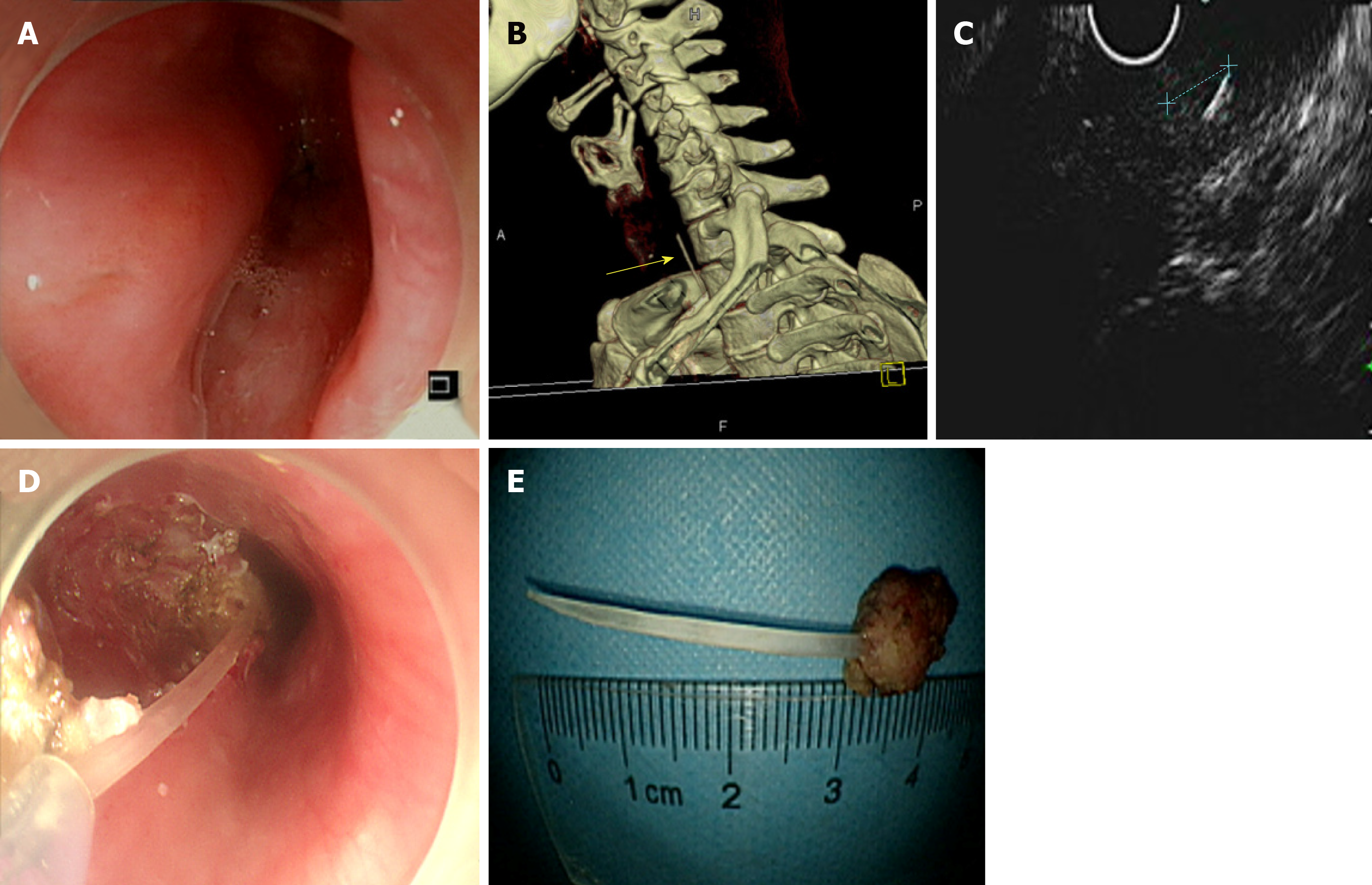
Gastroscopic examination suggested that the upper esophageal segment exhibited a strip-shaped submucous bulge of approximately 8 mm × 40 mm (Figure 1A). CT suggested that the upper esophageal segment contained a high-density band in the right wall, with a diameter of approximately 35 mm (Figure 1B). Endoscopic ultrasonography (EUS) revealed that the upper submucosa of the esophagus exhibited a striped hyperechoic mass, with a rear weak echo, and the muscularis propria was involved (Figure 1C).
A foreign body embed in the submucosa of the upper esophageal wall.
The results of CT reconstruction and EUS suggested that the fish bone was parallel to the longitudinal axis of the esophagus. Considering the age of patient and surgical operation may make much injury, we chose minimally invasive surgery performed by endoscopy to remove the fish bone. We performed a longitudinal mucosal incision from the highest point of the uplift by using an Olympus dual knife to find the fish bone. We did not find the fish bone in a longitudinal incision longer than 50 mm, and we therefore used ESD to remove the entire lump in the mucous membrane. However, no fish bone was found despite the small amount of mucosal tissue that remained. We continued to extend the incision in the anal direction, and found a fish bone embedded in the submucous layer when the incision length reached 70 mm. This location suggested that the fish bone had migrated into the submucous layer of the esophageal wall. We used a snare to slowly extract the fish bone out of the patient’s mouth (Figure 1D and E). The wound was sutured using a Nanjing mi-nimally invasive soft tissue clamp.
The patient was treated with antibiotics for 3 d. She was discharged from the hospital without complaints of fever, chest pain, hematemesis, or melaena.
Fish bones are one of the most common foreign bodies found in the digestive tract, but it is rare to find fish bones completely embedded in the wall of the esophagus with endoscopic findings similar to those of submucosal tumors. Therefore, if the patient is uncomfortable after eating fish, and endoscopic examination suggests submucous bulging, a fish bone granuloma should be suspected. The fish bone was not located directly below the bulging mass in the present case but had migrated into the esophageal wall. It is very important to locate the fish bone position accurately to reduce the size of the incision and wound. Cao et al[1] reported that methylene blue injection into the submucous layer labeled the foreign body position under the guidance of an ultrasound endoscope, and a thoracoscope was used to remove the fish bone. Therefore, we suggest the extraction of fish bone via ESD immediately after the injection of methylene blue into the submucous membrane under ultra-sonographic guidance to obtain accurate localization of the foreign body and thereby reduce the wound size, bleeding, and perforation in endoscopic surgery and avoid additional surgery. This approach may be a better method to treat this condition.
The extraction of fish bone via ESD immediately after the injection of methylene blue into the submucous membrane under ultrasonographic guidance to obtain accurate localization of the foreign body may be the best way for such patients. It can help us to reduce the wound size, bleeding, and perforation in endoscopic surgery and avoid additional surgery.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Lazăr DC, Viswanath YKS S-Editor: Ji FF L-Editor: Wang TQ E-Editor: Wu YXJ
| 1. | Cao L, Chen N, Chen Y, Zhang M, Guo Q, Chen Q, Cheng B. Foreign body embedded in the lower esophageal wall located by endoscopic ultrasonography: A case report. Medicine (Baltimore). 2018;97:e11275. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |