Published online Dec 16, 2016. doi: 10.12998/wjcc.v4.i12.385
Peer-review started: March 14, 2016
First decision: April 20, 2016
Revised: October 9, 2016
Accepted: October 22, 2016
Article in press: October 24, 2016
Published online: December 16, 2016
Processing time: 268 Days and 23.8 Hours
The primary splenic lymphoma is extremely uncommon, can present with grave complications like hypersplenism and splenic rupture. In view of vague clinical presentation, it is difficult to arrive at the diagnosis. In such circumstances, histopathological diagnosis is very important. A precise diagnosis can only be made on histopathology and confirmed on immunohistochemistry.Emergency splenectomy is preferred as an effective therapeutic and diagnostic tool in cases with giant splenomegaly. Core biopsy is usually not advised due to a high risk of post-core biopsy complications in view of its high vascularity and fragility. Aim behind highlighting the topic is to specify that core biopsy/ fine needle aspiration cytology can be used as an effective diagnostic tool to arrive at correct diagnosis to prevent untoward complications related to disease and treatment. Anticoagulation therapy is vital after splenectomy to avoid portal splenic vein thrombosis.
Core tip: Primary splenic lymphoma is a rare entity, has vague clinical presentation and can present with grave complications like hypersplenism and splenic rupture. In such circumstances, core biopsy/fine needle aspiration cytology can hit the correct pathological diagnosis. Emergency splenectomy is an effective therapeutic and diagnostic tool in cases with massive splenomegaly with features of hypersplenism.
- Citation: Ingle SB, Hinge (Ingle) CR. Primary splenic lymphoma: Current diagnostic trends. World J Clin Cases 2016; 4(12): 385-389
- URL: https://www.wjgnet.com/2307-8960/full/v4/i12/385.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v4.i12.385
Primary splenic lymphoma (PSL) is very unusual entities if strict diagnostic criteria are applied[1]. As per previous studies the final diagnosis of PSL should be made only when the disease is limited to spleen or involving hilar lymph nodes without any recurrence after splenectomy[1-4]. In patients with PSL, therapeutic splenectomy is to be done. However, presently ultrasound guided core biopsy is a safe and efficient diagnostic investigation, can be used routinely. Therapeutic splenectomy is to be followed by anticoagulation therapy and chemotherapy[5].
PSL is a rare neoplasm of the spleen, probably comprising less than 2% of all the lymphomas[6,7] and 1% of all the non-Hodgkin’s lymphomas[2,8-10].
There are two main types: (1) splenic lymphoma with circulating villous lymphocytes[6]; and (2) marginal zone splenic lymphoma originating from a peculiar splenic B-cell structure separated by the mantle zone.
Clinical presentations of nonspecific symptoms are weight loss, weakness, fever, and lower upper quadrant pain or discomfort due to enlarged spleen.
Clinical presentations of specific symptoms are mainly due to invasion of lymphoma cells in to adjacent organs stomach, pancreas, diaphragm, colon, or mesentery[11-16].
Cytopaenia can also be a presenting feature[7]. The complete blood count and peripheral smear (PS) findings are mostly unremarkable[17]. Elevation of ESR may be noted[7].
PSL presenting as splenic abscess although uncommon, is associated with high morbidity and death rates due to delayed diagnosis and management[18]. Due to vague presentation, the clinical diagnosis is difficult[19]. Splenic lymphomas usually present as space occupying solid lesions and when present as splenic abscesses are usually encountered in patients with underlying disorders, including infections, emboli, trauma, recent surgery, malignant hematologic conditions and immunosuppression[20].
The nonspecific clinical presentation of PSL creates the real diagnostic dilemma.
Dasgupta et al[1] reported that Lymphoma restricted to the spleen and hilar lymph nodes. Further confirmed following a 6-mo relapse-free period following splenectomy. Skarin et al[21] reported that lymphoma with splenic involvement in which splenomegaly is the dominant feature. Dachman et al[14] reported that splenic lesions with hypodensity on contrast enhanced Computed tomography scans or lesions with hypoechogenecity on ultrasound (USG) studies. Ahmann et al[11] reported that stage I refers to disease confined to the spleen; Stage II refers to splenic involvement along with hilar lymph nodes; Stage III refers to extra-splenic nodal or hepatic involvement.
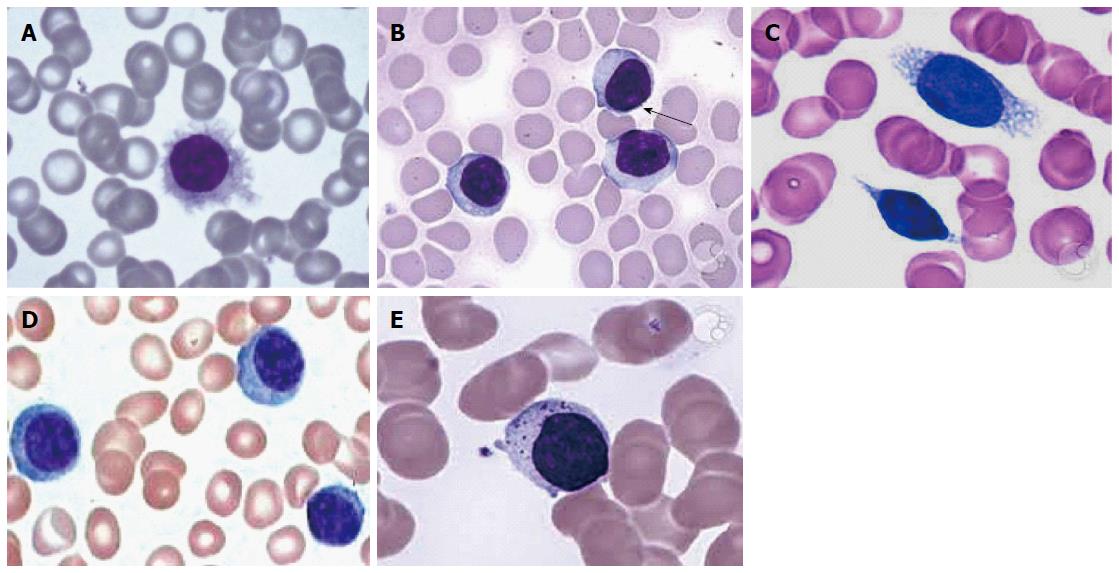
Most of the patients we can reveal neoplastic lymphoid cells on peripheral blood smear, i.e., hairy cells, prolymphocytes, villous lymphocytes, basophilic villous lymphocytes, etc., which may raise the suspicion of neoplastic lymphoid disease in the mind of pathologist (Figure 1).
Core biopsy/fine needle aspiration cytology (FNAC) are traditionally not recommended in view of high fragility of splenic tissue leading to hemorrhagic complications. However, currently it can be used as a routine diagnostic test[22].
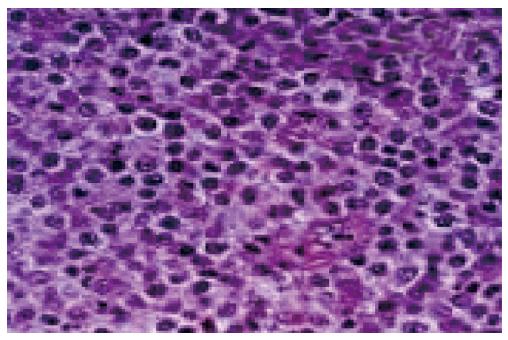
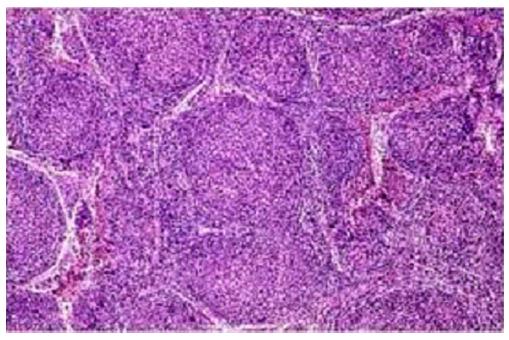
In diffuse large B cell lymphoma: Microscopy predominantly shows monotonous population of large neoplastic lymphoid cells with large areas of necrosis[5].The individual cells essentially demonstrated a large atypical nucleus, irregular nuclear borders with vesicular chromatin and prominent nuclei. Histopathological examination reported as Non-Hodgkin’s Lymphoma of diffuse large B cell phenotype[5] (Figure 2).
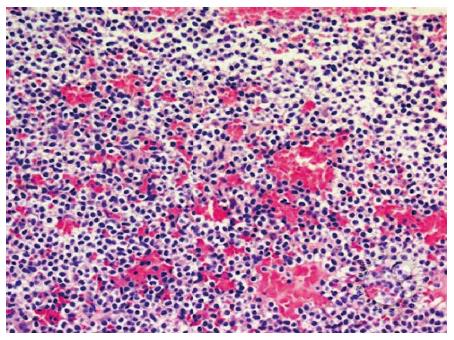
Hairy cell leukemia: Shows the small to medium sized lymphocytic infiltrate more clearly. Round to kidney-shaped with abundant clear cytoplasm are usually revealed (Figure 3).
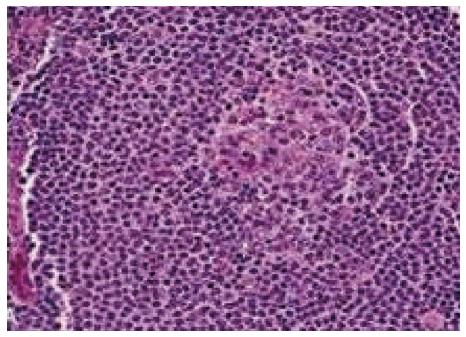
Marginal zone splenic lymphoma: Splenic white pulp reactive germinal centres show small neoplastic lymphoid cells almost replacing the mantle zone with occasional large blast like malignant lymphoid cells. Other points we have to reveal are epithelial histocytes, sinus invasion, and plasmacytic differentiation of proliferating cells[5] (Figure 4).
PSL (follicular type): It is neoplastic proliferation of follicle center B-cells, i.e., centrocytes and centroblasts exhibiting follicular pattern (Figure 5).
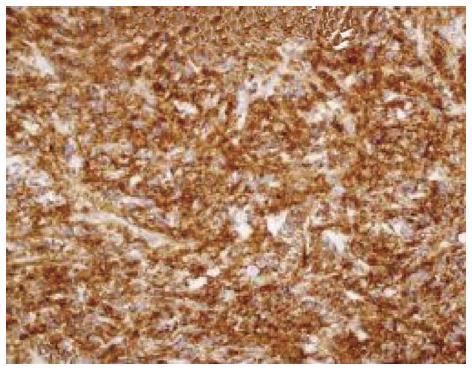
Histopathology report is to be confirmed by IHC. The tumor cells are immunopositive for B cell markers, e.g., CD 20 and immunonegative for T cell markers (Figure 6).
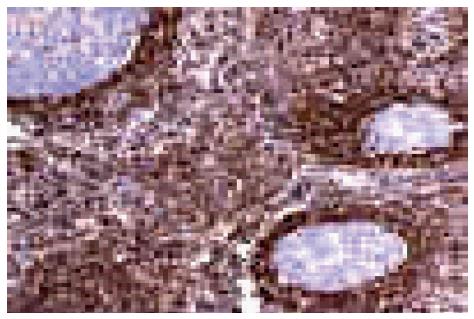
B cell lymphoma: B cell lymphoma-2 (BCL-2) immunoreactivity is useful to differentiate malignant lymphoma (BCL-2 positive) from reactive (BCL-2 negative) B cells in the marginal zone (Figure 7).
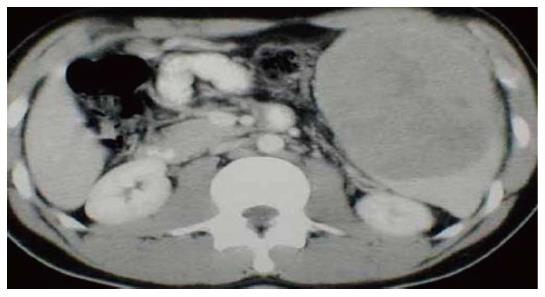
US imaging of the abdomen and whole-body computed tomography (Figure 8) scan are to be done in each and every case with splenomegaly. The B mode USG determines the actual size of spleen and computed tomography confirms the involvement of hilar lymph nodes[23,24].
The previous workers suggested splenectomy as an effective diagnostic and therapeutic tool[25,26]. It has morbidity and mortality rates accounting for approximately 12% and less than 1%, respectively[27]; Now a days, laparoscopic splenectomy can be used as a safe and efficient method, reducing both the mortality and morbidity significantly[28]. In this the distortion of the samples should be strictly avoided.
Needle core biopsy is more efficient and safe and can be used in high risk patients also. Previous studies[29,30] concluded that splenic needle biopsy has low complication rates with high diagnostic utility. Recently, laparoscopic splenectomy has often been used for splenic masses because of fewer complications and since it is rather appropriate for moderate splenomegaly[30,31].
Echo-guided splenic biopsy and FNAC are effective in peripherally located lesions[32].
Splenic DLBCLs are clinically aggressive neoplasms. So, line of treatment of such SLs should be same as DLBCLS[33]. Splenic form of the micronodular T-cell/histiocyte-rich DLBCL subtype presents with micronodules in the spleen with involvement of bone marrow or other extranodal sites[34,35].
Gastrosplenic fistula is associated with benign peptic ulcer disease, gastric Crohn’s disease, gastric adenocarcinoma, and primary gastric and splenic lymphomas. There occurs hemorrhage due to erosion by primary splenic lesion in the stomach. Upper intestinal hemorrhage can be successfully treated with splenic artery embolization, followed by splenectomy and gastric resection[35].
To conclude, splenic needle biopsy or core biopsy can be used as an effective diagnostic tool now days to hit the correct histological diagnosis to avoid untoward complications related to disease and treatment in search of accurate pathological diagnosis.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country of origin: India
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Chan EL, Liu QD S- Editor: Kong JX L- Editor: A E- Editor: Wu HL
| 1. | Dasgupta T, Coombes B, Brasfield rd. primary malignant neoplasms of the spleen. Surg Gynecol Obstet. 1965;120:947-960. [PubMed] |
| 2. | Cavanna L, Artioli F, Vallisa D, Di Donato C, Bertè R, Carapezzi C, Foroni R, Del Vecchio C, Lo Monaco B, Prati R. Primary lymphoma of the spleen. Report of a case with diagnosis by fine-needle guided biopsy. Haematologica. 1995;80:241-243. [PubMed] |
| 3. | Harris NL, Aisenberg AC, Meyer JE, Ellman L, Elman A. Diffuse large cell (histiocytic) lymphoma of the spleen. Clinical and pathologic characteristics of ten cases. Cancer. 1984;54:2460-2467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 4. | Burke JS. Surgical pathology of the spleen: an approach to the differential diagnosis of splenic lymphomas and leukemias. Part II. Diseases of the red pulp. Am J Surg Pathol. 1981;5:681-694. [PubMed] |
| 5. | Ingle SB, Ingle CR. Splenic lymphoma with massive splenomegaly: Case report with review of literature. World J Clin Cases. 2014;2:478-481. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 6. | Gobbi PG, Grignani GE, Pozzetti U, Bertoloni D, Pieresca C, Montagna G, Ascari E. Primary splenic lymphoma: does it exist? Haematologica. 1994;79:286-293. [PubMed] |
| 7. | Healy NA, Conneely JB, Mahon S, O’Riardon C, McAnena OJ. Primary splenic lymphoma presenting with ascites. Rare Tumors. 2011;3:e25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Kraemer BB, Osborne BM, Butler JJ. Primary splenic presentation of malignant lymphoma and related disorders. A study of 49 cases. Cancer. 1984;54:1606-1619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Kehoe J, Straus DJ. Primary lymphoma of the spleen. Clinical features and outcome after splenectomy. Cancer. 1988;62:1433-1438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Falk S, Stutte HJ. Primary malignant lymphomas of the spleen. A morphologic and immunohistochemical analysis of 17 cases. Cancer. 1990;66:2612-2619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Ahmann DL, Kiely JM, Harrison EG, Payne WS. Malignant lymphoma of the spleen. A review of 49 cases in which the diagnosis was made at splenectomy. Cancer. 1966;19:461-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Kim KH, Cho CK, Choo SW, Kim HJ, Kim KS. Primary lymphoma of the spleen- a case report. Korean J Surg. 1997;52:912-917. |
| 13. | Hahn JS, Lee S, Chong SY, Min YH, Ko YW. Eight-year experience of malignant lymphoma--survival and prognostic factors. Yonsei Med J. 1997;38:270-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Dachman AH, Buck JL, Krishnan J, Aguilera NS, Buetow PC. Primary non-Hodgkin’s splenic lymphoma. Clin Radiol. 1998;53:137-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 43] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Xiros N, Economopoulos T, Christodoulidis C, Dervenoulas J, Papageorgiou E, Mellou S, Styloyiannis S, Tsirigotis P, Raptis SA. Splenectomy in patients with malignant non-Hodgkin’s lymphoma. Eur J Haematol. 2000;64:145-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Brox A, Bishinsky JI, Berry G. Primary non-Hodgkin lymphoma of the spleen. Am J Hematol. 1991;38:95-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 48] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Izzo L, Binda B, Boschetto A, Carmanico L, Galati G, Fior E, Marini M, Mele LL, Stasolla A. Primary Splenic Lymphoma; the diagnostic and therapeutic value of splenectomy. Haematologica. 2002;87; ECR 20. |
| 18. | Agrawal SC, Bharucha MA, Deo A, Velling K. Post surgical diagnosis of primary DLBCL presenting as Splenic abscess. Austral - Asian Journal of Cancer. 2012;11:217-220. |
| 19. | Konstantiadou I, Mastoraki A, Papanikolaou IS, Sakorafas G, Safioleas M. Surgical approach of primary splenic lymphoma: report of a case and review of the literature. Indian J Hematol Blood Transfus. 2009;25:120-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Thanos L, Dailiana T, Papaioannou G, Nikita A, Koutrouvelis H, Kelekis DA. Percutaneous CT-guided drainage of splenic abscess. AJR Am J Roentgenol. 2002;179:629-632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 58] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 21. | Skarin AT, Davey FR, Moloney WC. Lymphosarcoma of the spleen. Results of diagnostic splenectomy in 11 patients. Arch Intern Med. 1971;127:259-265. [PubMed] |
| 22. | López JI, Del Cura JL, De Larrinoa AF, Gorriño O, Zabala R, Bilbao FJ. Role of ultrasound-guided core biopsy in the evaluation of spleen pathology. APMIS. 2006;114:492-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Lamb PM, Lund A, Kanagasabay RR, Martin A, Webb JA, Reznek RH. Spleen size: how well do linear ultrasound measurements correlate with three-dimensional CT volume assessments? Br J Radiol. 2002;75:573-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 103] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 24. | Peddu P, Shah M, Sidhu PS. Splenic abnormalities: a comparative review of ultrasound, microbubble-enhanced ultrasound and computed tomography. Clin Radiol. 2004;59:777-792. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 41] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 25. | Iannitto E, Tripodo C. How I diagnose and treat splenic lymphomas. Blood. 2011;117:2585-2595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 69] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 26. | Vander Walt JD. Lymphomas in the bone marrow. Diagn Histopathol. 2010;16:125-142. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 27. | Baccarani U, Terrosu G, Donini A, Zaja F, Bresadola F, Baccarani M. Splenectomy in hematology. Current practice and new perspectives. Haematologica. 1999;84:431-436. [PubMed] |
| 28. | Grahn SW, Alvarez J, Kirkwood K. Trends in laparoscopic splenectomy for massive splenomegaly. Arch Surg. 2006;141:755-761; discussion 761-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 73] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 29. | Tam A, Krishnamurthy S, Pillsbury EP, Ensor JE, Gupta S, Murthy R, Ahrar K, Wallace MJ, Hicks ME, Madoff DC. Percutaneous image-guided splenic biopsy in the oncology patient: an audit of 156 consecutive cases. J Vasc Interv Radiol. 2008;19:80-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 42] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 30. | Gómez-Rubio M, López-Cano A, Rendón P, Muñoz-Benvenuty A, Macías M, Garre C, Segura-Cabral JM. Safety and diagnostic accuracy of percutaneous ultrasound-guided biopsy of the spleen: a multicenter study. J Clin Ultrasound. 2009;37:445-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 40] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 31. | Armitage JO. How I treat patients with diffuse large B-cell lymphoma. Blood. 2007;110:29-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 101] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 32. | Tessier DJ, Pierce RA, Brunt LM, Halpin VJ, Eagon JC, Frisella MM, Czerniejewski S, Matthews BD. Laparoscopic splenectomy for splenic masses. Surg Endosc. 2008;22:2062-2066. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 33. | Shimizu I, Ichikawa N, Yotsumoto M, Sumi M, Ueno M, Kobayashi H. Asian variant of intravascular lymphoma: aspects of diagnosis and the role of rituximab. Intern Med. 2007;46:1381-1386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 34. | Kan E, Levy I, Benharroch D. Splenic micronodular T-cell/histiocyte-rich large B-cell lymphoma: effect of prior corticosteroid therapy. Virchows Arch. 2009;455:337-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 35. | Bird MA, Amjadi D, Behrns KE. Primary splenic lymphoma complicated by hematemesis and gastric erosion. South Med J. 2002;95:941-942. [PubMed] |