Published online Aug 16, 2018. doi: 10.12998/wjcc.v6.i8.214
Peer-review started: March 9, 2018
First decision: April 4, 2018
Revised: April 10, 2018
Accepted: June 7, 2018
Article in press: June 8, 2018
Published online: August 16, 2018
Processing time: 160 Days and 17 Hours
We report the case of a 56-year-old woman with pancreatic adenocarcinoma (PA) discovered during an episode of febrile jaundice. A computed tomography (CT) scan showed a mass in the head of the pancreas with circumferential infiltration of the superior mesenteric vein (SMV) and dilatation of the biliary and pancreatic ducts without metastases. The patient benefited from neoadjuvant chemotherapy (FOLFIRINOX) followed by radio-chemotherapy (45 Gy) and chemotherapy (LV5FU2). The revaluation CT revealed SMV thrombosis without portal vein (PV) thrombosis. There was no contact of the tumor with the PV. Pancreatoduodenectomy with combined resection of the SMV was performed with no reconstruction of this venous axis after confirmation of adequate PV, splenic, and left gastric venous flow and the absence of bowel ischemia. The pathological diagnosis was pT4N1R0 PA. There were no bowel angina issues during the follow-up period. At 15 mo after surgery, the patient died of metastatic recurrence.
Core tip: This case report showed that a short superior mesenteric vein resection could be achieved during pancreatoduodenectomy without venous reconstruction, when an appropriate small bowel venous outflow is ensured by inferior mesenteric vein.
- Citation: Jouffret L, Guilbaud T, Turrini O, Delpero JR. Pancreaticoduodenectomy with combined superior mesenteric vein resection without reconstruction is possible: A case report and review of the literature. World J Clin Cases 2018; 6(8): 214-218
- URL: https://www.wjgnet.com/2307-8960/full/v6/i8/214.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i8.214
Tumor resection is the only effective treatment option in patients with pancreatic adenocarcinoma (PA), and achieving macroscopic and microscopic complete resection (R0) is critical for long-term survival[1]. When the tumor involves either the superior mesenteric vein (SMV) or the portal vein (PV), SMV\PV resection is necessary at the time of pancreaticoduodenectomy (PD) to obtain his-tologically negative surgical margins[2,3]. Venous reconstruction is not usually a technical challenge, and end-to-end anastomosis is routinely performed with good 5-year patency rates[4]. In some case, involvement of first-order branches of the SMV increases the difficulty of venous reconstruction. We report the case of a patient presenting with PA with circumferential infiltration of the SMV and first-order branches in whom no venous reconstruction was performed.
A 56-year-old woman underwent abdominal computed tomography (CT) because of febrile jaundice. The CT scan revealed a mass (29 mm × 20 mm) in the head of the pancreas with circumferential infiltration of the SMV and dilatation of the biliary and pancreatic ducts. There was no metastasis.
An echo-endoscopy with retrograde catheterization was realized with stenting of the biliary duct. This exam affirmed the diagnosis of locally advanced PA. Neoadjuvant therapy was planned before surgical revaluation. The patient received neoadjuvant chemotherapy with 6 cycles of FOLFIRINOX followed by radio-chemotherapy at 45 Gy over 5 wk associated with LV5-FU2 chemotherapy. The revaluation CT performed after neoadjuvant therapy revealed SMV thrombosis but no PV thrombosis and no contact with the tumor (Figure 1). There was no ar-gument for a tumor origin of thrombosis, it was not enhanced by contrast product. There were some collaterals vessels from SMV to the Inferior Mesenteric Venous (IMV). A multidisciplinary tumor board decided on surgical resection, and PD was planned.
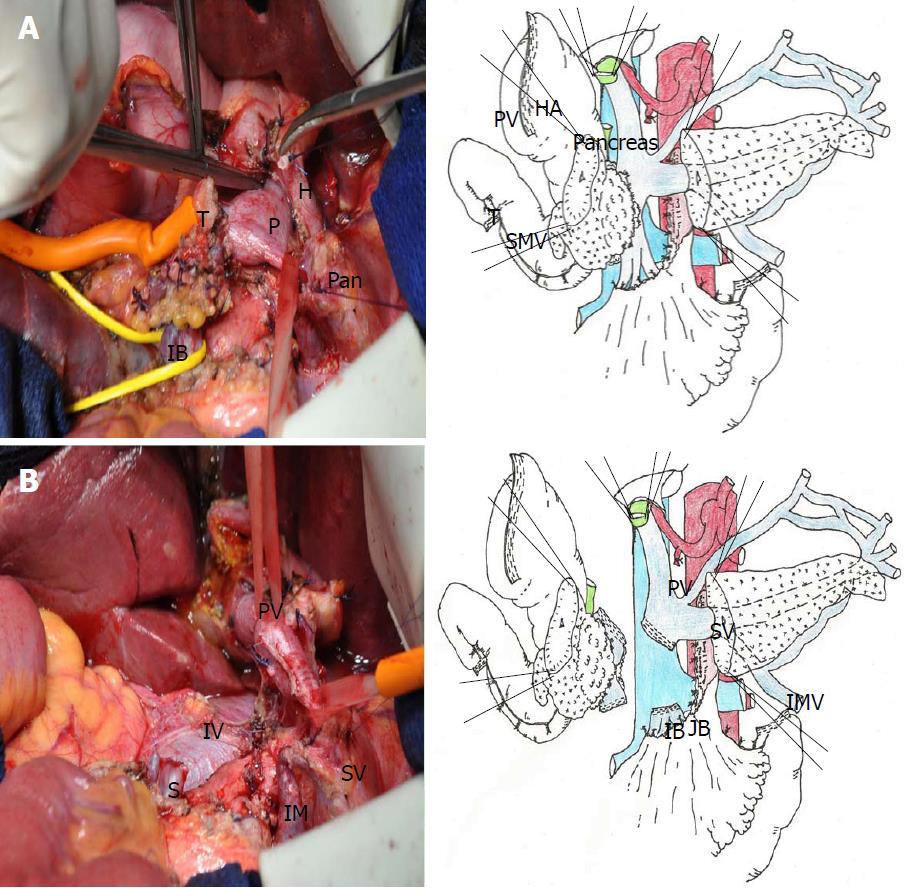
On exploration, there was no evidence of metastasis or peritoneal nodularity. We first approached the superior mesenteric artery to be sure of the resectability of the tumor. The intraoperative frozen-section analysis result of the superior mesenteric artery margins was negative. After dissection, we found a point of tumor contact with the SMV. There was SMV thrombosis, but the PV and splenomesaraic confluence were tumorfree. PD combined with SMV resection was performed to obtain a negative surgical margin. We mechanically sectioned the distal extremity of the SMV and selectively ligated the ileum and jejunum veins under the tumor. No reconstruction of this venous axis was realized after confirming, by a clamping test, adequate PV, splenic, and left gastric venous flow and the absence of bowel ischemia. We performed a Child reconstruction with pancreatojejunostomy and external pancreatic duct stenting and drainage (Figure 2). Surgery lasted 10 hours. There was less bleeding, and no transfusion. We inked the tumor margins to differentiate areas of venous, arterial and posterior margin resection. The pathological diagnosis was PA with poor differentiation, lymph node metastasis (2N+/5), vascular and perineural invasion, and SMV wall infiltration, ypT3N1M0. All resection margins were tumor-free.
During the postoperative course, the patient developed isolated chylous ascites that disappeared spontaneously in a few weeks. Control CT after surgery showed an aspect of aspecific colitis with edema in the mesenteric structures of the colon. The patient was released from the hospital after fifteen days. A multidisciplinary tumor board decided there were no indications for adjuvant therapy because of clinical and nutritional state of patient. Subsequently, the patient experienced metastatic evolution with hepatic and pulmonary lesions at 6 mo. Unfortunately, the patient died of metastatic progression, 15 mo after the surgery, with no evidence of local recurrence.
In this case, no reconstruction after venous resection without the use of autologous or prosthetic grafts was feasible. As SMV thrombosis was observed before the surgery, venous drainage of the small bowel was achieved via the lower mesenteric and splenic veins, and reconstruction of the SMV was not necessary. PD with SMV resection and without reconstruction was performed in two another cases, as described by Hashimoto et al[5], after confirming adequate PV flow and no small intestine congestion, and by Tang et al[6], who performed the same operation with anastomosis between the splenic vein and PV without SMV reconstruction.
The poor prognosis of this condition is partly due to local invasion of the tumor into the tissues around the pancreas. In this case, PD combined with venous resection was performed to treat pancreatic head adenocarcino-ma with tumor-vein contact and/or invasion to obtain R0 resection. The rationale for radical surgical excision is based on the poorer survival rate in patients with incomplete resection (R1) (14-21 mo) than in patients with R0 resection (18-28 mo), as determined by the study with the largest series of cases performed in an specialized center[7-10]. The definition of R1 resection has not been standardized. Chang et al[11] showed that a tumor clearance greater than 1.5 mm in the retroperitoneal section was an independent predictor of long-term survival in a multivariate analysis in 365 patients. Delpero et al[12] demonstrated that the standardized and systematic inking of the retroperitoneal margin increased the rates of R1 resection; additionally, these researchers confirmed the importance of R0 resection with a significantly lower 2-year disease-free survival rate in patients with R1 resection (R1: 26.5% vs R0: 42%; P = 0.02). In patients with R1 resection, the site of microscopic involvement impacted survival, and patients with involvement of vascular margins had poorer survival than patients with involvement of posterior margins[13].
When a tumor is in contact with the PV, tumor invasion occurs in only 50%-65% of cases, and involvement of the PV is a factor of a poor prognosis[14,15]. However, venous resection could increase the rate of R0 resection and be justified to increase the clearance of the retroportal resection margins. Additionally, Turrini et al[16] showed better 3-year overall survival in patients with no venous involvement who underwent PV resection than in those who did not (42% vs 22%, P = 0.04).
Many studies have not found any significant differences in terms of postoperative morbidity and mortality after venous resection[17]. Long-term results after PV reconstruction have shown 1- and 5-year patency rates of 50%-80% and 17%, respectively. There have been some cases of early thrombosis after PV reconstruction, with no major complications. Stenosis of the PV reconstruction area has been shown to be associated with local recurrence[4].
In most cases requiring reconstruction, end-to-end anastomosis is used, but some authors have described the use of autologous venous grafts or prosthetic patches in cases with long resection distances, with similar postoperative outcomes. Therefore, some patients developed thrombosis earlier in their graft, leading to large-volume ascites requiring paracentesis[18].
The involvement of first-order branches of the SMV is a surgical challenge. In a report by Katz et al[19], segmental resection of one of the two first-order branches of the SMV could be performed without reconstruction if the remaining branch is preserved and assures collateral mesenteric venous drainage.
Acute thrombosis of the PV and SMV can lead to mesenteric venous ischemia. Thus, the lack of feasible reconstruction has historically been a contraindication of pancreatic resection. Data from the trauma literature suggest that SMV ligation can be performed without dramatic consequences[20]. Therefore, in cases of chronic SMV obstruction by a tumor or previous thrombosis, the development of collateral flow through the inferior mesenteric and splenic veins allows ligation of the SMV.
In conclusion, before surgery, high-quality CT needs to be performed to identify chronic venous obstructions by tumor involvement or thrombosis, evaluate the development of venous collaterality, and determine the feasibility of resection with or without PV reconstruction.
A 56-year-old woman with a locally advanced pancreatic adenocarcinoma (PA).
Febrile Jaundicy.
Ca 19-9 42, cholestasis decreased after biliary stenting.
Computed tomography scan revealed superior mesenteric vein (SMV) thrombosis but no PV thrombosis and no contact with head PA.
PA with poor differentiation, lymph node metastasis (2N+/5), vascular and perineural invasion, and SMV wall infiltration. All resection margins were tumor-free.
Pancreaduodenectomy with SMV resection without reconstruction.
No reconstruction of this venous axis was realized after confirming adequate portal veinous, splenic, and left gastric venous flow and the absence of bowel ischemia.
Development of collateral flow through the inferior mesenteric and splenic veins allows ligation of the superior mesenteric venous.
This case report showed that a short SMV resection could be achieved during pancreatoduodenectomy without venous reconstruction, when an appropriate small bowel venous outflow is ensured by inferior mesenteric vein.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: France
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Fujino Y, Memeo R, Nakano H, Peng B, Uchiyama H S- Editor: Ji FF L- Editor: A E- Editor: Tan WW
| 1. | Howard TJ, Krug JE, Yu J, Zyromski NJ, Schmidt CM, Jacobson LE, Madura JA, Wiebke EA, Lillemoe KD. A margin-negative R0 resection accomplished with minimal postoperative complications is the surgeon’s contribution to long-term survival in pancreatic cancer. J Gastrointest Surg. 2006;10:1338-1345; discussion 1345-1346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 242] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 2. | Adham M, Jaeck D, Le Borgne J, Oussoultzouglou E, Chenard-Neu MP, Mosnier JF, Scoazec JY, Mornex F, Partensky C. Long-term survival (5-20 years) after pancreatectomy for pancreatic ductal adenocarcinoma: a series of 30 patients collected from 3 institutions. Pancreas. 2008;37:352-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 57] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 3. | Carrère N, Sauvanet A, Goere D, Kianmanesh R, Vullierme MP, Couvelard A, Ruszniewski P, Belghiti J. Pancreaticoduodenectomy with mesentericoportal vein resection for adenocarcinoma of the pancreatic head. World J Surg. 2006;30:1526-1535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 88] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 4. | Kang MJ, Jang JY, Chang YR, Jung W, Kim SW. Portal vein patency after pancreatoduodenectomy for periampullary cancer. Br J Surg. 2015;102:77-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 50] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 5. | Hashimoto M, Makuuchi M, Matsuda M, Watanabe G. Superior mesenteric vein resection without reconstruction in pylorus-preserving pancreatoduodenectomy for pancreatic head cancer. Hepatogastroenterology. 2010;57:1087-1089. [PubMed] |
| 6. | Tang J, Abbas J, Hoetzl K, Allison D, Osman M, Williams M, Zelenock GB. Ligation of superior mesenteric vein and portal to splenic vein anastomosis after superior mesenteric-portal vein confluence resection during pancreaticoduodenectomy - Case report. Ann Med Surg (Lond). 2014;3:137-140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Schnelldorfer T, Ware AL, Sarr MG, Smyrk TC, Zhang L, Qin R, Gullerud RE, Donohue JH, Nagorney DM, Farnell MB. Long-term survival after pancreatoduodenectomy for pancreatic adenocarcinoma: is cure possible? Ann Surg. 2008;247:456-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 339] [Cited by in RCA: 377] [Article Influence: 22.2] [Reference Citation Analysis (0)] |
| 8. | Winter JM, Cameron JL, Campbell KA, Arnold MA, Chang DC, Coleman J, Hodgin MB, Sauter PK, Hruban RH, Riall TS. 1423 pancreaticoduodenectomies for pancreatic cancer: A single-institution experience. J Gastrointest Surg. 2006;10:1199-1210; discussion 1210-1211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1125] [Cited by in RCA: 1122] [Article Influence: 59.1] [Reference Citation Analysis (0)] |
| 9. | Fatima J, Schnelldorfer T, Barton J, Wood CM, Wiste HJ, Smyrk TC, Zhang L, Sarr MG, Nagorney DM, Farnell MB. Pancreatoduodenectomy for ductal adenocarcinoma: implications of positive margin on survival. Arch Surg. 2010;145:167-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 140] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 10. | Rau BM, Moritz K, Schuschan S, Alsfasser G, Prall F, Klar E. R1 resection in pancreatic cancer has significant impact on long-term outcome in standardized pathology modified for routine use. Surgery. 2012;152:S103-S111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 105] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 11. | Chang DK, Johns AL, Merrett ND, Gill AJ, Colvin EK, Scarlett CJ, Nguyen NQ, Leong RW, Cosman PH, Kelly MI. Margin clearance and outcome in resected pancreatic cancer. J Clin Oncol. 2009;27:2855-2862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 267] [Cited by in RCA: 247] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 12. | Delpero JR, Bachellier P, Regenet N, Le Treut YP, Paye F, Carrere N, Sauvanet A, Autret A, Turrini O, Monges-Ranchin G. Pancreaticoduodenectomy for pancreatic ductal adenocarcinoma: a French multicentre prospective evaluation of resection margins in 150 evaluable specimens. HPB (Oxford). 2014;16:20-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 130] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 13. | Pingpank JF, Hoffman JP, Ross EA, Cooper HS, Meropol NJ, Freedman G, Pinover WH, LeVoyer TE, Sasson AR, Eisenberg BL. Effect of preoperative chemoradiotherapy on surgical margin status of resected adenocarcinoma of the head of the pancreas. J Gastrointest Surg. 2001;5:121-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 124] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 14. | Siriwardana HP, Siriwardena AK. Systematic review of outcome of synchronous portal-superior mesenteric vein resection during pancreatectomy for cancer. Br J Surg. 2006;93:662-673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 164] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 15. | Nakao A, Kanzaki A, Fujii T, Kodera Y, Yamada S, Sugimoto H, Nomoto S, Nakamura S, Morita S, Takeda S. Correlation between radiographic classification and pathological grade of portal vein wall invasion in pancreatic head cancer. Ann Surg. 2012;255:103-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 148] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 16. | Turrini O, Ewald J, Barbier L, Mokart D, Blache JL, Delpero JR. Should the portal vein be routinely resected during pancreaticoduodenectomy for adenocarcinoma? Ann Surg. 2013;257:726-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 61] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 17. | Ouaïssi M, Turrini O, Hubert C, Louis G, Gigot JF, Mabrut JY. Vascular resection during radical resection of pancreatic adenocarcinomas: evolution over the past 15 years. J Hepatobiliary Pancreat Sci. 2014;21:623-638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | Chu CK, Farnell MB, Nguyen JH, Stauffer JA, Kooby DA, Sclabas GM, Sarmiento JM. Prosthetic graft reconstruction after portal vein resection in pancreaticoduodenectomy: a multicenter analysis. J Am Coll Surg. 2010;211:316-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 86] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 19. | Katz MH, Fleming JB, Pisters PW, Lee JE, Evans DB. Anatomy of the superior mesenteric vein with special reference to the surgical management of first-order branch involvement at pancreaticoduo-denectomy. Ann Surg. 2008;248:1098-1102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 66] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 20. | Asensio JA, Petrone P, Garcia-Nuñez L, Healy M, Martin M, Kuncir E. Superior mesenteric venous injuries: to ligate or to repair remains the question. J Trauma. 2007;62:668-675; discussion 675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 50] [Article Influence: 2.8] [Reference Citation Analysis (0)] |