Published online May 26, 2019. doi: 10.12998/wjcc.v7.i10.1169
Peer-review started: January 4, 2019
First decision: March 10, 2019
Revised: March 16, 2019
Accepted: March 26, 2019
Article in press: March 26, 2019
Published online: May 26, 2019
Processing time: 142 Days and 21.7 Hours
Renal duplication is a common deformity of the urinary system, with an incidence of approximately 1/125 in children. Symptomatic patients with hydronephrosis, vesicoureteral reflux, or incontinence may require surgical interventions. Laparoscopy and retroperitoneoscopy are the two main accesses for partial nephrectomy.
A 9-year-old child was admitted to the hospital for hydronephrosis of the left kidney. Ultrasonography showed that the left kidney was larger, approximately 12.6 cm × 6.3 cm × 5.5 cm in size, with visible separation of the pelvis and an obviously separated lower portion. The upper segment of the left ureter was dilated (approximately 2.6 cm in width), and no significant dilation was observed in the middle and upper segments. The right kidney and ureter were normal. Primary diagnosis was left renal duplication malformation and hydronephrosis. Retroperitoneal laparoscopic nephrectomy and ureterectomy were performed. Intraoperative exploration revealed a dilated pelvis and thin renal parenchyma at the lower pole of the left kidney. The upper left kidney was smaller than normal, and the pelvis and ureter were larger than normal. The renal artery was blocked for 40 min. A hemolock was used to clamp down the kidney ureter, and a drainage tube was retained in the retroperitoneal cavity. The operation was uneventful, and the estimated amount of blood loss was 100 mL. Total abdominal drainage amount was 116 mL. The drainage tube was removed on postoperative day (POD) 3 and the patient was discharged on POD6. The pathological diagnosis confirmed the atrophy of the renal parenchyma, the dilation of the renal pelvis, hydronephrosis, and ureteral cystic dilation.
The retroperitoneoscopic approach for partial nephrectomy is feasible and effective in selective pediatric patients with a duplex kidney.
Core tip: Duplex kidney is a common congenital malformation of the urinary system in chil-dren, and most symptomatic patients should opt for surgical management. However, there is still some controversy on the applications of the translaparoscopic approach and retrolaparoscopic approach. We will discuss the advantages and disadvantages of both approaches in this case. These contents provide a basis for future research.
- Citation: Chen DX, Wang ZH, Wang SJ, Zhu YY, Li N, Wang XQ. Retroperitoneoscopic approach for partial nephrectomy in children with duplex kidney: A case report. World J Clin Cases 2019; 7(10): 1169-1176
- URL: https://www.wjgnet.com/2307-8960/full/v7/i10/1169.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i10.1169
Duplex kidney is a common congenital malformation of the urinary system in children, with an incidence of 1/125 individuals. More girls are afflicted with the disorder than boys, and the unilateral incidence of the disorder is higher than the bilateral incidence[1]. The main clinical manifestations are urinary tract infection, urinary incontinence, dysuria, and the presence of an abdominal mass. In addition to having well-developed kidneys that require no treatment, most symptomatic patients should opt for surgical management.
At present, laparoscopic nephrectomy is a mainstream choice in clinical practice. However, there is still some controversy on the applications of the translaparoscopic approach and retrolaparoscopic approach[2-4]. The laparoscopic approach can provide large operation space, and is more suitable for infants. However, complications such as urinary leakage, intestinal adhesion, and intestinal obstruction may occur after operation due to the dissection of abdominal organs and abdominal organs. The retroperitoneal laparoscopic approach is more direct, with less interference to other organs, postoperative urine leakage and bleeding or hematoma confined to the peritoneum, less stimulation, but has a steep learning curve[5].
Due to the lack of experience among surgeons in aspects of the retroperitoneal anatomy and the long operation time, the retroperitoneal laparoscopic technique has not been widely applied among pediatric surgeons[6]. Herein, we report our exper-ience with a retroperitoneal laparoscopic surgery for duplex kidney.
A 9-year-old boy was admitted to the hospital with left-sided hydronephrosis for one week.
Due to abdominal pain, the patient underwent an ultrasonic examination in the out-patient department and was diagnosed as having "left hydronephrosis". It was suspected that the left side had the indication of a renal malformation. He was admitted to the hospital with "left hydronephrosis".
The patient exhibited abdominal flatness, a soft abdomen, normal bowel sounds, no varicose veins in the abdominal wall, no tenderness, no rebound pain, no abdominal masses, and slight percussion pain in the kidney.
The following characteristics were observed via an ultrasound (abdominal) exam-ination: The left kidney was enlarged (with a size of approximately 12.6 cm × 6.3 cm × 5.5 cm), the cortex was thin (with a thickness of approximately 1.0 cm), the pelvis was visibly separated, the lower part of the pelvis was obvious and separated within a range of approximately 7.8 cm × 5.9 cm × 5.4 cm, and the upper part of the pelvis was separated, both before and after treatment, with a diameter of approximately 2.2 cm. The size and morphology of the right kidney were normal, with a uniform cortical echo, a clear renal internal structure, no separation of the renal pelvis, and no clear occupying lesions. The upper segment of the left ureter was dilated (approximately 2.6 cm wide), and no significant dilation was observed in the middle and lower segments. No dilation was observed in the right ureter. Bladder filling was optimal, the wall was not thick, but smooth, and there was no abnormal echo inside of the kidney.
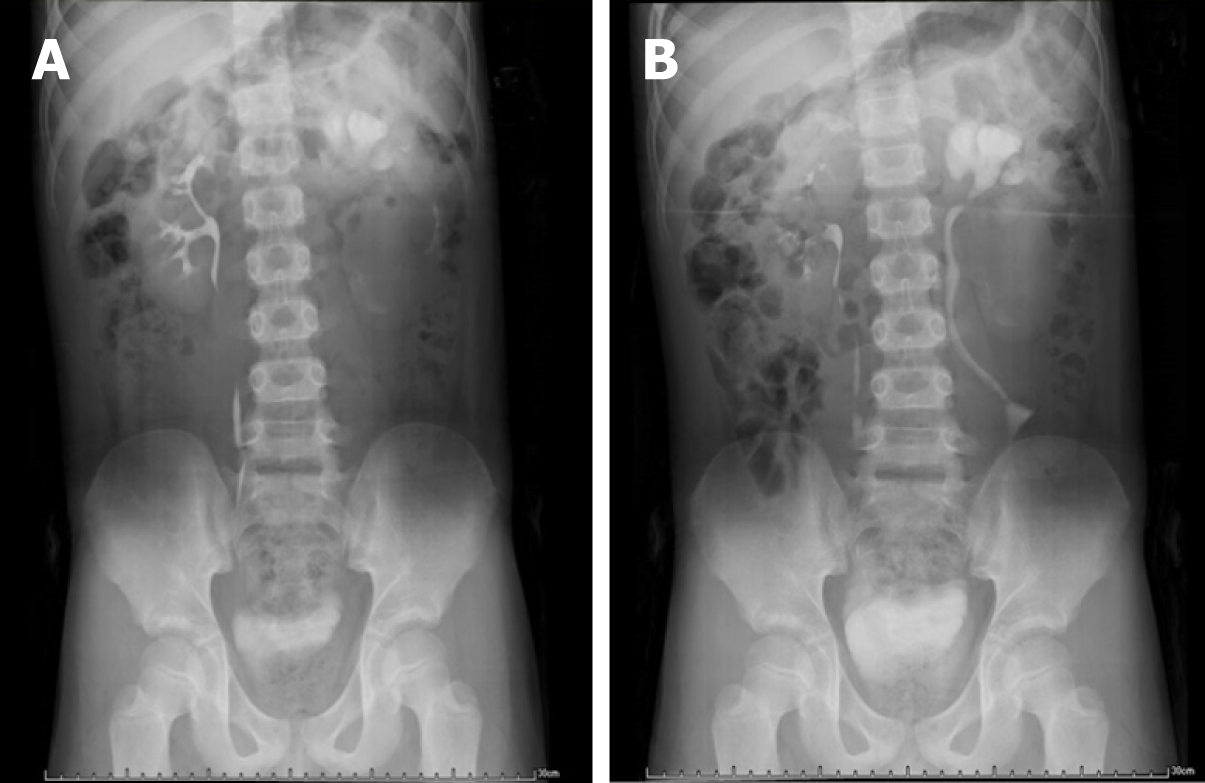
The following characteristics were observed via an intravenous pyelography (Figure 1): No positive stones were observed in the abnormalities of the ureters and the bladder on both sides. After the injection of the contrast agent, bilateral ureters and bilateral kidneys were developed. The left renal pelvis was dilated, and the calyx was blunt. The right renal pelvis was not enlarged, no filling defect was observed, and the calyx cup was sharp. The bilateral ureters showed no stenosis or dilations. The bladder was filled, but no defect was found.
The following characteristics were observed via a nuclear medicine examination (ECT): The excretion from the left kidney was not smooth, and the glomerular filtration rate (GFR) was slightly reduced. The right kidney function was generally normal. The following results were obtained: After the intravenous injection of a "pellet" tracer, a renal blood perfusion and the dynamic imaging of renal function were immediately performed. The renal blood perfusion imaging and curve exhibited normal renal perfusion. The renal function curve showed that the aggregation segment of the left kidney was available and that the peak time was delayed, thus showing a parabolic curve. The right kidney could be clustered and cleared. The GFR was as follows: 25.47 mL/min for the left kidney and 47.42 mL/min for the right kidney. Based on the kidney image, the left kidney had an irregular morphology, and the size and shape of the right renal shadow were acceptable.
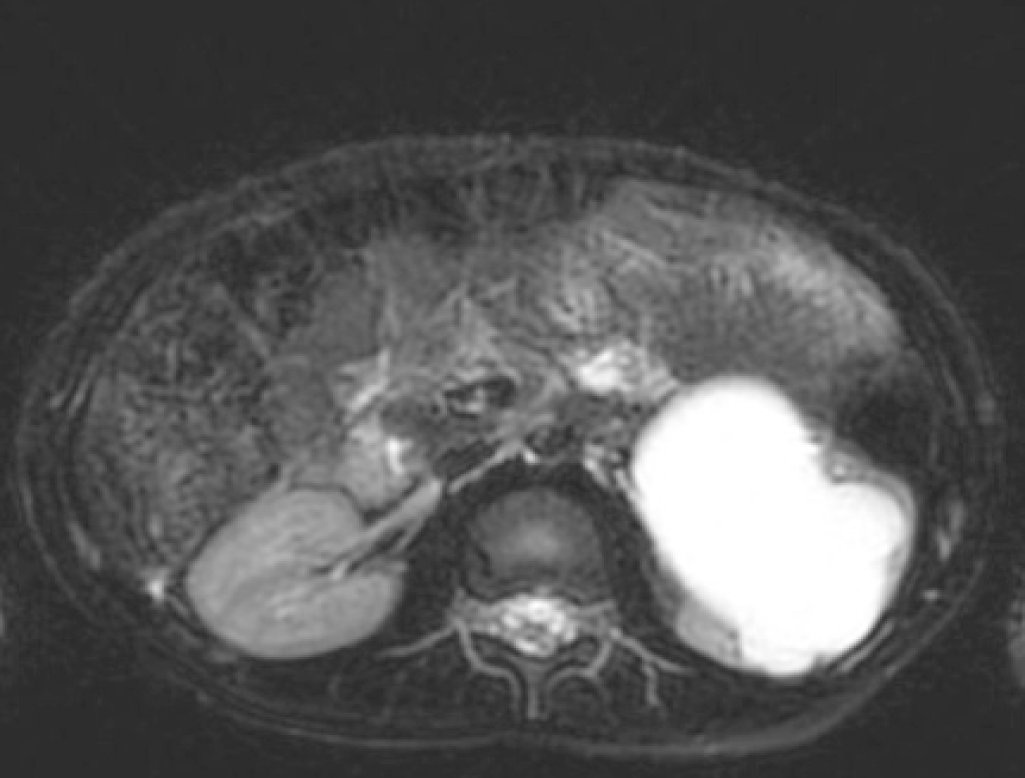
A magnetic resonance examination (Figure 2) showed that the left renal pelvis and ureter were significantly dilated, the widest part of the ureter was approximately 29 mm, the left ureter was stenosed in the middle part, the right renal pelvis, calyces, and ureter were not abnormally stenosed or dilated, and no stones were observed.
For the treatment of left renal duplication, kidney seeper, and left ureteral dilation, retroperitoneal laparoscopic nephrectomy and ureterectomy were performed under general anesthesia.
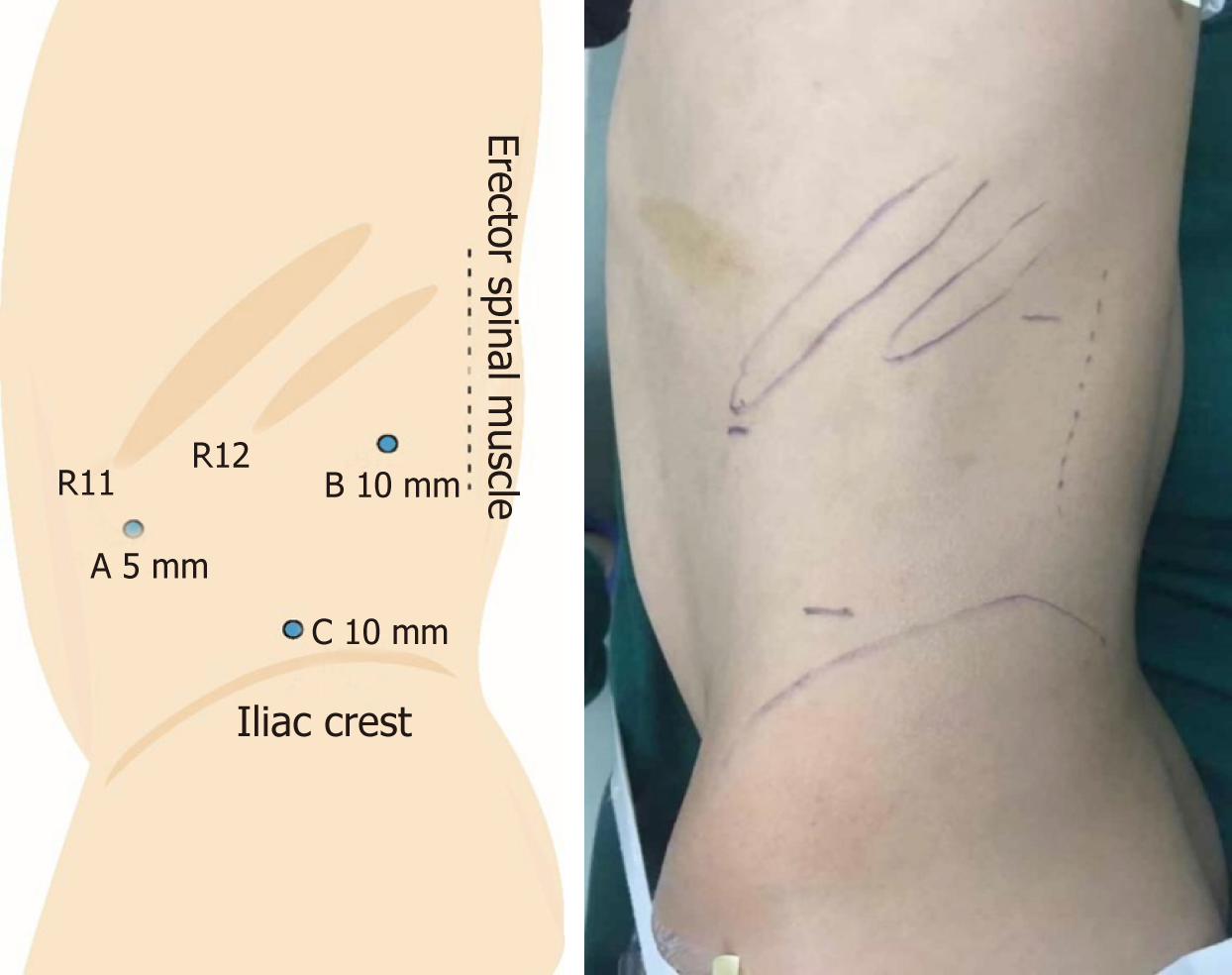
Patients were placed into the right lateral position. After an incision of the upper lumbar triangle was performed in the abdominal cavity, an indicator finger and a balloon expansion were used to establish the pneumoperitoneum (Figure 3). The pressure was observed at 10 mmHg. A 10 mm trocar and laparoscopic lens were inserted, and two trocars (10 mm and 5 mm) were placed in the lower lumbar triangle and the twelve costal tips, respectively.
The left upper kidney was smaller than normal, and the pelvis and ureter were both larger than normal. The junction of the posterior renal fascia and the psoas major muscle was cut open with an ultrasound knife and extended to the upper pole of the kidney. No independent blood supply was found in the lower left kidney. The adhesion between the anterior fascia of the kidney and the posterior peritoneum was separated in the forward position. The peritoneum was broken, and a 5 mm trocar was placed under the xiphoid process, in order to allow for exhaust. The arteries and veins of the left kidney were exposed. The left upper kidney shared the main renal artery with the left lower kidney. There was no obvious boundary between the upper kidney and the lower kidney. The artery clamp was used to block the renal artery. The dilated renal pelvis was cut open, and the colorless clear liquid was absorbed. The duplex kidney was resected along the junction of the pyoid sac wall and the renal parenchyma with an ultrasonic knife. A 1-0 barbed wire was used to continuously suture the renal section, and the renal artery clamp was released. No obvious bleeding was observed. The renal artery was blocked for 40 minutes. The ureters of the left upper kidney and the left lower kidney converged below the level of the iliac crest. The ureter of the left lower kidney became significantly thinner at the junction, and a hemlock was used to clamp the lower kidney ureter. The lower left kidney and ureter were removed from the body with an 8 cm bag and were rinsed. No obvious bleeding was found during the reexamination period. The negative pressure drainage tube was retained in the retroperitoneal cavity and was drilled out of the body under the trocar in the lower lumbar triangle. The following sutures were utilized: A 3-0 absorbable line intermittent suture for the abdominal wall muscle, a 4-0 absorbable line inter-mittent suture for subcutaneous tissue, and a biological protein adhesive for the skin. A pull film was used to tighten the skin of all of the incisions, and a dressing was used to cover the incisions.
The patient was safely returned to the ward postoperation, with 100 mL of bleeding and no need for a blood transfusion. The left lower kidney and ureter were sent for pathological examinations.
The postoperative recovery consisted of diet, optimal consciousness levels, and good spirits. After a conventional anti-infection treatment, a total volume of 116 mL of the postoperative peritoneal drainage was drained (which was clear after bleeding), and the drainage tube was extracted on the third day after the surgery. On the sixth day after the surgery, the patient met the discharge indications and was discharged for treatment. The following pathological diagnoses were made: Lower left atrophy of the renal parenchyma, decrease of glomerular number with fibrosis, decrease of renal tubules in several regions, epithelial hyperplasia of the collecting tubes, and inter-stitial fibrous tissue hyperplasia with lymphocyte infiltration. The renal pelvis was dilated, the mucosa exhibited chronic inflammation, the epithelium underwent atrophy and became thinner, and the subepithelium underwent interstitial fibrous tissue hyperplasia, which conformed to the hydronephrosis change. There was also ureteral cystic dilation, with chronic inflammation of the mucosa.
The final diagnosis was left renal duplication, kidney seeper, and left ureteral dilation.
For the treatment of left renal duplication, kidney seeper, and left ureteral dilation, retroperitoneal laparoscopic nephrectomy and ureterectomy were performed under general anesthesia.
The patient was discharged after recovery. No recurrence was found after two years of follow-up.
In clinical practice, duplicate kidney is closely related to the formation of ureteral mal-formations. Duplex kidney is usually divided into three types: Developmental type, hydronephrosis type, and dysplasia type. This patient was classified as having the hydronephrosis type; specifically, the patient had a left hydronephrosis combined with a ureteral cyst. Ureteral malformations can be divided into complete and incomplete types. This patient had a complete ureteral malformation with double ureters. B-ultrasound examination is the preferred method for preliminary screening and for follow-up review. The commonly used treatment method is laparoscopic heminephrectomy, which is divided into a peritoneal approach and retroperitoneal approach, both of which are relatively complex operations and are still not used to a high degree in pediatric urology[7,8].
In 1993, Jordan et al[9] first reported on the use of laparoscopic heminephrectomy, which caused great repercussions in this medical field. Afterwards, laparoscopic heminephrectomy gradually replaced the use of open surgery due to its unique advantages and was widely accepted for use by pediatric urologists. In 2000, with the development of endoscopic technology, Miyazato et al[10] reported on the first case of retroperitoneal laparoscopic heminephrectomy, which posed a challenge to the technology that was being used by pediatric urologists. Since then, the advantages and disadvantages of the two different surgical approaches have become a focus of debate.
The advantages of the laparoscopic approach mainly include comprehensive exposure to the anatomy of the kidney and its blood vessels, ability to easily suture the kidney in vivo, and ability to easily identify the nonfunctional kidney, which are crucial steps in this operation. Regardless of the age of the child, and as long as there is bowel preparation before the surgery, the entire kidney can then be assessed. Castellan et al[11] compared 48 cases of seminephrectomy through the abdominal cavity by the use of the retroperitoneal approach. They believed that the peritoneal approach provided better exposure space and recommended the use of the peritoneal approach for infants less than 1 year old[11]. Another advantage of the laparoscopic approach is that the entire ureter surrounding the bladder dome can be almost completely removed, which is a good choice for patients with ureteral dilation, reflux, and tortuosity, and is especially useful for patients with urinary tract infections. Esposito et al[3] analyzed 102 cases of partial nephrectomy and concluded that laparoscopic total ureterectomy was always recommended for patients with urinary tract infections.
However, there are some deficiencies associated with the translaparoscopic ap-proach. Because it passes through the abdominal cavity, the intestinal tract needs to be intraoperatively dissected. Furthermore, the older the patient is, the more extensive the dissection will be. The aim is to obtain an optimal exposure of the kidney and the ureter. Subsequently, this increases the incidence of postoperative urine leakage in patients[3]; additionally, intestinal adhesion, intestinal obstruction, and other complications may occur. These conditions can affect postoperative healing and increase the average length of hospital stay.
In comparison, the advantages of retroperitoneoscopy mainly include the fact that it provides a more direct access to the kidney and avoids the risk of colon dissociation, damage to the hollow organs, and the potential risk of adhesion[12,13]. A retrospective comparative study, conducted by Rassweiler et al[14], concluded that the retro-peritoneal approach is less invasive to the body than the peritoneal approach. Singh et al[15] reported 42 cases of retroperitoneal laparoscopic heminephrectomy, and they believed that direct exposure through the use of retroperitoneal laparoscopy avoided intestinal complications and resulted in faster recovery rates. Another advantage of retroperitoneoscopy is that postoperative urine leakage and bleeding or hematomas are confined to the retroperitoneum. This reduces urine and blood irritation to the peritoneum and postoperative pain. Such limitations also facilitate drainage. In this case, we left a drainage tube in and pulled it out three days later.
CO2 pneumoperitoneum is also a quiet critical factor during the operation. Schauer et al[16] believed that the amount of CO2 absorption through the retroperitoneal route is less than that through the abdominal cavity. The absorbance of too much CO2 will definitely increase the risk of hypercapnia, which will then lead to a series of compli-cations. However, studies have shown that hemodynamic changes that are caused by retroperitoneal CO2 pneumoperitoneum are statistically significant, compared with those that are caused by the peritoneum[17]. Therefore, this may be associated with reduced renal blood flow, which could then lead to functional renal ischemia. Wallis et al[13] believed that, due to the small retroperitoneal space, infants who are younger than 1 year old may be more affected by a pneumoperitoneum, and they recommended the use of an open heminephrectomy for infants under the age of 1 year.
Compared with laparoscopy, retroperitoneoscopy requires higher technical re-quirements, which involves a narrow space of operation of the surgeon[18-20], as well as the reverse anatomy of the kidney and umbilical regions. Additionally, the younger the child is, the narrower the peritoneal space becomes. In this case, the retroperitoneal approach exhibits its advantage, and our traditional retroperitoneal approach is used as the lateral approach in the lateral supine position. Borzi[19] and Mushtaq et al[21] described the method of the posterior approach in the prone position. They believed that, although the posterior approach required the continuous traction of the kidney, it was easier to enter the renal blood vessels in a completely prone position, and the effects of peritoneal tear and pneumoperitoneum were avoided.
Retroperitoneal laparoscopy may not be able to maximally remove dilated ureters, thus resulting in an increased incidence of postoperative symptomatic ureteral residues[3,19]. The ureter near the bladder dome can be completely removed by the use of the laparoscopic approach, but Borzi[19] believes that, when a ureterectomy is needed, the lateral approach can be utilized in older children, which can create a larger working space and a wider field of vision in ureterectomy.
The incidence rates of complications and conversion to open surgery in the retroperitoneoscopic approach are higher than those through the laparoscopic approach, which has been reported more in domestic and foreign studies concerning the use of retroperitoneal laparoscopic heminephrectomy in children[3,11,13]. In 2015, Esposito et al[20] reported that the high technical requirements and small operating range of retroperitoneoscopy led to higher complication and conversion rates, and their recent studies have shown that these rates are decreasing.
Leclair et al[8] found that the probability of switching to open surgery was related to surgical experience, and these findings reflected that retroperitoneal laparoscopic technology was not fully popularized in the field of pediatric urology, and these pediatric urologists need this experience.
In recent years, with the development of surgical techniques and surgical instruments in the medical industry, robotic[22] and tranumbilical single-hole[23] heminephrectomy have emerged, which have caused great repercussions in the industry. But research into these new technologies is scarce, and the increased finan-cial burden on patients requires further investigation.
Laparoscopic and retroperitoneal heminephrectomies are the standard procedures in most pediatric urological centers. The retroperitoneoscopic approach is more consistent with the principle of minimally invasive surgery than the laparoscopic approach, even with a steep learning curve and restricted space. It may be a feasible surgical approach for selective pediatric patients.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Facciorusso A, Musquer N S-Editor: Wang JL L-Editor: Wang TQ E-Editor: Wu YXJ
| 1. | Kazemi-Rashed F, Simforoosh N. Gil-Vernet antireflux surgery in treatment of lower pole reflux. Urol J. 2005;2:20-22. [PubMed] |
| 2. | Seibold J, Schilling D, Nagele U, Anastasiadis AG, Sievert KD, Stenzl A, Corvin S. Laparoscopic heminephroureterectomy for duplex kidney anomalies in the pediatric population. J Pediatr Urol. 2008;4:345-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Esposito C, Escolino M, Miyano G, Caione P, Chiarenza F, Riccipetitoni G, Yamataka A, Savanelli A, Settimi A, Varlet F, Patkowski D, Cerulo M, Castagnetti M, Till H, Marotta R, La Manna A, Valla JS. A comparison between laparoscopic and retroperitoneoscopic approach for partial nephrectomy in children with duplex kidney: a multicentric survey. World J Urol. 2016;34:939-948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | You D, Bang JK, Shim M, Ryu DS, Kim KS. Analysis of the late outcome of laparoscopic heminephrectomy in children with duplex kidneys. BJU Int. 2010;106:250-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Gundeti MS, Patel Y, Duffy PG, Cuckow PM, Wilcox DT, Mushtaq I. An initial experience of 100 paediatric laparoscopic nephrectomies with transperitoneal or posterior prone retroperitoneoscopic approach. Pediatr Surg Int. 2007;23:795-799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Esposito C, Escolino M, Castagnetti M, Savanelli A, La Manna A, Farina A, Turrà F, Roberti A, Settimi A, Varlet F, Till H, Valla JS. Retroperitoneal and laparoscopic heminephrectomy in duplex kidney in infants and children. Transl Pediatr. 2016;5:245-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Miranda ML, Oliveira-Filho AG, Carvalho PT, Ungersbock E, Olimpio H, Bustorff-Silva JM. Laparoscopic upper-pole nephroureterectomy in infants. Int Braz J Urol. 2007;33:87-91; discussion 91-3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Leclair MD, Vidal I, Suply E, Podevin G, Héloury Y. Retroperitoneal laparoscopic heminephrectomy in duplex kidney in infants and children: a 15-year experience. Eur Urol. 2009;56:385-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 45] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 9. | Jordan GH, Winslow BH. Laparoendoscopic upper pole partial nephrectomy with ureterectomy. J Urol. 1993;150:940-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 141] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 10. | Miyazato M, Hatano T, Miyazato T, Kagawa H, Yonou H, Ogawa Y. Retroperitoneoscopic heminephrectomy of the right upper collecting system emptying into an ectopic ureterocele in a 5-year-old girl: a case report. Hinyokika Kiyo. 2000;46:413-416. [PubMed] |
| 11. | Castellan M, Gosalbez R, Carmack AJ, Prieto JC, Perez-Brayfield M, Labbie A. Transperitoneal and retroperitoneal laparoscopic heminephrectomy--what approach for which patient? J Urol. 2006;176:2636-9; discussion 2639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 56] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 12. | Lee RS, Retik AB, Borer JG, Diamond DA, Peters CA. Pediatric retroperitoneal laparoscopic partial nephrectomy: comparison with an age matched cohort of open surgery. J Urol. 2005;174:708-11; discussion 712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 94] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 13. | Wallis MC, Khoury AE, Lorenzo AJ, Pippi-Salle JL, Bägli DJ, Farhat WA. Outcome analysis of retroperitoneal laparoscopic heminephrectomy in children. J Urol. 2006;175:2277-80; discussion 2280-2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 96] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 14. | Rassweiler J, Frede T, Henkel TO, Stock C, Alken P. Nephrectomy: A compara-tive study between the transperitoneal and retroperitoneal laparoscopic versus the open approach. Eur Urol. 1998;33:489-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 89] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 15. | Singh RR, Wagener S, Chandran H. Laparoscopic management and outcomes in non-functioning moieties of duplex kidneys in children. J Pediatr Urol. 2010;6:66-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Schauer PR, Luna J, Ghiatas AA, Glen ME, Warren JM, Sirinek KR. Pulmonary function after laparoscopic cholecystectomy. Surgery. 1993;114:389-97; discussion 397-9. [PubMed] |
| 17. | Halachmi S, El-Ghoneimi A, Bissonnette B, Zaarour C, Bagli DJ, McLorie GA, Khoury AE, Farhat W. Hemodynamic and respiratory effect of pediatric urological laparoscopic surgery: a retrospective study. J Urol. 2003;170:1651-4; discussion 1654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 32] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Valla JS. Retroperitoneoscopic surgery in children. Semin Pediatr Surg. 2007;16:270-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Borzi PA. A comparison of the lateral and posterior retroperitoneoscopic approach for complete and partial nephroureterectomy in children. BJU Int. 2001;87:517-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 88] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 20. | Esposito C, Miyano G, Caione P, Escolino M, Chiarenza F, Riccipetitoni G, Yamataka A, Cerulo M, Savanelli A, Settimi A, Valla JS. Retroperitoneoscopic Heminephrectomy in Duplex Kidney in Infants and Children: Results of a Multicentric Survey. J Laparoendosc Adv Surg Tech A. 2015;25:864-869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 21. | Mushtaq I, Haleblian G. Laparoscopic heminephrectomy in infants and children: first 54 cases. J Pediatr Urol. 2007;3:100-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 22. | Ballouhey Q, Binet A, Clermidi P, Braik K, Villemagne T, Cros J, Lardy H, Fourcade L. Partial nephrectomy for small children: Robot-assisted versus open surgery. Int J Urol. 2017;24:855-860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 23. | Urbanowicz W, Sulisławski J, Wolnicki M. Pediatric single port transumbilical nephrectomy and nephroureterectomy. Cent European J Urol. 2011;64:240-242. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |