Published online Feb 16, 2014. doi: 10.12998/wjcc.v2.i2.48
Revised: November 30, 2013
Accepted: January 7, 2014
Published online: February 16, 2014
Processing time: 153 Days and 16.2 Hours
Ameloblastic carcinoma is a rare odontogenic tumor exhibiting histological evidence of malignancy in the primary or recurrent tumor. It is characterized by rapid, painful expansion of the jaw, unlike conventional ameloblastomas. The tumor most frequently involves the mandible. The expanding lesion causes perforation of the buccal and lingual plates of the jaw and invades the surrounding soft tissue. Rapidly growing large tumor mass may cause tooth mobility. A mandibular tumor involving the mental nerve leads to paresthesia of the nerve. A maxillary tumor can produce a fistula in the palate and paresthesia of the infraorbital nerve. Most ameloblastic carcinomas are presumed to have arisen de novo with a few cases of malignant transformation of ameloblastomas. Although rare, these lesions have been known to metastasize, mostly to the regional lymph nodes or lungs. A case of ameloblastic carcinoma in a 60-year-old man is reported here and its clinical, radiological and histological features are discussed.
Core tip: Clinically, ameloblastic carcinoma is more aggressive than most typical ameloblastomas, with extensive local destruction, perforation of the cortical plate, extension into surrounding soft tissues, numerous recurrent lesions and metastasis, usually to cervical lymph nodes. Histologically, the tumor cells resemble cells seen in ameloblastoma but show cytological atypia, cellular pleomorphism, nuclear hyperchromatism, mitoses and vascular and neural invasion. These identifying features of ameloblastic carcinoma must be known and recognized by dental practitioners. It is probable that ameloblastoma, like other tumors (such as carcinoid tumors and epithelial tumors of the ovary), shows a spectrum of histological and biological behavior, ranging from benignity at one end to frank malignancy at the other.
- Citation: Srikanth MD, Radhika B, Metta K, Renuka NV. Ameloblastic carcinoma: Report of a rare case. World J Clin Cases 2014; 2(2): 48-51
- URL: https://www.wjgnet.com/2307-8960/full/v2/i2/48.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v2.i2.48
Malignant odontogenic tumors are very uncommon and ameloblastic carcinoma is a rare odontogenic carcinoma, with very few such cases being reported so far. The frequency of malignant change in ameloblastomas is difficult to establish but probably may be less than 1% among all cases of ameloblastomas[1].
The terminology for these lesions is somewhat controversial. The term malignant ameloblastoma should be used for a tumor that shows the histopathological features of ameloblastoma, both in the primary tumor and in the metastatic deposits[2]. However, the term ameloblastic carcinoma should be reserved for an ameloblastoma that has cytological features of malignancy in the primary tumor, in a recurrence, or in any metastatic deposit[3]. These lesions may follow a markedly aggressive local course but metastases do not necessarily occur[4].
Odontogenic carcinoma signifies the primary malignant epithelial tumors of the terms that are so poorly differentiated that they bear little or no resemblance to any of the odontogenic apparatus. With the presence of many clear cells in conjunction with the other patterns and histological features considered to be indicative of malignancy in these lesions and in keeping with the guidelines of World Health Organization (WHO) classification of odontogenic tumors, some authors even prefer to designate these tumors as clear cell ameloblastic carcinoma or ameloblastic carcinoma, clear cell variant.
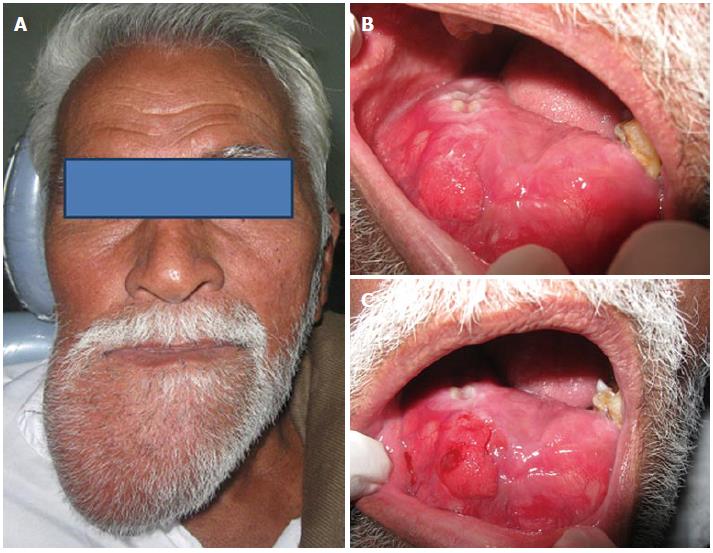
A 60-year-old male patient came to the department of oral medicine and radiology with a chief complaint of swelling over the right side of the face for 10 years (Figure 1A). History revealed that he first noticed a small intra oral swelling at the labial aspect of lower right canine region which gradually increased in size. Initially he noticed pain in that region but subsequently but there was no pain and the swelling increased progressively to the present size. The patient also noticed development of paresthesia of the lower lip with pain over the swelling.
On examination, a huge extra oral swelling was found, measuring around 23 cm × 11.5 cm in size, extending from the right side of mandible and crossing the midline with well defined margins, hard in consistency, with tenderness over the swelling. Intra oral examination revealed complete obliteration of the buccal and labial vestibule on the right side, with the swelling extending in to the anterior region of the floor of the mouth (Figure 1B). It had a normal mucosal color and 31-33 and 41-47 teeth were missing. The intra oral swelling was hard in consistency and tenderness was present on palpation (Figure 1C).
In light of the above findings and the nature and duration of the lesion, a provisional diagnosis of ameloblastoma was considered and odontogenic myxoma and osteosarcoma were considered for a differential diagnosis.
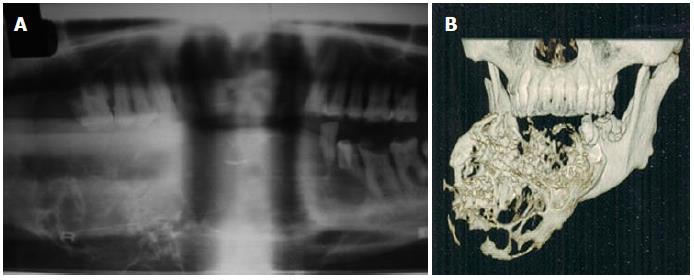
The patient had an orthopantomograph (OPG), computed tomography (CT) mandible and magnetic resonance imaging. OPG showed huge multilocular radiolucency with the septa giving an appearance of a soap bubble or honeycomb extending from the ramus molar region on right side, crossing the midline to the lower left premolar region (Figure 2A). CT dental scan showed an enlarged tumor extending from the ramus region of 48 to the 35 region (Figure 2B). The tumor caused severe expansion of the buccal and lingual cortical plates with a multilocular appearance.
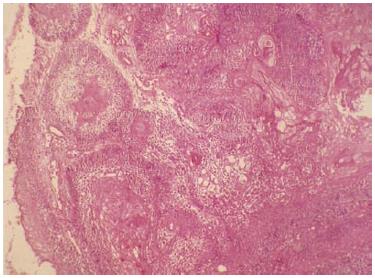
Excisional biopsy revealed numerous epithelial follicles spread out in a scanty connective tissue stroma. The epithelial nests showed typical (tall) columnar peripheral cells with apically placed nuclei and vacuolated cytoplasm. The central cells showed squamous metaplasia and numerous keratin pearls. A few cells showed features of dysplasia, such as irregular aggregation, cellular and nuclear pleomorphism with nuclear hyperchromasia (Figure 3).
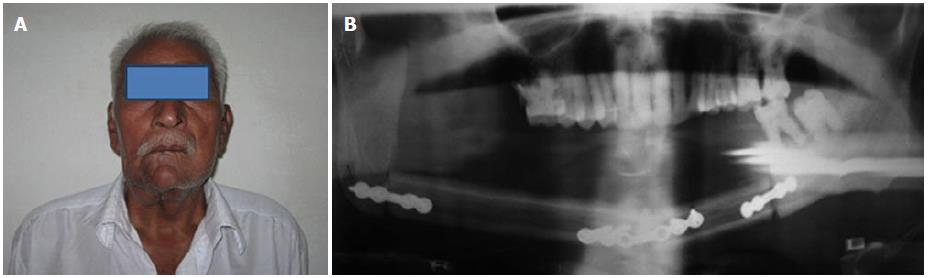
The histological features were consistent with ameloblastic carcinoma. Myxomas radiologically show honeycomb variant and fine trabeculations within the small lobules not present in ameloblastoma. Osteosarcoma is a common primary malignant tumor affecting the jaw and radiologically a sunray appearance is present. Hence, they were excluded and a final diagnosis of ameloblastic carcinoma was made. The patient underwent surgical resection of the tumor by microvascular reconstructive surgery with complete resection of the mandible and reconstruction of the mandible was done by fibula graft (Figure 4). The patient is being followed up closely.
Ameloblastic carcinoma is a rare neoplasm that represents a challenge in its diagnosis, treatment and prognosis. Information regarding its clinical features is scanty[5]. The demographic data of ameloblastic carcinoma reported in the literature suggests that it is more common in males (M:F 1.5:1) and the site of distribution is in the mandible, particularly in the posterior mandible[1]. The age range of occurrence shows a large variation with an average age of 39.8 years. However, a few authors have stated that the sixth decade is the predominant age group. Ameloblastic carcinoma has been reported to arise either de novo or from a preexisting odontogenic cyst or ameloblastoma[5].
The common clinical signs and symptoms include swelling, pain, trismus and dysphonia[6] and there are several classifications: (1) WHO classification of odontogenic carcinomas: malignant ameloblastoma; primary intraosseous carcinoma; malignant variants of other odontogenic tumors; and malignant changes in odontogenic cysts; (2) Classification of odontogenic carcinomas according to Slootweg and Muller: primary intraosseous carcinoma, e.g., odontogenic cyst (Type I); malignant ameloblastoma (type IIA); ameloblastoma carcinoma, arising de novo, e.g., ameloblastoma, or e.g., odontogenic tumor (type IIB); and primary intraosseous carcinoma arising de novo (type IIIA: non keratinizing; type IIIB: keratinizing); and (3) LJ Slater, Oral and Maxillofacial Clinics of North America - odontogenic carcinomas: metastasizing ameloblastoma; ameloblastic carcinoma; carcinoma, e.g., ameloblastoma; primary intraosseous carcinoma; solid; cystic (e.g., odontogenic cyst); central mucoepidermoid carcinoma; ghost cell odontogenic carcinoma; and clear cell odontogenic carcinoma.
The diagnostic criteria of an ameloblastic carcinoma that differentiate from ameloblastoma are based on cytological atypia and an increased mitotic index[5]. The histological changes should include a higher proliferative index emphasized by higher mitotic activity, higher proliferating cell nuclear antigen expression and higher ki67, atypia such as nuclear pleomorphism and basilar hyperplasia, hyperchromatic nuclei of basaloid cells, and other features of malignancy, such as peripheral or perivascular invasion. This should be correlated with the clinical features. The four important characteristics include[5] growth rate, the propensity for ameloblastic carcinoma to perforate the cortex, pain, as a third of patients with ameloblastic carcinoma experience pain or discomfort, and sensory disturbance, such as paresthesia which is rare with ameloblastoma.
Ameloblastic carcinoma is an aggressive neoplasm that is locally invasive and can spread to regional lymph nodes or distant metastatic sites such as long bones. It is managed with wide local excision, elective or therapeutic neck dissection and post operative radiation therapy[5]. Radiotherapy and chemotherapy seem to be of limited value. The prognosis is poor and hence close follow up of the patient is needed.
Although the reported cases of ameloblastic carcinoma are scarce, the above features can be applied to diagnose an ameloblastic carcinoma at an early stage to enable early intervention and better treatment[7].
A case of ameloblastic carcinoma in a 60-year-old man is reported here and its clinical, radiological and histological features are discussed.
The patient had an orthopantomograph (OPG), computed tomography mandible and magnetic resonance imaging. OPG showed huge multilocular radiolucency with the septa giving an appearance of a soap bubble or honeycomb extending from the ramus molar region on right side, crossing the midline to the lower left premolar region.
Excisional biopsy revealed numerous epithelial follicles spread out in a scanty connective tissue stroma.
The patient underwent surgical resection of the tumor by microvascular reconstructive surgery with complete resection of mandible and the reconstruction of the mandible was done by a fibula graft.
It is probable that ameloblastoma, like other tumors (such as carcinoid tumors and epithelial tumors of the ovary), shows a spectrum of histological and biological behavior, ranging from benignity at one end to frank malignancy at the other.
Ameloblastic carcinoma is a rare malignant tumor. This report is very interesting.
P- Reviewers: Abu El-Naaj I, Asaumi J S- Editor: Zhai HH L- Editor: Roemmele A E- Editor: Wu HL
| 1. | Rajendran R. Shafer’s textbook of oral pathology. 6th ed. India: Elsevier publisher 2009; . |
| 2. | Neville BW, Damm DD, Allen CM, Bouquot JE. Odontogenic cysts and tumors. Oral and maxillofacial pathology. Philadelphia: Saunders 2002; 589. |
| 3. | Wood ND, Goaz PW. Differential diagnosis of oral and maxillofacial region. 5th ed. St. Louis: The CV Mosby Company 1997; . |
| 4. | Hall JM, Weathers DR, Unni KK. Ameloblastic carcinoma: an analysis of 14 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:799-807. [PubMed] |
| 5. | Akrish S, Buchner A, Shoshani Y, Vered M, Dayan D. Ameloblastic carcinoma: report of a new case, literature review, and comparison to ameloblastoma. J Oral Maxillofac Surg. 2007;65:777-783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 43] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 6. | Suomalainen A, Hietanen J, Robinson S, Peltola JS. Ameloblastic carcinoma of the mandible resembling odontogenic cyst in a panoramic radiograph. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:638-642. [PubMed] |
| 7. | Lau SK, Tideman H, Wu PC. Ameloblastic carcinoma of the jaws. A report of two cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:78-81. [PubMed] |