Published online Nov 6, 2018. doi: 10.12998/wjcc.v6.i13.707
Peer-review started: July 31, 2018
First decision: August 24, 2018
Revised: September 16, 2018
Accepted: October 11, 2018
Article in press: October 11, 2018
Published online: November 6, 2018
Processing time: 98 Days and 6.1 Hours
IgG4-related disease (IgG4-RD) is an increasingly recognized pathological entity that tends to involve multiple organs with an elevated level of serum IgG4, which is easily misdiagnosed owing to sharing common clinical features with a variety of other diseases. Here, we report an interesting IgG4-RD case of a woman with progressive multi-organ involvement for over 19 years, started with swollen eyelids, dry eye and mouth, and polydipsia and hydruria. Imaging diagnosis revealed diffuse enlargement of the parotid glands, enlargement of the head of the pancreas, pulmonary infection and interstitial lung. Serological tests showed a remarkable elevation of the serum IgG4, and cytological analysis further revealed a large amount of lymphoplasmacytic infiltration into the focal lobule, and IgG4-positive cell infiltration in bladder mucosa. Therapeutically, the patient responded well to steroid therapy, and thus, she was diagnosed as IgG4-RD suspicious. This report highlights the importance of an early diagnosis in this autoimmune disease and suggests that patients with a clinically unclear cause of inflammation, swelling and refractory glands, rhinitis, pancreatitis, hypophysitis, and/or interstitial pneumonia should be considered for IgG4-RD. The plasma IgG4 level and lymphoplasmacytic infiltration may be useful indexes for screening, and a low dose of steroid maintaining therapy may offer benefits for patients with IgG4-RD.
Core tip: IgG4-related disease (IgG4-RD) is an easily misdiagnosed immune disorder with an elevated serum IgG4 and multiple organ involvements. Hence, it is important in early diagnosis for guiding clinical treatments. Here, we report an interesting case of a woman with progressive multi-organ involvement of IgG4-RD for 19 years. The 67-year-old woman has suffered from progressive diseases of multiple organs, including lacrimal glands, kidneys, parotid glands, submandibular glands, salivary glands, pituitary, pancreas and lung. Patients with IgG4-RD normally respond well to steroid therapy; however, the broad spectrum of manifestation with commonly clinical features of other diseases easily leads to misdiagnosis and improper treatment in clinical settings. Therefore, this report highlights the importance of early diagnosis in this autoimmune disease.
- Citation: Xue J, Wang XM, Li Y, Zhu L, Liu XM, Chen J, Chi SH. Highlighting the importance of early diagnosis in progressive multi-organ involvement of IgG4-related disease: A case report and review of literature. World J Clin Cases 2018; 6(13): 707-715
- URL: https://www.wjgnet.com/2307-8960/full/v6/i13/707.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i13.707
IgG4-related disease (IgG4-RD) is a systemic and clinical entity with autoimmune pathogenesis, which is characterized by a high level of circulating IgG4 and a dramatic response to steroid therapy[1]. It was first identified in patients with autoimmune pancreatitis (AIP) that was initially described in patients with chronic pancreatitis[2,3]. Although its etiology has not yet been fully determined, the clinical spectrum of this disorder is extremely broad from manifestation in a single organ (pancreas, kidneys, salivary gland, orbit, skin, lungs, prostate, biliary tree, liver, and pituitary gland) to involvement of multiple organs[4,5]. Tumefactive lesions of involved organs (mainly lacrimal glands, pancreas and salivary glands) with pseudotumoral swelling and sclerosis are often its main clinical manifestation. Histopathologically, the involved organs of IgG4-RD are infiltrated with lymphocytes, IgG4-positive plasma cells and variable degrees of fibrosis[1].
Most cases of IgG4-RD occur in middle-aged and elderly males, and here, we retrospectively report a female case with progressive multi-organ involvement of IgG4-RD with over 19 years of disease duration, which highlights the importance in early diagnosis and intervention of IgG4-RD in clinical settings.
Written informed consent was obtained from the patient for publication of this case. The ethics committee of the human research of the General Hospital at Ningxia Medical University approved the informed consent for reporting this case. Table 1 lists the clinical history, examinations and treatment of this patient.
| Time | Investigations | Results |
| February 10, 2000 | Physical examination | Non-specific, non-infective orbital inflammatory pseudotumor |
| July 9, 2003 | CT | Enlargement of double lacrimal glands, parotid glands |
| Lacrimal glands biopsy | Lymphonid pseudotumor of double lacrimal glands | |
| May 21, 2005 | CT | Enlargement of parotid glands |
| B-ultrasonography | Diffused enlargement of parotid glands | |
| November 2, 2005 | Blood routine examination | LYM%: 50.9% (20.0-50.0), LYM#: 2.11 × 10-9/L (1.10-3.20), EOS%: 13.6% (0.4-8.0), EOS#: 0.78 × 10-9/L (0.02-0.50), NEUT%: 68.0% (50.0-70.0), NEUT#: 6.62 × 10-9/L (2.00-7.00) |
| Biochemistry | AST: 628.5 U/L (13.0-35.0), ALT: 648.4 U/L (7.0-40.0), ALP: 356 U/L (50-135), GGT: 422.9 U/L (7.0-45.0) | |
| CT | Enlargement of the head of pancreas | |
| December 4, 2005 | ERCP | Implantation of a biliary stent |
| March 6, 2006 | IGG, RF | High levels of serum IgG, RF, Ig light chain KAP, Ig light chain LAM |
| March 31, 2006 | ERCP | Implantation of two biliary stents |
| Biopsy | Extensive lymphatic plasma cell infiltrated in focal lobular, salivary gland tissue was under the squamous mucosa | |
| July 8, 2006 | IGG, RF | Low levels of serum complement C3 and IgG and Ig light chain KAP, high level of Ig light chain LAM |
| November 4, 2006 | Complement | Low level of serum complement C3 |
| ENA antibody, ANA | HEp2-ANA: positive 1:100 (< 1;100), ENA-AbSSA: negative, ENA-AbSSB: negative | |
| November 8, 2006 | ERCP | Remove of the biliary stent |
| November 26, 2006 | CT | No enlargement of the head of pancreas |
| Physical examination | Normal eyeball, normal conjunctiva, eyelids without edema, normal light reaction | |
| September 4, 2007 | Blood routine examination | Normal parameters |
| September 6, 2007 | Endocrine examinations | Details seen in Table 2 |
| October 10, 2007 | Renal function examination | Normal function |
| May 17, 2008 | MRI | Pituitary stalk thickening |
| October 7, 2009 | CT | Enlargement of the head of pancreas |
| November 13, 2009 | Blood routine examination | LYM%: 46.0% (20.0-50.0), LYM#: 1.92 × 10-9/L (1.10-3.20), EOS%: 23.1% (0.4-8.0), EOS#: 0.89 × 10-9/L (0.02-0.50), NEUT%: 49.0% (50.0-70.0), NEUT#: 5.83 × 10-9/L (2.00-7.00) |
| December 14, 2009 | MRI | Enlargement of the head of pancreas |
| September 20, 2011 | CT | Normal volume of the head of pancreas |
| November 22, 2011 | Bone scan | Rib fracture |
| November 23, 2011 | Blood routine examination | LYM%: 22.6% (20.0-50.0), LYM#: 1.85 × 10-9/L (1.10-3.20), EOS%: 11.1.% (0.4-8.0), EOS#: 0.97 × 10-9/L (0.02-0.50), NEUT%: 59.0% (50.0-70.0), NEUT#: 4.83 × 10-9/L (2.00-7.00) |
| IGG, RF | High levels of IgE, RF | |
| November 24, 2011 | IGG | IgG1: 7.670 g/L (4.900-11.400 ), IgG2: 3.540 g/L (1.500-6.400), IgG3: 0.103 g/L (0.200-1.100), IgG4: 8.650 g/L (0.020-2.000) |
| IGG, RF | High levels of serum IgE and RF | |
| July 5, 2012 | Blood routine examination | LYM%: 38.9% (20.0-50.0), LYM#: 3.99 × 10-9/L (1.10-3.20), EOS%: 1.6% (0.4-8.0), EOS#: 0.16 × 10-9/L (0.02-0.50), NEUT%: 51.8% (50.0-70.0), NEUT#: 5.32 × 10-9/L (2.00-7.00) |
| July 10, 2012 | MRI | Normal shapes of pituitary gland, lung and pancreas |
| April 3, 2018 | Blood routine examination | EOS%: 0.0% (0.4-8.0), EOS#: 0.00 × 10-9/L (0.02-0.50), LYM%: 15.0% (20.0-50.0), LYM#: 1.72 × 10-9/L (1.10-3.20), NEUT%: 82.6% (50.0-70.0), NEUT#: 9.44 × 10-9/L (2.00-7.00) |
| Urinalysis | Normal, Only the WBC count 26.3/uL (0.0-23.0 ) | |
| Biochemistry | UREA: 2.10 mmol/L (3.10-8.80), ALB: 36.10 g/L (40.00-55.00), AST: 43.6U/L (13.0-35.0), ALP: 43U/L (50-135), GGT: 5.1 U/L (7.0-45.0) | |
| IGG, Complement, RF | IgG: 25.10 g/L (7.00-16.00), IgA:1.51 g/L (0.70-4.00), IgM: 0.45 g/L (0.40-2.30g/l), C3: 0.56 g/L (0.90-1.80), C4: 0.088 g/L (0.100-0.400), RF: 356.00 IU/mL (0.00-19.00), IgG4: 23.300 g/L (0.020-2.000) | |
| CT | Severe interstitial lung lesions | |
| Bladder biopsy | Chronic inflammation | |
| May 7,2018 | IGG | IgG4: 5.280 g/L (0.020-2.000) |
| CT | Normal |
| Date | Serum osmotic pressure (270-300 mOsm/L) | Urine osmotic pressure (400-1200 mOsm/L) | Urine NAG enzyme (0-21 U/gCr) | ||||||
| September 24 | 289 mOsm/L | 62 mOsm/L | - | ||||||
| September 25 | 298 mOsm/L | 65 mOsm/L | 87.5 U/gCr | ||||||
| September 28 | 300 mOsm/L | 148 mOsm/L | 106.5 U/gCr | ||||||
| Serum prolactin (PRL) (µg/L) | |||||||||
| September 30 | Pre-stimulation with metoclopramide (10 mg) | Post-stimulation with metoclopramide (10 mg) | |||||||
| 15 min | 0 min | 15 min | 30 min | 60 min | 90 min | ||||
| 28.66 | 29.28 | 38.78 | 35.22 | 38.66 | 39.84 | ||||
| September 30 | Changes of serum hormone levels | ||||||||
| Testosterone | Estrogen | LH | PRL | FSH | Progestone | Cortisol | |||
| - | - | ↓ | ↑ | ↓ | - | 12:00 AM | 8:00 AM | ||
| - | - | ||||||||
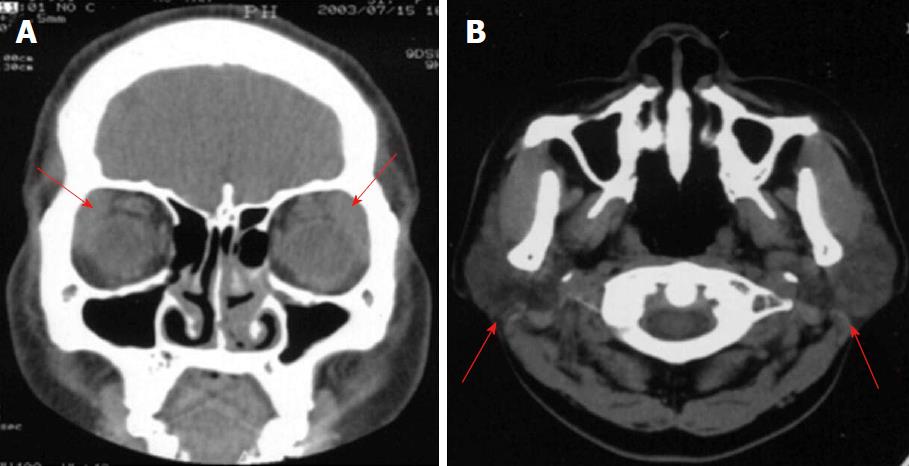
A 60-year-old woman who had no medical history was admitted because of the traumatic rib fracture to our hospital in November of 2011. She observed an ophthalmologist at a local hospital for left eyelid swelling with a feeling of sand in the eye without any known cause late in 1999. She was first diagnosed with “allergic rhinitis” and was externally treated with eye drops (an ointment) of dexamethasone and sodium chromate. However, no obvious efficacy was observed. The symptoms gradually worsened. Computed tomography (CT) showed an enlargement of double lacrimal glands (Figure 1A) and was treated as “non-specific, non-infective orbital inflammatory pseudotumor” by taking prednisone 60 mg/d, together with roxithromycin and eye drops. The efficacy was only observed at the beginning of the treatment. There was no obvious improvement observed. Follow up CT) 2 years late showed an enlargement of double lacrimal glands, and the pathological findings showed a double lacrimal lymphoid pseudotumor in surgical resections of the bilateral lacrimal glands and fat pads. Although the symptom of swelling of the eyelids was improved after the surgery, the dryness of the eyes, nasal cavity and mouth required the patient for a long-term application of artificial tears.
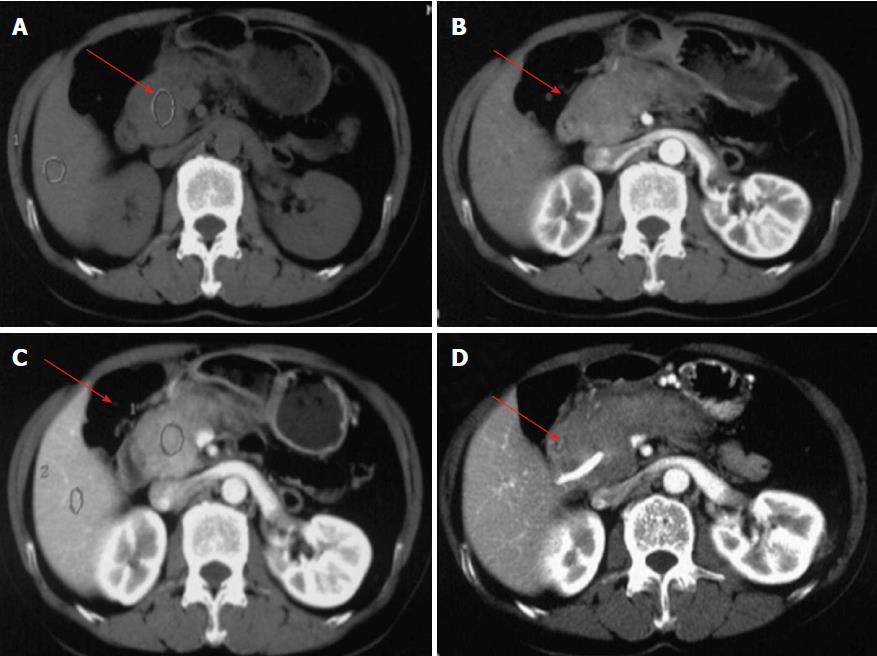
In May 2005, the patient had symptoms of repeated diffuse swelling of the parotid glands as diagnosed by CT (Figure 1B), but no treatment was undertaken until she was admitted to our hospital with repeated severe gastric pains in November of 2005. Abdominal CT showed an enlargement of the head of pancreas (Figure 2), and the blood routine examination showed a neutrophil count of LYM%: 50.9% (20.0-50.0), LYM#: 2.11 × 10-9/L (1.10-3.20), EOS%: 13.6% (0.4-8.0), EOS#: 0.78 × 10-9/L (0.02-0.50), NEUT%: 68.0% (50.0-70.0), NEUT#: 6.62 × 10-9/L (2.00-7.00) (Table 1). The endoscopic retrograde cholangiopancreatography (ERCP) further showed bile duct (biliary) stricture and biliary sludge, and thus, severe acute cholestasis pancreatitis was diagnosed. The patient underwent bile duct dredging and a biliary stent implantation. However the patient was re-admitted to hospital because of severe abdominal pains, along with complications of fever, and obvious swelling of the left parotid gland and both sides of the submandibular glands four month late. A second ERCP showed no obvious tumor signs. Thus, an additional two biliary stents were implanted. The pathology of labial gland biopsy showed lymphoplasmacytic infiltration into the focal lobules of the salivary gland tissue beneath the squamous mucous epithelia, with low level of serum complement C3, positive HEp2-ANA 1:100 (< 1;100), but negative ENA-AbSSA: negative, ENA-AbSS (Table 1). Therefore, Sjogren’s syndrome was considered. A pulse therapy of a combination of steroid and gamma globulin with 200 mg, 500 mg, 500 mg of methylprednisolone, respectively, and 20 g of gamma globulin was performed for three consecutive days. In addition, she was prescribed oral prednisone, hydroxychloroquine sulfate, total glucosides of paeony and methotrexate until her symptoms were significantly relieved. The above oral medicines were then gradually tapered after her clinical condition had improved. Together with the efficacy of steroid treatments, CT, laboratory results and symptoms, she was finally diagnosed with Sjogren’s syndrome with AIP. A six-month follow-up demonstrated a stable condition, and CT showed no enlargement of the head of pancreas, and therefore, a third ERCP was performed to remove the three implanted biliary stents.
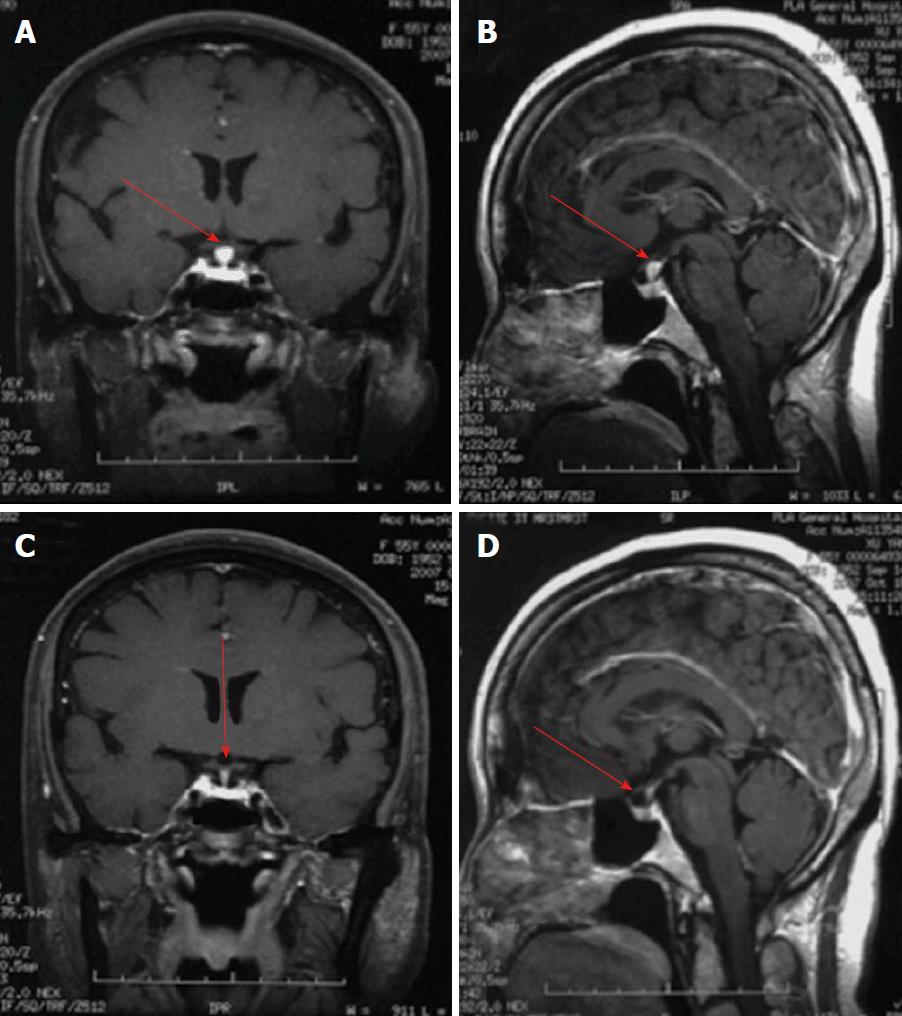
However, she was re-admitted to hospital because of symptoms of polydipsia and polyuria, accompanied with fatigue and weight loss in August 2007. Remarkably, she could drink water as much as 11000 mL/d and urinate as much as 10400 mL/d. Magnetic resonance imaging (MRI) showed pituitary stalk nodular thickening (Figure 3). Endocrinal examinations revealed an increased concentration of N-acetyl-β-D-glucosaminidase (NAG) and serum follicle stimulating hormone (FSH), with a decreased level of serum luteinizing hormone (LH) and prolactin (PRL) (Table 2). However, the renal examination suggested normal renal function. She was considered to have lymphocytic hypophysitis and diabetes insipidus and was given methylprednisolone pulse therapy for 12 d (600 mg × 3 d, 400 mg × 3 d, 200 mg × 3 d, 100 mg × 3 d), and oral desmopressin acetate tablets (Minirin®). Afterward, the patient was given oral prednisone 60 mg/d and gradually tapered. The above clinical conditions were significantly improved. Unexpectedly, the patient revisited the hospital with right lung infection in May 2008. The condition improved after an antibiotics treatment but showed symptoms of polydipsia and polyuria. The cranial brain MRI examination showed pituitary stalk thickening. She was given 500 mg of methylprednisolone pulse therapy for 3 d, and continuously took oral leflunomide, prednisone, hydroxychloroquine sulfate, total elixir (Pavulin), desmopressin acetate tablets and calcium supplements until her condition was improved. The oral prednisone was taken and gradually tapered as she was discharged from the hospital. The patient continued to take a low dose of prednisone (5.0 mg/d) and her condition was stable.
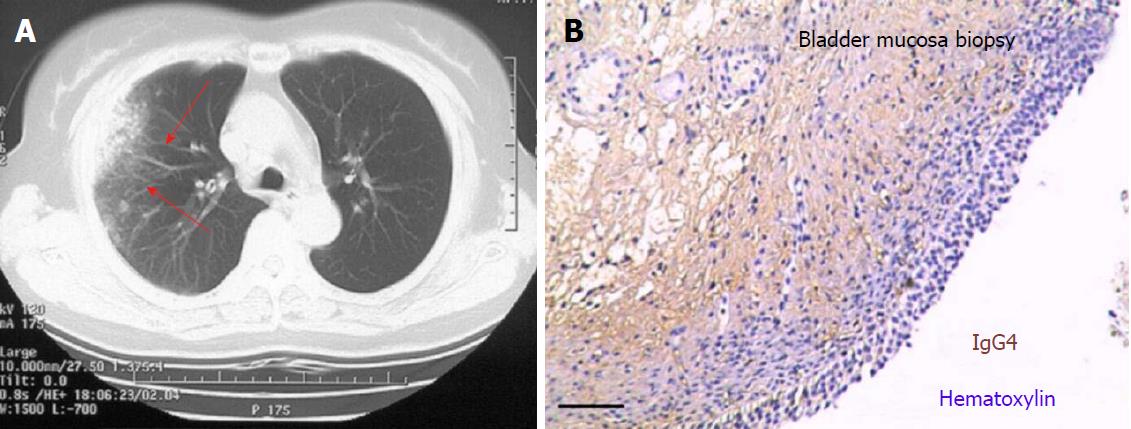
Of note, follow-up CT and MRI examinations revealed that the enlargement of the head of the pancreas was not significantly improved with low signal intensity on T2WI and T1WI in 2009, although the head of pancreas became normal as evaluated by abdominal CT when she was re-admitted to the hospital with nasal congestion with coughing and chest pain (but without fever and chilling) in November 2011 (Table 1). Chest CT showed right lung infection and interstitial lung lesions (Figure 4A). Antibiotic therapy did not improve her clinical conditions. Bone scan showed a rib fracture; blood tests demonstrated high neutrophil and eosinophilic cell counts and high levels of serum IgE and rheumatic factor (RF); IgG examination further revealed strikingly higher levels of serum IgG4 at 8.65 g/L compared to the normal range of 0.02 g/L-2.00 g/L (Table 1). The patient was thus diagnosed as IgG4-RD suspicious. The patient was then given pulse therapy by intravenously infusion with 200 mg of methylprednisolone and 20 g of gamma globulin for 3 d, combined with intravenous injection of 10 mg of incadronate disodium for anti-osteoporosis therapy. She was discharged from the hospital after her condition had improved. During 2012 to 2014, she was given steroids and immunosuppressants as maintenance therapy.
In May 2015, the patient was re-admitted to the hospital because of double traumatic rib fractures, along with complications of cough. She was diagnosed as with an IgG4-RD relapse, chronic obstructive pulmonary disease, diabetes mellitus type II, severe osteoporosis, rib fracture, cervical degeneration and lumbar disc herniation. The patient was treated with methylprednisolone 16 mg/d, lefluramide 20 mg/d and hydroxychloroquine 0.2 g/d to control the primary disease, and other agents for osteoporosis treatment for one month. She was stable for one year before being considered as the relapse of IgG4-RD. The treatment of orally giving methylprednisolone 4.0 mg/d, lefluramide 20 mg/d, hydroxychloroquine 0.2 g/d and thymopentin on a routine base, along with anti-infective, anti-diabetic agents and a calcium supplement, was effective.
Most recently, the patient was re-admitted to the hospital because of symptoms of polydipsia and polyuria, burning and pain in April 2018. The serum IgG examination further revealed a strikingly higher level of serum IgG4 at 23.3 g/L, urine tests showed a high number of white blood cell (WBC) counts, and chest CT showed severe interstitial lung lesions. A bladder biopsy showed chronic inflammation with IgG4-positive infiltration (Figure 4B). The patient was given oral prednisolone 60 mg/d, iguratimod 50 mg/d and antibiotic therapy for three weeks. One month later, the serum concentration of IgG4 was decreased to 5.28 g/IgG (Table 1), Chest CT also showed a normal lung image. The condition of this patient is currently stable with a maintenance steroid therapy.
IgG consists of four subclasses, and among them IgG4 is the least abundant subclass in the serum with an average concentration of 0.30-0.465 g/L[6]. Functionally, IgG4 can react with hapten exchanges owing to its special structure and function in biochemistry. Chemically, disulfide bonds between IgG4 heavy chains are not stable, leading to the heavy chain separating and recombining randomly. Therefore, IgG4 is theoretically incapable of effectively activating the immune effector cell and classical pathway of complements. However, the immune imbalance and autoantibody induced by allergen exposure may trigger IgG4-RD[7]. In this regard, IgG4 can enhance Th2 and Treg-mediated immunoreactions[8]. The Th2 cell-produced IL-4/IL-13 can in turn convert B cells to produce IgG4 and IgE, and the IL-10 produced by Th2 and Treg cells also tends to transform IgG4[9]. In addition, the repeated allergen exposure also enhances Th2 reactions that results in the clearance of plentiful B cells from IgE conversion. B cells survive after IgG4 conversion, TGF-β from Treg-facilitated fibrosis. These processes may contribute to pathological manifestations of special IgG4-RD to some extent. In this context, IgG4-RD can be involved in multiple organs, without a specific clinical symptom in the early stages of this disease. Therefore, an early diagnosis of IgG4-RD has an important clinical significance. However, the broad spectrum of clinical manifestations of IgG4-RD in different organs, i.e., each organ may demonstrate special manifestations, and present various clinical symptoms, may cause misdiagnosis and prevent early diagnosis of this disease.
Clinically, an early diagnosis of IgG4-RD remains a challenge, owing to its symptoms and pathology mimicking several other diseases such as infections and malignancies, even if the IgG4-RD diagnostic criteria are followed[10]. For example, clinically, IgG4-RD often presents with multifocal tumor-like masses that leads to confusions with malignancy. In the present report, we present a female patient who suffered from progressive IgG4-RD in multi-organs for nineteen years (1999-2018), before and after her IgG4-RD was confirmed. Obviously, in addition to the typical pancreas involvement (AIP), the patient was affected in other organs including the eye orbit, lacrimal gland, parotid gland, pituitary and lung. Although the main complaint was gastric pain with yellow jaundice in this case, progressive disorders of other involved organs occurred.
IgG4-RD is considered to be a rare disorder, but it is often overlooked and misdiagnosed. It may take several years before the diagnosis is made. From the diagnostic standpoint, although it may be difficult to establish a diagnostic criteria covering all IgG4-RD, the “Japanese Research Committee of IgG4-RD” proposed the comprehensive diagnostic criteria (CDC) for IgG4-RD in 2011[11]. These criteria included: (1) one or more organs experience diffuse/focal swelling; (2) serum IgG4 > 135 mg /dL; (3) the histological pattern of lesions is fibro-inflammatory, with a lymphoplasmocytic infiltration of IgG4-positive plasma cells and storiform pattern of fibrosis, and the ratio of IgG4/IgG-positive plasma cell is above 40% in tissues; and (4) immunohistochemistry showed more than 10 IgG4-positive plasma cells per high powered field (HPF). A patient who conforms to all above four criteria can be diagnosed as IgG4-RD, those who conform to three of above four criteria can be diagnosed as IgG4-RD probable, and any who conform to the above two of above four criteria can be diagnosed as IgG4-RD suspicious[4,12,13]. In the same year at the “IgG4-RD” international conference held in the United States, researchers reached a consensus that the diagnosis of IgG4-RD should primarily rely on pathological features rather than IgG-positive plasma cell count and ratio, although they are an essential condition of diagnosis[14]. In this case, the patient at least fulfills two of above criteria: (1) one or more organs experience diffuse/focal swelling; and (2) serum IgG4 > 135 mg /dL, and therefore was diagnosis as diagnosed as IgG4-RD suspicious.
This patient was very responsive to steroid and immunosuppressant therapies, but the patient reported in this case was misdiagnosed as a single involved organ disorder many times, highlighting the importance of systemic and comprehensive evaluation of symptoms, CT and MRI imaging results, laboratory data and histology of biopsies in the diagnosis of IgG4-RD. Unfortunately, a determination of infiltrated IgG4-positive plasma cells was not performed in biopsies of involved organs of this patient. In addition, the overlooking concentration of serum IgG4 was another main reason to delay the clinical diagnosis of IgG4-RD in this case.
In conclusion, IgG4-RD is a complicated clinical syndrome that is currently short of diagnostic criteria, and is easy to be misdiagnosed. The present case is a typical IgG4-RD in a woman with progressive multiple organ involvement, including lacrimal glands, parotid glands, pancreas, lungs and pituitary during the long course of the disease progression. From therapeutic standpoint, patients with IgG4-RD respond well to steroid therapy, and/or immunosuppressive agents resulted in a significant remission of disease and improved patient conditions. However, the disease can easily recur after the steroid is reduced or withdrawn.
Importantly, adverse effects of severe clinical complications such as osteoporotic fractures and infections were observed in this patient during the long-term steroid therapy. Therefore, it is critical to give pulse therapy with high doses of steroid in combination with immunosuppressive agents during the active disease period of the disease in clinical settings, which may avoid disease recurrence during the reduction of the steroid. Equally noteworthy, in addition to clinical symptoms, concentrations of serum IgG4, IgE, ESR, CRP and other laboratory results may allow us to identify disease activity early. An early identification of disease activity may allow us to adjust the treatment regimen and avoid severe complications caused by an overdose of steroid treatment. From a diagnostic standpoint, the early disease symptoms are generally mild with an involvement of one or two organs for a long time period, before it gradually develops to involve multiple organs with life-threatening complications. Thus, this case emphasizes a clinical importance in the early diagnosis and interventions for IgG4-RD. In this regard, patients with a clinically unclear cause of inflammation, swelling and refractory glands (such as the lacrimal gland, parotid gland and thyroid), rhinitis, pancreatitis, hypophysitis, and/or interstitial pneumonia should be considered as to the possibility of IgG4-RD and recommended for the plasma IgG4 test, which may provide important diagnostic data and clues for this disease, although the immunohistological examination is required for confirmation.
A sixty-seven-year-old female presented with a progressive multi-organ involvement of IgG4-related disease (IgG4-RD) for over 19 years.
As a disorder with multiple organ involvement, IgG4-RD presents no specifically clinical manifestation for an early diagnosis, and the diagnosis largely relies on a combination of clinical manifestation, histology, imaging, and serology.
IgG4-RD has a broad spectrum of clinical manifestations and it is important to differentially diagnosis it from various diseases of the involved organs, such as Mikuri’s disease, autoimmune pancreatitis, interstitial pneumonia and retroperitoneal fibrosis.
A significantly increased serum IgG4 level (> 1350 mg/L) is a signal for serological diagnosis in IgG4-RD.
Computed tomography, magnetic resonance imaging or endoscopic retrograde cholangiopancreatography imaging showed a swollen feature or tumor-like structure in the involved organs.
IgG4-positive lymphocyte infiltration and sclerosis in the involved organs.
The patient was given methylprednisolone 200 mg/d pulse therapy for 3 d, a large dose of gamma globulin (20 g/d) intravenous infusion for 3 d and taking oral prednisolone 30 mg/d for three weeks. The prednisolone was then gradually tapered.
Patients with a clinically unclear cause of inflammation, swelling and refractory glands (such as the lacrimal gland, parotid gland and thyroid), rhinitis, pancreatitis, hypophysitis, and/or interstitial pneumonia should be considered for the possibility of IgG4-RD and recommended for plasma IgG4 test.
IgG4-RD is a systemic and clinical entity with autoimmune pathogenesis, which is characterized by high levels of circulating IgG4 and a dramatic response to steroid therapy.
Since the clinical manifestations of IgG4-RD are commonly similar to features of other diseases, it is easily misdiagnosed and improperly treated. This case emphasizes a clinical importance of the early diagnosis and interventions for IgG4-RD. From a diagnostic standpoint, the early disease symptoms are generally mild with an involvement of one or two organs for a long time before they gradually develop into multiple organ involvements with life-threatening complications. Apart from clinical symptoms, concentrations of serum IgG4, IgE, ESR, CRP and other laboratory results may provide important diagnostic data and clues for early identity disease activities. From a therapeutic standpoint, patients with IgG4-RD respond well to steroid therapy, and/or immunosuppressive agents resulting in a significant remission of disease and improved patient conditions. Notably, the disease can easily recur after the steroid is reduced or withdrawn. To reduce the adverse effects of long-term steroid therapy, it is critical to give pulse therapy with high doses of steroids in combination with immunosuppressive agents during the active disease period of the disease in clinical settings.
The authors cordially thank the patient for her acceptance to publish her personal medical data and all members participated in the diagnosis and treatment of this case in the General Hospital at Ningxia Medical University, China.
CARE Checklist (2013) statement: The authors have read the CARE Checklist (2013), and the manuscript was prepared and revised according to the CARE Checklist (2013).
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Ferrante A, Kai K, Rosales C S- Editor: Ji FF L- Editor: A E- Editor: Tan WW
| 1. | Umehara H, Okazaki K, Nakamura T, Satoh-Nakamura T, Nakajima A, Kawano M, Mimori T, Chiba T. Current approach to the diagnosis of IgG4-related disease - Combination of comprehensive diagnostic and organ-specific criteria. Mod Rheumatol. 2017;27:381-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 152] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 2. | Aithal GP, Breslin NP, Gumustop B. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med. 2001;345:147-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2026] [Cited by in RCA: 1878] [Article Influence: 78.3] [Reference Citation Analysis (0)] |
| 3. | Yoshida K, Toki F, Takeuchi T, Watanabe S, Shiratori K, Hayashi N. Chronic pancreatitis caused by an autoimmune abnormality. Proposal of the concept of autoimmune pancreatitis. Dig Dis Sci. 1995;40:1561-1568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1044] [Cited by in RCA: 925] [Article Influence: 30.8] [Reference Citation Analysis (0)] |
| 4. | Kamisawa T, Okazaki K, Kawa S, Ito T, Inui K, Irie H, Nishino T, Notohara K, Nishimori I, Tanaka S. Amendment of the Japanese Consensus Guidelines for Autoimmune Pancreatitis, 2013 III. Treatment and prognosis of autoimmune pancreatitis. J Gastroenterol. 2014;49:961-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 148] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 5. | Xiao X, Lian M, Zhang W, Eric Gershwin M, Ma X. The Immunologic Paradoxes of IgG4-Related Disease. Clin Rev Allergy Immunol. 2018;54:344-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Rungsakulkij N, Sornmayura P, Tannaphai P. Isolated IgG4-related sclerosing cholangitis misdiagnosed as malignancy in an area with endemic cholangiocarcinoma: a case report. BMC Surg. 2017;17:17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Celis IM, Kriekaart RL, Aliredjo RP, van Lochem EG, van der Vorst MJ, Hassing R. IgG4-related disease: a disease we probably often overlook. Neth J Med. 2017;75:27-31. [PubMed] |
| 8. | Zen Y, Fujii T, Harada K, Kawano M, Yamada K, Takahira M, Nakanuma Y. Th2 and regulatory immune reactions are increased in immunoglobin G4-related sclerosing pancreatitis and cholangitis. Hepatology. 2007;45:1538-1546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 526] [Cited by in RCA: 481] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 9. | Robinson DS, Larché M, Durham SR. Tregs and allergic disease. J Clin Invest. 2004;114:1389-1397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 204] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 10. | Xiao J, Li G, Yang G, Jia C, Li B. Case report: A female case of isolated IgG4-related sclerosing cholangitis mimicking cholangiocarcinoma. Medicine (Baltimore). 2017;96:e6542. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Okazaki K, Umehara H. Are Classification Criteria for IgG4-RD Now Possible? The Concept of IgG4-Related Disease and Proposal of Comprehensive Diagnostic Criteria in Japan. Int J Rheumatol. 2012;2012:357071. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 103] [Cited by in RCA: 98] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 12. | Kawano M, Saeki T, Nakashima H, Nishi S, Yamaguchi Y, Hisano S, Yamanaka N, Inoue D, Yamamoto M, Takahashi H. Proposal for diagnostic criteria for IgG4-related kidney disease. Clin Exp Nephrol. 2011;15:615-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 290] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 13. | Matsuda K, Saito A, Takeuchi Y, Fukami H, Sato H, Nagasawa T. IgG4-Related Disease Manifesting as Interstitial Nephritis Accompanied by Hypophysitis. Am J Case Rep. 2017;18:593-598. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Mikumo H, Hamada N, Harada E, Yanagihara T, Ogata S, Yabuuchi H, Ijichi K, Takayama K, Nakanishi Y. A case of immunoglobulin G4-related respiratory disease with multiple lung cysts: A case report. Respir Med Case Rep. 2017;21:89-92. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |