Published online Apr 16, 2014. doi: 10.12998/wjcc.v2.i4.86
Revised: March 8, 2014
Accepted: March 17, 2014
Published online: April 16, 2014
Processing time: 82 Days and 5 Hours
Endoscopic hemorrhoidal band ligation is a well-established nonoperative method for treatment of bleeding internal hemorrhoids (grade 1 to 3). It is a safe and effective technique with a high success rate. Complications with this procedure are uncommon. Although rectal ulceration due to band ligation is a rare complication, it can cause life-threatening hemorrhage especially when patients are on medications which impair hemostasis like aspirin or non steroidal anti-inflammatory drugs. We present 2 cases of massive lower gastro-intestinal bleeding in patients who had a band ligation procedure performed 2 wk prior to the presentation and were on aspirin at home. Both the patients were hemodynamically unstable requiring resuscitation. They required platelet and blood transfusions and were found to have rectal ulcers on colonoscopy done subsequently. The rectal ulcers corresponded to the site of band ligation. The use of aspirin by these patients would have caused defects in the hemostasis and may have predisposed them to massive bleeding in the presence of rectal ulcers occurring after the band ligation procedure. Managing aspirin before and after the ligation may be difficult especially since adequate guidelines are unavailable. Stopping aspirin in all the cases might not be safe and the decision should be individualized.
Core tip: Rubber band ligation is known to be a relatively safe procedure. Massive bleeding and rectal ulceration is a very rare complication of this procedure. We came across two cases of severe, life-threatening lower gastrointestinal hemorrhage following endoscopic hemorrhoidal band ligation in patients on aspirin. The use of aspirin and other non-steroidal anti-inflammatory drugs can predispose to massive hemorrhage. The case report aims at creating awareness about these complications and that it may be advisable to avoid aspirin and non steroidal anti-inflammatory drugs immediately after band ligation.
- Citation: Patel S, Shahzad G, Rizvon K, Subramani K, Viswanathan P, Mustacchia P. Rectal ulcers and massive bleeding after hemorrhoidal band ligation while on aspirin. World J Clin Cases 2014; 2(4): 86-89
- URL: https://www.wjgnet.com/2307-8960/full/v2/i4/86.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v2.i4.86
Hemorrhoids are dilated or bulging veins in the rectum and/or anus caused by increased pressure in the rectal veins. They are believed to be normal anatomic structures, as demonstrated by their presence in babies[1]. Frequently, they can become a source of significant morbidity if they get inflamed or swollen. The estimated prevalence rate of symptomatic hemorrhoids in the United States is 4.4% of the adult population. More than one million individuals are affected annually by hemorrhoidal conditions[2,3]. The prevalence peaks between the ages of 45-65 and declines thereafter. It is more commonly found in whites more than blacks and the rates are higher in people from higher socioeconomic background[2].
Elastic band ligation is a well-established nonoperative method for treatment of bleeding internal hemorrhoids (stages II-III). Usually, one or two bands are placed at a single session by using rigid instruments. Endoscopic hemorrhoidal band ligation is a safe and effective technique used in the management of hemorrhoids, with a high success rate[4]. Blaisdell[5] and Barron[6] described and refined the band ligation therapy. Complications with this procedure are uncommon.
Massive bleeding and rectal ulceration due to band ligation is a very rare complication. The use of aspirin (acetylsalicylic acid, ASA) and other non-steroidal anti-inflammatory drugs (NSAID) can predispose to massive hemorrhage. We came across two cases of severe, life-threatening lower gastrointestinal hemorrhage following endoscopic hemorrhoidal band ligation in patients on aspirin.
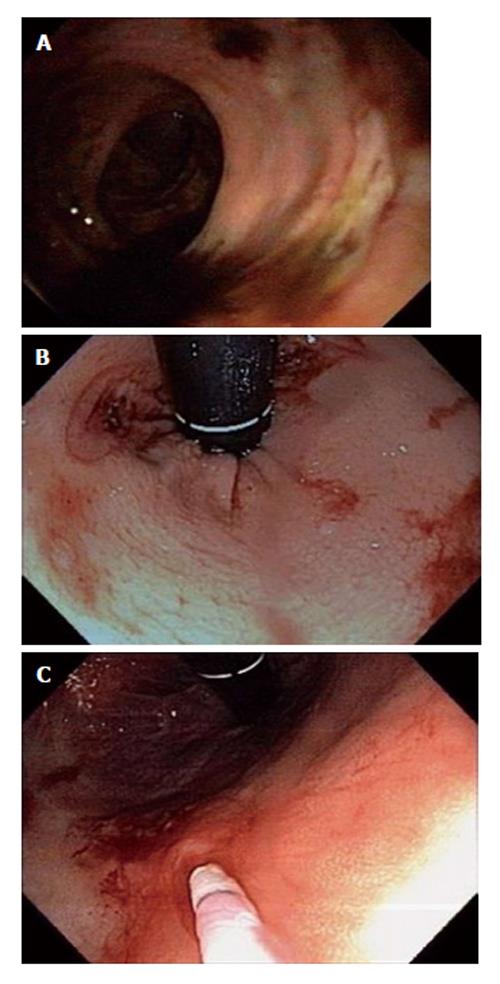
A 52-year-old white man with a past medical history of anxiety and a recent band ligation for hemorrhoids 15 d prior to presentation came to the emergency room (ER) complaining of bleeding from his rectum for 2 h. He was in his usual state of health when he suddenly had a large bowel movement with bright red blood and clots. He had no other complaints such as abdominal pain, coffee ground vomiting or black stools. His medications included aspirin (81 mg/d) for preventing cardiovascular disease and Sertraline for his anxiety. His blood pressure (BP) was 130/76 mmHg, temperature was 98.3 F, respiratory rate was 16/min and the heart rate (HR) was 96/min. His abdomen was soft, with normal bowel sounds and no tenderness or guarding. His rectal exam revealed reduced sphincter tone and bright red blood. His BP subsequently dropped to 80/40 mmHg with a HR of 140/min within an hour. He became unresponsive and was subsequently intubated for airway protection in the ER. His initial blood work revealed a hemoglobin of 12 g/dL and platelets of 199000. Due to hemodynamic collapse and the large volume of blood seen in the stool, he received fluids, 2 units of packed red blood cells and 1 unit of platelets after which his vital signs stabilized. ASA was discontinued. He underwent a colonoscopy (Figure 1A) which showed two clean based rectal ulcers measuring 3 cm and 1cm with overlying exudates 7 cm from the anal verge. The location of the rectal ulcers corresponded to the site of band ligation. The rectal ulcer biopsy revealed active chronic inflammation with surface exudates and attached fragment of granulation tissue. Bleeding subsequently stopped and the patient was extubated on day 2 of admission and later discharged after an otherwise uncomplicated hospital course.
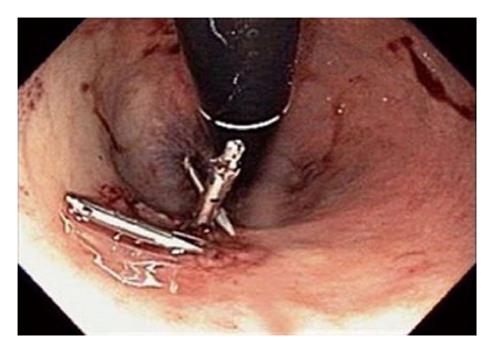
A 67-year-old white man presented to the ER with complaints of bleeding from his rectum for 4 h. He was known to have symptomatic hemorrhoids for which he underwent band ligation 2 wk prior to the presentation. He denied abdominal pain, nausea, vomiting, black stools or any other complaints. His past medical history was significant for hypertension, hyperlipidemia, coronary artery disease for which he underwent Coronary Artery Bypass Graft surgery in 2004 and stroke with no residual neurological deficits in 2005. His medications included Aggrenox (aspirin/Dipyridamole -25/200 mg twice a day for stroke prevention), Amlodipine, Metoprolol, Atorvastatin and Ezetimibe. On arrival, he was afebrile with a BP of 80/50 mmHg and a HR of 62 beats per minute. The absence of tachycardia was presumed to be due to the beta blockade. His abdomen was soft, with normal bowel sounds and no tenderness or guarding. The rectal exam revealed bright red blood with clots, normal sphincter tone and no palpable masses. His initial hemoglobin was 14 g/dL and platelet count was 187000. His hemoglobin decreased to 10 g/dL over 10 h and he continued to have rectal bleeding. Due to ongoing bleeding and hemodynamic instability he received fluids, 2 units of packed red blood cells and 1 unit of platelets. An emergent colonoscopy was then performed which showed a solitary rectal ulcer (Figure 1B and C) of 1 cm size with a visible vessel proximal to the dentate line. The visible vessel was successfully clipped endoscopically (Figure 2). The location of the rectal ulcer corresponded to the site of band ligation. No further bleeding was noted and the patient was subsequently discharged home.
Initial treatment for mild to moderate hemorrhoidal disease consists of increased fiber intake[7], oral hydration, use of NSAIDs for pain, avoidance of straining during defecation, and sitz baths[8]. Hemorrhoids that fail to respond to medical management may be treated with rubber band ligation, sclerosis, and thermotherapy by using infrared beam, electric current, CO2 laser, or ultrasonic energy. Surgery is reserved for those who fail to improve with conservative measures.
Rubber band ligation is found to be the most effective method to treat symptomatic internal hemorrhoids (grade 1 to 3) that have failed to respond to conservative management[4,9-11]. Complications associated with ligation are uncommon (< 2%) and usually benign which may include pain, rectal bleeding from early dislodgment, vasovagal response or infection[12,13]. Bleeding after ligation may occur immediately after the procedure or 3-10 d after the rubber band and the ligated tissue fall off. Rectal ulcers after the band ligation are extremely rare complication. The exact incidence is unknown. These ulcers can lead to massive life threatening bleeding especially in the patients taking antiplatelet agents like aspirin. ASA and other NSAIDs inhibit platelet production of thromboxane A2. ASA irreversibly acetylates the platelet enzyme so that a single dose impairs hemostasis for five to seven days hence causing hemostasis defects[14]. Recovery of the platelets after discontinuing these drugs is slow and is equivalent to the lifespan of the platelets. The other NSAIDs are competitive and reversible inhibitors with more transient effects.
A prospective study of 512 patients by Bat et al[15] who underwent hemorrhoidal rubber band ligation over a seven-year period were followed up for any complications. Most of the patients, who had hemorrhoidal band ligation, had a successful event free outcome (82%). Minor complications were found in 24 patients (4.7%) including painful, thrombosed hemorrhoids, slippage of bands, minor rectal bleeding, chronic longitudinal ulcers and priapism. Major complications were noted in 13 patients (2.5%) who had either delayed massive bleeding or severe complicated thrombosis of the hemorrhoids. Five of the six patients who had massive bleeding, had the onset of symptoms 10 d or more after the procedure similar to our 2 patients. Three of the six patients with massive bleeding required transfusions. Two of the three patients who were transfused were taking aspirin regularly.
Both our cases developed massive bleeding 2 wk following the banding procedure requiring platelet and blood transfusions. The use of aspirin by these patients would have caused defects in the hemostasis and may have predisposed them to massive life-threatening hemorrhage in the presence of rectal ulcers occurring after the band ligation procedure. The first patient was taking ASA for preventing cardiovascular diseases and aspirin could have been safely stopped atleast 1 wk prior to the procedure. On the contrary, the second patient had a history of coronary artery bypass graft and a stroke, stopping ASA in him abruptly might have caused more harm. Managing ASA before and after the ligation may be difficult especially since adequate guidelines are unavailable. Stopping ASA in all the cases might not be safe and the decision should be individualized.
The cases we report are an example of a rare and life threatening complication of a procedure known to be relatively safe. Use of aspirin may have been a coincidence or would have predisposed the patient to a massive bleeding. It may be advisable to avoid ASA and NSAIDs immediately after band ligation.
Two men, age 52 and 67, on aspirin at home came to the emergency room with bright red blood per rectum 2 wk after a hemorrhoidal band ligation.
The authors came across two cases of severe, life-threatening lower gastrointestinal hemorrhage following endoscopic hemorrhoidal band ligation in patients on aspirin.
Diverticular disease, hemorrhoids, colitis, bleeding ulcers.
Patient one had a hemoglobin of 12 g/dL and platelets of 199000 on admission. Patient 2 had a hemoglobin of 14 g/dL and a platelet count of 187000 initially. Both patients were losing blood rapidly leading to drop in the hemoglobin subsequently.
Colonoscopy was performed in both the cases which showed two clean based rectal ulcers measuring 3 cm and 1 cm with overlying exudates 7 cm from the anal verge in the first case and a solitary rectal ulcer of 1 cm size with a visible vessel proximal to the dentate line in the second case.
In the first case, rectal ulcer biopsy revealed active chronic inflammation with surface exudates and attached fragment of granulation tissue. No biopsy was performed in the second patient.
Treatment mainly included platelet and blood transfusions. The second patient had a rectal ulcer with a visible vessel which was endoscopically clipped.
There are a very few case reports which have described massive bleeding after hemorrhoidal band ligation in patients on aspirin.
Rubber band ligation is a procedure performed endoscopically in which rubber bands are tied off at the base of the hemorrhoids hence, cutting off the blood flow to the hemorrhoids.
Massive bleeding is a rare but life threatening complication of a fairly safe procedure which may be avoided if we attempt to tailor the use of aspirin pre and post band ligation according to individual patient conditions.
This is an easy to read, well written and an interesting case report worth highlighting in the surgical community since rubber band ligation is a very commonly performed procedure.
P- Reviewers: Botaitis BC, Burke D S- Editor: Zhai HH L- Editor: A E- Editor: Liu SQ
| 1. | Thomson WH. The nature of haemorrhoids. Br J Surg. 1975;62:542-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 440] [Cited by in RCA: 328] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 2. | Johanson JF, Sonnenberg A. The prevalence of hemorrhoids and chronic constipation. An epidemiologic study. Gastroenterology. 1990;98:380-386. [PubMed] |
| 3. | Bleday R, Pena JP, Rothenberger DA, Goldberg SM, Buls JG. Symptomatic hemorrhoids: current incidence and complications of operative therapy. Dis Colon Rectum. 1992;35:477-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 151] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 4. | MacRae HM, McLeod RS. Comparison of hemorrhoidal treatment modalities. A meta-analysis. Dis Colon Rectum. 1995;38:687-694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 333] [Cited by in RCA: 250] [Article Influence: 8.3] [Reference Citation Analysis (2)] |
| 5. | Blaisdell PC. Prevention of massive hemorrhage secondary to hemorrhoidectomy. Surg Gynecol Obstet. 1958;106:485-488. [PubMed] |
| 6. | Barron J. Office ligation treatment of hemorrhoids. Dis Colon Rectum. 1963;6:109-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 59] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Moesgaard F, Nielsen ML, Hansen JB, Knudsen JT. High-fiber diet reduces bleeding and pain in patients with hemorrhoids: a double-blind trial of Vi-Siblin. Dis Colon Rectum. 1982;25:454-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 62] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Dodi G, Bogoni F, Infantino A, Pianon P, Mortellaro LM, Lise M. Hot or cold in anal pain? A study of the changes in internal anal sphincter pressure profiles. Dis Colon Rectum. 1986;29:248-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 50] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Templeton JL, Spence RA, Kennedy TL, Parks TG, Mackenzie G, Hanna WA. Comparison of infrared coagulation and rubber band ligation for first and second degree haemorrhoids: a randomised prospective clinical trial. Br Med J (Clin Res Ed). 1983;286:1387-1389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 45] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Walker AJ, Leicester RJ, Nicholls RJ, Mann CV. A prospective study of infrared coagulation, injection and rubber band ligation in the treatment of haemorrhoids. Int J Colorectal Dis. 1990;5:113-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 52] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Johanson JF, Rimm A. Optimal nonsurgical treatment of hemorrhoids: a comparative analysis of infrared coagulation, rubber band ligation, and injection sclerotherapy. Am J Gastroenterol. 1992;87:1600-1606. [PubMed] |
| 12. | O’Hara VS. Fatal clostridial infection following hemorrhoidal banding. Dis Colon Rectum. 1980;23:570-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 46] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Russell TR, Donohue JH. Hemorrhoidal banding. A warning. Dis Colon Rectum. 1985;28:291-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 65] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Handin RI. Disorders of the platelet and vessel wall. Harrison‘s Principles of Medicine, 14th ed. New York: McGraw-Hill Companies Inc 1998; 730-736. |
| 15. | Bat L, Melzer E, Koler M, Dreznick Z, Shemesh E. Complications of rubber band ligation of symptomatic internal hemorrhoids. Dis Colon Rectum. 1993;36:287-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 70] [Article Influence: 2.2] [Reference Citation Analysis (0)] |