Published online Dec 26, 2018. doi: 10.12998/wjcc.v6.i16.1199
Peer-review started: October 18, 2018
First decision: November 8, 2018
Revised: November 12, 2018
Accepted: November 23, 2018
Article in press: November 24, 2018
Published online: December 26, 2018
Processing time: 67 Days and 18.8 Hours
Vaginal abscess is a treatable disease and should be considered in female patients with voiding difficulties and perineal tenderness. There are no reported cases of vaginal abscess causing voiding dysfunction in the absence of a previous surgery. Early diagnosis and drainage of vaginal abscesses may lead to excellent outcomes.
We presented a case of vaginal abscess that caused voiding dysfunction without surgery history. A 64-year-old woman had a past history of type 2 diabetes mellitus. She came to our clinic following urinary difficulty with perineal tenderness. Bladder ultrasonography revealed a pelvic cystic lesion with a mass effect on the bladder. The presence of a vaginal abscess was suspected following pelvic examination and transvaginal ultrasound. After transvaginal drainage of the vaginal abscess and a full course of antibiotic treatment, she recovered well without any urination symptoms.
Voiding dysfunction caused by vaginal abscess is rare but should be considered in female patients with perineal tenderness.
Core tip: Vaginal abscess is a treatable disease and should be considered in female patients with voiding difficulties and perineal tenderness. To our knowledge, this is the first reported case of vaginal abscess causing voiding dysfunction in the absence of a previous surgery.
- Citation: Yeh CC, Yang SSD, Huang SC, Wang YC. Uncommon cause of voiding dysfunction in a female patient-vaginal abscess: A case report. World J Clin Cases 2018; 6(16): 1199-1201
- URL: https://www.wjgnet.com/2307-8960/full/v6/i16/1199.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i16.1199
Voiding dysfunction is a clinical condition that affects voiding and causes lower urinary tract symptoms. It is not an unusual complaint in middle-aged women, and the prevalence of female voiding dysfunction varies between 2%-25% based on the study[1-5]. Voiding dysfunction might be related to detrusor underactivity and bladder outlet obstruction[6]. The etiology of bladder outlet obstruction could have either an anatomical or a functional cause[7]. In order to identify the cause of voiding dysfunction, previous medical history should be obtained, as well as a physical examination, urine analysis, uroflowmetry, and ultrasonography[8]. Vaginal abscess is a treatable disease; it may cause voiding difficulty but could easily be neglected when the patient is afebrile with no previous history of surgery. We presented an unusual case of voiding dysfunction due to vaginal abscess.
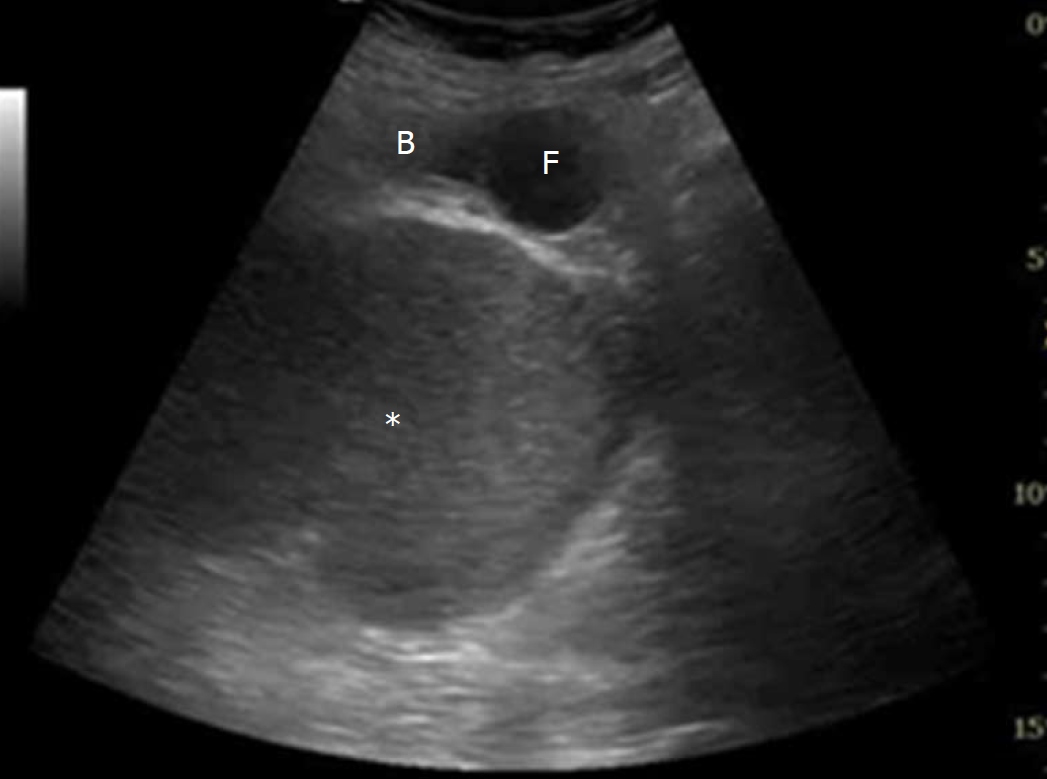
A 64-year-old woman with a past history of type 2 diabetes mellitus (under medical control by sitagliptin 100 mg per day for 5 years) experienced progressive voiding difficulty without fever for 2 mo. She had not undergone any previous urological or gynecological surgery. Urinary analysis showed pyuria, and she was admitted to our ward for further treatment. Bladder ultrasonography revealed urinary retention and a pelvic cystic lesion with a mass effect on the bladder (Figure 1). During admission, she also complained of perineal pain when she started to sit on a chair. Therefore, we arranged a pelvic computed tomography and the report showed a cystic lesion (9.1 cm) in the right lower pelvic region (Figure 2). Urologists were consulted and urodynamic studies were arranged. Uroflowmetry revealed an interrupted flow pattern with elevated post-void residual urine. Video urodynamics showed fair cystometric capacity and detrusor contraction, but the sphincter did not open during the examination. The results of the examinations all supported a diagnosis of bladder outlet obstruction due to a pelvic anatomical lesion. We consulted a gynecological expert, and a mass bulging from the right vaginal wall was found during pelvic examination. Transvaginal ultrasound revealed a pelvic cystic lesion originated from the vaginal wall. A vaginal abscess causing voiding dysfunction was diagnosed.
Voiding dysfunction due to vaginal abscess.
She received transvaginal drainage of the abscess and a full course of intravenous antibiotic treatment with cefuroxime. Urine and pus cultures both grew Escherichia coli. Pathology of this cyst lesion reported adipose tissue and congested vessels with some inflammatory cell infiltration. There was no evidence of malignancy in the sections examined.
After treatment, she recovered well without any urination symptoms. At a 1.5-year follow-up, uroflowmetry disclosed normal bell pattern with acceptable post-void residual urine. The voiding dysfunction did not recur.
A vaginal abscess causing voiding dysfunction is rarely reported. Huang et al presented a case with symptoms of urinary frequency, voiding difficulty, and postvoid dribbling after Burch colposuspension[9]. The presence of a vaginal abscess was confirmed by transvaginal ultrasound, and an incision was made in the abscess wall followed by drainage. With correct diagnosis and treatment, both our patient and the one described by Huang et al showed good recovery of voiding function.
In patients with a long-term history of diabetes mellitus, diabetic cystopathy is highly prevalent[10]. Diabetic cystopathy related to detrusor sphincter dyssynergia is a common cause of voiding difficulty. Full clinical history, physical examination, urodynamic studies, and bladder ultrasound could provide clinical clues for other differential diagnoses of voiding dysfunction. In regard to our patient, the symptoms of perineal tenderness indicated a gynecologic lesion. A pelvic cyst found during bladder ultrasonography suggested an anatomical cause of bladder obstruction.
Vaginal abscess that contains pus or fluid might grow to a substantially large size before causing discomfort to the patient. A large abscess lump might induce pain in the perineal area, which may be aggravated during sitting, walking, or sexual intercourse[9]. Symptomatic abscesses require drainage and marsupialization because abscesses rarely resolve by themselves. The mass effect of the abscess could also be relieved by drainage, and voiding dysfunction could be resolved.
In conclusion, a vaginal abscess should be considered as a differential diagnosis in female patients with voiding difficulty and perineal tenderness. Early diagnosis and management of vaginal abscesses may produce excellent outcomes.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: Taiwan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Choi MR, Ekpenyong CEE S- Editor: Cui LJ L- Editor: Filipodia E- Editor: Wu YXJ
| 1. | Dwyer PL, Desmedt E. Impaired bladder emptying in women. Aust N Z J Obstet Gynaecol. 1994;34:73-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 45] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Stanton SL, Ozsoy C, Hilton P. Voiding difficulties in the female: prevalence, clinical and urodynamic review. Obstet Gynecol. 1983;61:144-147. [PubMed] |
| 3. | Groutz A, Gordon D, Lessing JB, Wolman I, Jaffa A, David MP. Prevalence and characteristics of voiding difficulties in women: are subjective symptoms substantiated by objective urodynamic data? Urology. 1999;54:268-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 80] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 4. | Groutz A, Blaivas JG. Non-neurogenic female voiding dysfunction. Curr Opin Urol. 2002;12:311-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 43] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 5. | Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, Coyne K, Kelleher C, Hampel C, Artibani W. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006;50:1306-1314; discussion 1314-1315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1745] [Cited by in RCA: 1843] [Article Influence: 97.0] [Reference Citation Analysis (0)] |
| 6. | Abdel Raheem A, Madersbacher H. Voiding dysfunction in women: How to manage it correctly. Arab J Urol. 2013;11:319-330. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Lin CD, Kuo HC, Yang SS. Diagnosis and Management of Bladder Outlet Obstruction in Women. Low Urin Tract Symptoms. 2016;8:30-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Payam N, Debjyoti K, Peter D. Female Voiding Dysfunction: a Practical Approach to Diagnosis and Treatment. Curr Obstet Gynecol Rep. 2018;7:74-83. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Huang WC, Yang SH, Yang SY, Yang E, Yang JM. Vaginal abscess mimicking a cystocele and causing voiding dysfunction after Burch colposuspension. J Ultrasound Med. 2009;28:63-66. [PubMed] |
| 10. | Golbidi S, Laher I. Bladder dysfunction in diabetes mellitus. Front Pharmacol. 2010;1:136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 97] [Article Influence: 6.5] [Reference Citation Analysis (0)] |