Published online Dec 16, 2016. doi: 10.12998/wjcc.v4.i12.409
Peer-review started: February 24, 2016
First decision: April 26, 2016
Revised: April 29, 2016
Accepted: June 1, 2016
Article in press: June 3, 2016
Published online: December 16, 2016
Processing time: 288 Days and 11.4 Hours
Granulomatous lobular mastitis is a rare inflammatory disease of the breast of unknown etiology. Most present as breast masses in women of child-bearing age. A 29-year-old female presented with a swollen, firm and tender right breast, initially misdiagnosed as mastitis. Core needle biopsy revealed findings consistent with granulomatous lobular mastitis, and cultures were all negative for an infectious etiology. She was started on steroid therapy to which she initially responded well. A few weeks later she deteriorated and was found to have multiple breast abscesses. She underwent operative drainage and cultures grew Mycobacterium fortuitum. Granulomatous lobular mastitis is a rare inflammatory disease of the breast. The definitive diagnose entails a biopsy. Other causes of chronic or granulomatous mastitis should be ruled out, including atypical or rare bacteria such as Mycobacterium fortuitum. This is the first reported case of granulomatous mastitis secondary to Mycobacterium fortuitum. With pathologic confirmation of granulomatous mastitis, an infectious etiology must be ruled out. Atypical bacteria such as Mycobacterium fortuitum may not readily grow on cultures, as with our case. Medical management is appropriate, with surgical excision reserved for refractory cases or for drainage of abscesses.
Core tip: Granulomatous mastitis is a rare inflammatory disease of the breast, that often presents as a breast mass. The exact etiology is unkown. We report a rare presentation of this conditions arising in the right breast of a 29-year-old female. The treatment if granulomatous mastitis is yet to be defined, but literature supports non operative management with steroids, with surgery reserved for failure of medical management. Failure of steroid therapy should raise the suspicion of an underlying misdiagnosed infectious etiology. If an infectious etiology is identified however, medical management with antibiotics remains the mainstay for treatment.
- Citation: Kamyab A. Granulomatous lobular mastitis secondary to Mycobacterium fortuitum. World J Clin Cases 2016; 4(12): 409-412
- URL: https://www.wjgnet.com/2307-8960/full/v4/i12/409.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v4.i12.409
Granulomatous lobular mastitis is a rare inflammatory disease of the breast[1]. Although it was first described in 1972[2] and has been a recognized disease for over 40 years, it remains an overall rare entity. The exact etiology remains unknown. The clinical presentation is often similar to that of breast cancer[1], with a unilateral breast mass being most common[2]. Pathologic findings include non-necrotizing granulomatous inflammation of the lobules[1,2].
Treatment is based on the suspected etiology. For idiopathic granulomatous mastitis, excision has been proposed by some[3], whereas medical management with repeated courses of steroid therapy has been proposed by others[1]. Published cases reveal opposing outcomes to different treatment algorithms and modalities. The optimal treatment of granulomatous lobular mastitis therefore remains complex and there is currently no standard of care for its management. In cases where an infection has been identified, the standard treatment remains antibiotic therapy.
We report the case of a 29-year-old female eleven months postpartum, no longer breast feeding, who presented to her primary care provider with the complaint of a swollen and tender right breast, with a large area of firmness. She had no personal or family history of breast cancer, had no previous breast masses or biopsies, no previous breast surgeries, and had no history of chest radiation. Due to the degree of swelling and tenderness, a presumptive diagnosis of an infectious mastitis was made and the patient was prescribed a course of antibiotics. She subsequently failed to improve and was referred for a surgical evaluation.
On examination she was found to have a visibly swollen right breast, tender to touch, and with a large approximately 10 by 10 cm firm mass in the superior and outer portion of the breast. An ultrasound was performed to rule out abscess formation or fluid collection as well as to further characterize the mass (Figure 1), which revealed a large irregular hypoechoic mass without any evidence of abscess or fluid collection.
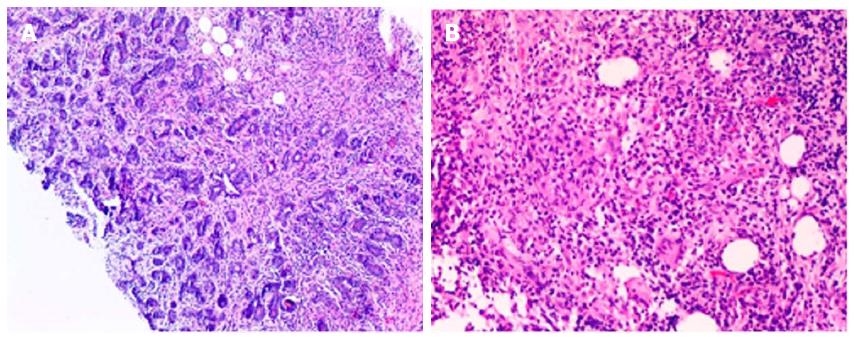
A core-needle biopsy was therefore performed to rule out breast cancer, as well as for cultures to definitively rule out an infectious mastitis. Cultures at this time were negative for bacterial, fungal, acid fast staining, or mycobacterial growth. Histologic evaluation of the biopsy revealed granulomatous inflammatory reaction centered on lobules, with granulomas composed of epithelioid histiocytes, Landerhans giant cells accompanied by lymphocytes, plasma cells and occasional eosinophils (Figure 2), consistent with granulomatous lobular mastitis.
The patient was given a course of oral steroids starting with an initial Prednisone dose of 60 mg/d and tapering thereafter, and given a period of observation. Her condition began to improve after 2 wk on steroids, and on a 1-mo follow-up she remained free of any symptoms.
She then presented approximately 3 wk later with recurrent redness and tenderness of the right breast. A repeat ultrasound in the office revealed multiple fluid collections within the breast. A diagnostic needle aspiration of one of the fluid collections was performed and revealed purulent fluid consistent with abscesses. The collections were therefore all aspirated and the patient given repeat antibiotics and observed. Cultures of this purulent fluid were once again all negative for any bacterial growth or for acid fast staining.
Her condition continued to deteriorate and the abscesses enlarged and increase in number. She therefore underwent operative incision and drainage of her multiple abscesses, as well as a third set of bacterial cultures. This time, the cultures grew Mycobacterium fortuitum. She was referred to an infectious disease specialist for treatment, and was prescribed a long term course of multiple antibiotics, consisting of Ciprofloxacin, Linezolid, and Sulfamethoxazole/Trimethoprim as per their recommendations for the treatment of her Mycobacterium fortuitum causing granulomatous mastitis.
Granulomatous lobular mastitis is a rare and benign inflammatory disease of the breast first described in 1972[2]. The clinical findings and presentation is often reported as mimicking that of breast cancer[1], however in our case it initially resembled an infectious mastitis.
Most published cases of granulomatous mastitis in the literature have no identifiable causative bacteria, and the etiology therefore remains unclear. An autoimmune etiology has proposed[4] however no specific antibodies have been recognized. In published cases, it typically affects women of child bearing age[1,5], and it has no propensity to favor the right or left breast[5].
As with the workup of any other breast mass, the physician must remain vigilant and ruling out cancer remains the utmost priority. Mammographic findings are non-specific, yet ultrasound identifies a hypoechoic mass in the majority of cases[1], including ours. The definitive diagnose entails a biopsy. Core-needle is favored over fine-needle aspiration since it carries a higher diagnostic yield. Surgical excision or open biopsy is not required for diagnosis.
Pathologically, it is characterized by non-necrotizing lobular granulomatous inflammation[5], originating in the breast lobules[1]. Certain pathologic features can overlap with other breast conditions, and therefore other causes of chronic or granulomatous mastitis should be ruled out, such as sarcoidosis, fungal infections, and Wegener’s granulomatosis[1,4].
There is no definitive consensus on the appropriate treatment for granulomatous mastitis. Once an infectious etiology has been ruled out, a course of steroid therapy appears to be appropriate in most studies. Satisfactory results have been published with an initial dose of Prednisone at 60 mg/d[1]. In a recent study reviewing 50 female patients with granulomatous mastitis, steroid therapy was not found to be effective, and many patients ultimately required surgical excision either due to failed treatment or abscess collection after steroid treatment[6]. We suspect in such cases of failure of steroid treatment, that an underlying infection was pre-existent despite negative cultures, as was the case with our patient.
Mycobacterium fortuitum is a rapidly growing group of nontuberculous mycobacteria more common in patients with genetic or acquired causes of immune deficiency[7]. It is commonly associated with surgical procedures, and is known to infect implanted medical devices, cause injection site abscesses, and also seen with breast implants[7]. There have been previously reported cases of breast abscesses secondary to Mycobacterium fortuitum, but this is the first reported case of a granulomatous mastitis secondary to Mycobacterium fortuitum, in an immunocompetent patient without foreign body in her breast.
A granulomatous response is a known protective immune response against Mycobacterial infections[8]. We suspect that in many of the previously reported cases of granulomatous mastitis, especially in those in whom steroid therapy had failed, that an underlying atypical bacterium was the cause. In our case, two different sets of tissue cultures, including Mycobacterial cultures and acid-fast staining, had failed to grow Mycobacterium fortuitum, further demonstrating how inconspicuous such an infection can be.
Such a variety in outcomes of published cases further outlines the complexity of granulomatous lobular mastitis. The proper treatment should be chosen on a case-by-case basis[6], but ruling out a neoplastic and infectious etiology are of utmost importance. Failure of steroid treatment should raise the suspicion of a misdiagnosed underlying pathogen.
Dr. Jami R Skrade, MD and Dr. Kyle Noskoiviak, MD, Pathologists, CoxHealth, Springfield, MO, for the pathologic findings on histology, as well as the histologic picture.
A 29-year-old woman with no significant medical history presented with a painless left breast mass.
Right breast swelling and redness in the upper outer portion of the right breast.
Infectious mastitis, inflammatory breast cancer, granulomatous mastitis.
All labs were within normal limits.
Ultrasound showed a large irregular hypoechoic mass without any evidence of abscess or fluid collection.
Granulomatous inflammatory reaction centered on lobules, with granulomas composed of epithelioid histiocytes, Landerhans giant cells accompanied by lymphocytes, plasma cells and occasional eosinophils, consistent with granulomatous lobular mastitis.
Oral steroid therapy.
Granulomatous lobular mastitis is a rare and benign inflammatory disease of the breast. The etiology remains unclear. An autoimmune etiology has proposed, however no specific antibodies have been recognized.
Granulomatous mastitis is a benign inflammatory disease of the breast.
This entity is commonly confused with an infectious mastitis or inflammatory breast cancer. Ruling out cancer is of utmost importance in any breast mass. There is no definitive consensus on the appropriate treatment. Most studies however favor medical management over surgical excision.
The authors report a rare breast granulomatous lobular mastitis in a young woman. This paper is valuable due to a rarity of this disease. This manuscript provides useful information to the medical students, clinicians, and researchers in this field.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Song J, Sonoda K, Zhang XQ S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Hovanessian Larsen LJ, Peyvandi B, Klipfel N, Grant E, Iyengar G. Granulomatous lobular mastitis: imaging, diagnosis, and treatment. AJR Am J Roentgenol. 2009;193:574-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 161] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 2. | Kessler E, Wolloch Y. Granulomatous mastitis: a lesion clinically simulating carcinoma. Am J Clin Pathol. 1972;58:642-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 393] [Cited by in RCA: 444] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 3. | Miliauskas JR, Pieterse AS, Williams RS. Granulomatous lobular mastitis. Aust N Z J Surg. 1995;65:139-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Imoto S, Kitaya T, Kodama T, Hasebe T, Mukai K. Idiopathic granulomatous mastitis: case report and review of the literature. Jpn J Clin Oncol. 1997;27:274-277. [PubMed] |
| 5. | Going JJ, Anderson TJ, Wilkinson S, Chetty U. Granulomatous lobular mastitis. J Clin Pathol. 1987;40:535-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 120] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 6. | Hur SM, Cho DH, Lee SK, Choi MY, Bae SY, Koo MY, Kim S, Choe JH, Kim JH, Kim JS. Experience of treatment of patients with granulomatous lobular mastitis. J Korean Surg Soc. 2013;85:1-6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 7. | Betal D, Macneill FA. Chronic breast abscess due to Mycobacterium fortuitum: a case report. J Med Case Rep. 2011;5:188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Co DO, Hogan LH, Kim SI, Sandor M. Mycobacterial granulomas: keys to a long-lasting host-pathogen relationship. Clin Immunol. 2004;113:130-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 69] [Article Influence: 3.3] [Reference Citation Analysis (0)] |