Published online Dec 16, 2014. doi: 10.12998/wjcc.v2.i12.938
Revised: August 21, 2014
Accepted: September 23, 2014
Published online: December 16, 2014
Processing time: 213 Days and 0.2 Hours
The authors have presented a technique of full occlusal rehabilitation in a case of severe dental fluorosis. In this technique, maxillary and mandibular anterior teeth were simultaneously prepared and restored first. This was followed by simultaneous preparation of maxillary and mandibular posterior teeth that were restored in canine guided occlusion. The technique and sequence followed here is unique and is not available in dental literature. This technique reduces number of appointments while fulfilling all objectives. Periodontal follow-up over 3 years was satisfactory. A restorative treatment protocol has been devised for fluorosis which will act as a guide for the dental practitioners.
Core tip: A novel technique of full occlusal rehabilitation is illustrated here. It is a simple procedure which adheres to all the principles of occlusal rehabilitation. Rehabilitation of dental fluorosis using the treatment protocol suggested here will systematize and streamline the clinical technique and it is hoped that this approach will benefit the patients and act as a guide for dentists. Although the technique described here is skill sensitive, it is the author’s belief that it is a new paradigm in full mouth occlusal rehabilitation.
- Citation: Joshi N, Palaskar J, Joshi M, Kathariya R. Complete oral rehabilitation in a case with severe dental fluorosis. World J Clin Cases 2014; 2(12): 938-942
- URL: https://www.wjgnet.com/2307-8960/full/v2/i12/938.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v2.i12.938
There are hardly any documented cases in dental literature where dental fluorosis is treated by full occlusal rehabilitation. Restoration of dentitions affected by dental fluorosis is a challenging prospect. The presence of dental hypoplasia, the severity of discoloration, associated symptoms like hypersensitivity and attrition makes treatment planning extremely critical. The majority of fluorosis patients usually have mild to moderate fluorosis[1,2] wherein the main symptoms are discoloration and/or very mild hypoplasia[3,4]. These may be managed by simple restorative procedures like bleaching or composite filling. Some patients have moderate fluorosis which requires veneers or an occasional crown[5-8]. Very rarely, patients with severe fluorosis require full occlusal rehabilitation. The protocol for treatment of dental fluorosis has been formulated in this article.
This article documents a case of severe dental fluorosis with intraoral findings such as severe attrition, anterior open bite and unilateral cross bite, which was treated by full occlusal rehabilitation. Novel clinical and technical modifications were employed which may help to simplify the procedure of full occlusal rehabilitation.
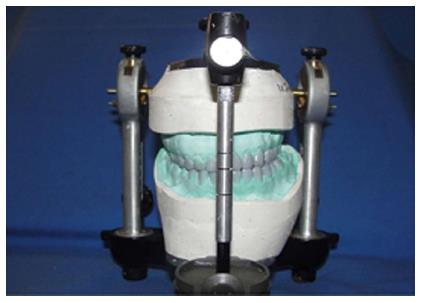
A 28-year male patient reported to the Department of Prosthodontics, with a chief complaint of inability to chew food and discoloration of teeth. A detailed personal history revealed that the patient belonged to one of the fluoride belts of India. Clinical findings included protruded mandible, concave facial profile, severe dental fluorosis (Level 4 on Dean’s Modified Index)[9], maxillary midline not coinciding with mandibular midline, anterior open bite, unilateral crossbite with a few centric stops on left side, generalized severe attrition of teeth with moderate sensitivity (Figure 1). However, there was no loss of vertical dimension which could be attributed to passive eruption to compensate for the attrition. Diagnostic impressions were made using irreversible hydrocolloid (Zelgan 2002, Dentsply, India) and casts poured using dental stone (Kalabhai Karson Pvt. Ltd., India). Face bow (Hanau Springbow, Waterpik Technologies, United States) transfer was done and the casts were mounted using a centric relation record on a semi-adjustable articulator (Hanau H2, Whip Mix Corp, United States). All the clinical findings were confirmed by diagnostic mounting of the casts. Diagnostic wax up was done based on findings of clinical examination, diagnostic mounting and diagnostic wax up. Full occlusal rehabilitation using ceramometal crowns [Meta Cast (V), United States], without changing the vertical dimension at occlusion, was decided as the treatment of choice. The limitations of this treatment option viz., inability to coincide the maxillary and mandibular midline, inability to improve the facial profile and persistence of crossbite on left side were explained to the patient and his approval was obtained for the treatment plan. Maxillary and mandibular anterior teeth were prepared simultaneously to receive individual ceramometal crowns. Impressions were made using Vinyl Polysiloxane (GC America Inc, Made in Japan) by the putty-wash technique[10]. Individual temporary crowns (DPI, India) were fabricated using the indirect technique[11] and were used to establish the anterior guidance in the patient’s mouth in such a way that anterior temporaries provided canine guided occlusion. This was transferred to the semi-adjustable articulator and a custom incisal table was fabricated. The anterior metal try-in was carried out and ceramic (Vita VMK 95, Germany) build up was done according to the anterior guidance obtained from the patient. These definitive anterior restorations were seated in the patient’s mouth, the canine guided occlusion verified and finally the anterior individual crowns were cemented using glass ionomer luting cement (Ketac Cem, 3M ESPE, Germany). The maxillary and mandibular midlines got close but could not be coincided. In the next phase of treatment, all the posterior teeth (maxillary and mandibular) were prepared simultaneously in a single appointment and a centric relation record was obtained. Impressions were made and master casts poured using die stone (Kalrock, Kalabhai Karson Pvt Ltd, India). The casts obtained were mounted on the semi-adjustable articulator. The horizontal and lateral condylar guidances were set arbitrarily at 20o and 15o respectively[12]. The metal copings were fabricated and tried in the patient. Before the ceramic build up was started, the occlusal plane had to be established. This was set at the midpoint between the prepared maxillary and mandibular posterior teeth. After ceramic build up, the definitive restorations were tried in the patient, harmony of centric relation and centric occlusion was verified (Figure 2), canine guided occlusion was confirmed and the restorations were cemented.
Follow up of the restorations and surrounding tissues was done for 3 years. Gingival and Periodontal component of Periodontal Disease Index (PDI)[13] and Plaque component of PDI (Shick and Ash modification) was recorded at the beginning of treatment, every 3 mo for 1 year post treatment and every 6 mo for next 2 years (Figure 3). The Gingival and Periodontal component of PDI score before treatment was 2, in the first year post treatment it was 1 and for the next two years it was 0. Plaque component of PDI score before treatment was 2 and for the next three years it was 1. This indicated high compliance of oral hygiene instructions post-treatment by the patient and successful integration of the restorations in harmony with the periodontal apparatus. The patient expressed satisfaction with treatment and esthetics and restorations were sound and asymptomatic (no sensitivity to heat or cold, no pain/tenderness) at the follow-up visits. This three year follow up has reinforced that the treatment plan was sound and objectives of full occlusal rehabilitation were fulfilled while addressing all the pre-treatment problems of the patient.
Dental fluorosis is seldom so severe[14-16] as to warrant full occlusal rehabilitation. In addition, complexities such as unilateral cross bite on left side, minimum occlusal contacts on right side, anterior open bite (as found in the present case) makes the prosthetic rehabilitation of such a patient challenging. Every attempt was made in this case to provide the best possible functional and aesthetic rehabilitation of the patient.
The dentition in full occlusal rehabilitation cases are restored variously following different principles and philosophies. The canine guided occlusion is the favoured occlusal scheme, most often adopted in full occlusal rehabilitation[17-24]. In this technique, the posterior teeth contact only in centric relation, the incisors are the only teeth contacting in protrusion and the canines are the only teeth contacting in mandibular lateral movements. In this patient, the canine guided occlusal scheme was implemented.
In canine guided occlusion the orientation and location of occlusal plane is not critical as long as it allows the anterior guidance to do its job. In this case, the occlusal plane was planned to be located midway between the prepared posterior teeth. This concept was relatively easy to apply as both the maxillary and mandibular posteriors were prepared at the same time and made the technician’s job much easier. Since the technician received both maxillary and mandibular final casts with prepared posterior teeth, it was easier for her to establish proper contours and height of opposing restorations making optimum use of the available space. This technique is especially advantageous in cases of full occlusal rehabilitation restored using canine guided occlusion. In the present case, a technique has been attempted which simplifies the clinical and laboratory procedures of full occlusal rehabilitation while fulfilling all its objectives[12,25].
The restorative procedures were divided into two components: anterior segment restoration followed by posterior segment restoration. The maxillary and mandibular anterior restorations were fabricated at the same time. Establishing the anterior guidance was also easier. Any adjustments and trimming could be done easily. When the posterior restorations were fabricated, developing the occlusal plane was greatly simplified as both the maxillary and mandibular segments were simultaneously prepared. The occlusal level was then set at the midpoint between the prepared maxillary and mandibular posterior teeth on the articulated casts.
Some occlusal rehabilitation philosophies recommend the restoration of posterior teeth prior to that of anterior teeth (e.g., Hobo Twin-Stage procedure[26] -Conditions 1 and 2). Other philosophies of full occlusal rehabilitation, including the Panky-Mann-Schyuler concept modified by Dawson[12] recommend the sequential restoration of mandibular anterior segment, maxillary anterior segment, mandibular posterior and finally the maxillary posterior segment. The approach discussed in this article is unlike any other philosophies of full occlusal rehabilitation, is simple, requires least number of appointments, is unique and novel, and yet it fulfils all the requirements of full occlusal rehabilitation.
Hence clinical work is greatly simplified and patient appointments are limited to just 6 as follows: Appointment 1: Diagnostic impression, face bow transfer. Appointment 2: Preparation of maxillary and mandibular anterior teeth, impressions, temporization of anteriors. Appointment 3: Anterior metal try-in. Appointment 4: Cementation of anterior ceramometal crowns, selective grinding, finishing, polishing; preparation of all posterior teeth; impressions, face bow transfer, temporization of all posterior teeth. Appointment 5: Metal try-in of posterior restorations; Appointment 6: Cementation of posterior ceramometal crowns selective grinding, finishing, and polishing. Appointment 4 may be split into two depending on convenience of operator and/or patient.
Depending on the Modified Dean’s Fluorosis Index[9] which is the gold standard for quantifying dental fluorosis, a treatment protocol is herewith suggested (Table 1) which is meant as a guide; the operator may follow any treatment modality given in the protocol depending upon the skill-philosophy-convenience-preference.
| Modified dean’s fluorosis index score | Clinical findings | Suggested treatment options |
| Normal (0) | Enamel represents usual transparency, semi-vitriform type of structure. The surface appears smooth, glossy and usually of a pale, creamy white colour | No treatment |
| Questionable (0.5) | Few flecks to occasional white spots | No treatment/bleaching |
| Very Mild (1) | Small, opaque, paper white areas scattered over < 25% of the tooth surface | No treatment /bleaching |
| Mild (2) | White opaque areas in enamel of the teeth are more extensive, but do not involve as much as 50% of the tooth | Bleaching/composite restoration |
| Moderate (3) | All enamel surfaces of the teeth are affected and surfaces subject to attrition show wear. Brown stain is frequently a disfiguring feature | If discolorations accompanied by wear: Full coverage If only discoloration without any wear: 1 Bleaching or 2 Veneers (Direct or indirect) or 3 Bleaching followed by Veneers (Direct or indirect) |
| Severe (4) | All enamel surfaces affected, severe hypoplasia, discrete or confluent pitting. Brown stains are widespread and teeth often present a corroded-like appearance | Full coverage |
The technique of full occlusal rehabilitation illustrated here simplifies the procedures while adhering to all its principles. Rehabilitation of dental fluorosis using the treatment protocol suggested here will systematize and streamline the clinical procedure and it is hoped that this approach will benefit the patient and act as a guideline for dentists.
This is a report of a case of severely discolored teeth, secondary to dental fluorosis; with generalized sensitivity, inability to chew food from both sides and deformed esthetics due to anterior open bite.
The patient had a concave facial profile with severe dental fluorosis (level 4 on Dean’s Modified Index), with prognathic mandible, maxillary midline not coinciding with mandibular midline, anterior open bite, unilateral cross bite with a few centric stops on left side, and severe generalized attrition with moderate sensitivity.
The differential diagnosis can be hypoplasia secondary to trauma to the teeth and jaws, any infections during pregnancy or infancy, poor pre-natal and post-natal nutrition, hypoxia, exposure to toxic chemicals and a variety of hereditary disorders, irregular vitamin D metabolism (vitamin D-resistant rickets) or chronic kidney failure at the time of tooth development.
The tests included intra oral periapical and extra oral panoramic radiographs, diagnostic model mounting, pulp vitality testing of all teeth that confirmed the clinical findings of permanent hypoplastic teeth with sensitivity that were severely attrided and in malocclusion.
Imaging techniques used were orthopantomograph and intraoral periapical radiographs which showed generalized hypoplastic teeth, malocclusion, and anterior open bite.
The treatment given was a full mouth rehabilitation using a specialized, simplified technique which is novel.
All terms are standard and established which have been used empirically.
The approach to a full mouth rehabilitation case has to be holistic, patient specific and should fulfill all the criteria of scientific treatment protocol.
This is an interesting and well written article. Methods are appropriate. Results are clearly presented. Discussion and Conclusions are really interesting.
P- Reviewer: Boffano P, Gokul S S- Editor: Song XX L- Editor: A E- Editor: Wu HL
| 1. | Tabari ED, Ellwood R, Rugg-Gunn AJ, Evans DJ, Davies RM. Dental fluorosis in permanent incisor teeth in relation to water fluoridation, social deprivation and toothpaste use in infancy. Br Dent J. 2000;189:216-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Catani DB, Hugo FN, Cypriano S, Sousa Mda L, Cury JA. Relationship between fluoride levels in the public water supply and dental fluorosis. Rev Saude Publica. 2007;41:732-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Fluoridation facts. Chicago (Illinois): American Dental Association, 2005:29. Available from: http://www.ada.org/sections/newsAndEvents/pdfs/fluorodiation_facts.pdf. |
| 4. | Beltrán-Aguilar ED, Barker LK, Canto MT, Dye BA, Gooch BF, Griffin SO, Hyman J, Jaramillo F, Kingman A, Nowjack-Raymer R. Surveillance for dental caries, dental sealants, tooth retention, edentulism, and enamel fluorosis--United States, 1988-1994 and 1999-2002. MMWR Surveill Summ. 2005;54:1-43. [PubMed] |
| 5. | Akpata ES. Occurrence and management of dental fluorosis. Int Dent J. 2001;51:325-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 36] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Bertassoni LE, Martin JM, Torno V, Vieira S, Rached RN, Mazur RF. In-office dental bleaching and enamel microabrasion for fluorosis treatment. J Clin Pediatr Dent. 2008;32:185-187. [PubMed] |
| 7. | Ardu S, Stavridakis M, Krejci I. A minimally invasive treatment of severe dental fluorosis. Quintessence Int. 2007;38:455-458. [PubMed] |
| 8. | Loyola-Rodriguez JP, Pozos-Guillen Ade J, Hernandez-Hernandez F, Berumen-Maldonado R, Patiño-Marin N. Effectiveness of treatment with carbamide peroxide and hydrogen peroxide in subjects affected by dental fluorosis: a clinical trial. J Clin Pediatr Dent. 2003;28:63-67. [PubMed] |
| 9. | World health organization. Oral health surveys- basic methods. 4ed. Geneva: World Health Organization 1997; 35-36. |
| 10. | Anusavice KL. Phillips’ science of dental materials, 11th ed. WB: Saunders Company 2003; . |
| 11. | Rosenstiel SF, Fujimoto J, Land MF. Contemporary Fixed Prosthodontics. 4th ed. St. Louis: Elsevier Health Sciences 2006; . |
| 12. | Dawson PE. Evaluation, diagnosis and treatment of occlusal problems. 2nd ed. CV: Mosby Company 1989; . |
| 13. | Ramfjord SP. The Periodontal Disease Index (PDI). J Periodontol. 1967;38:Suppl: Suppl:602-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 222] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 14. | Clark DC. Trends in prevalence of dental fluorosis in North America. Community Dent Oral Epidemiol. 1994;22:148-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 83] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 15. | Driscoll WS, Horowitz HS, Meyers RJ, Heifetz SB, Kingman A, Zimmerman ER. Prevalence of dental caries and dental fluorosis in areas with negligible, optimal, and above-optimal fluoride concentrations in drinking water. J Am Dent Assoc. 1986;113:29-33. [PubMed] |
| 16. | Osuji OO, Leake JL, Chipman ML, Nikiforuk G, Locker D, Levine N. Risk factors for dental fluorosis in a fluoridated community. J Dent Res. 1988;67:1488-1492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 122] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 17. | Amico D. Functional occlusion of the natural teeth in man. J Prosthet Dent. 1961;11:899-915. [RCA] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 80] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Scaife RR. Holt JE: Natural occurrence of cuspid guidance. J Prosthet Dent. 1969;22:225-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 51] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Stuart CE. Good occlusion for natural teeth. J Prosthet Dent. 1964;14:716-724. [RCA] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 56] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | McAdam DB. Tooth loading and cuspal guidance in canine and group-function occlusions. J Prosthet Dent. 1976;35:283-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | DiPietro GJ. A study of occlusion as related to the Frankfort-mandibular plane angle. J Prosthet Dent. 1977;38:452-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Goldstein GR. The relationship of canine-protected occlusion to a periodontal index. J Prosthet Dent. 1979;41:277-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 23. | Siebert G. Recent results concerning physiological tooth movement and anterior guidance. J Oral Rehabil. 1981;8:479-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | Belser UC, Hannam AG. The influence of altered working-side occlusal guidance on masticatory muscles and related jaw movement. J Prosthet Dent. 1985;53:406-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 78] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 25. | Michael DW. Failure in the Restored Dentition: Management and Treatment. Tokyo: Quintessence Publishing Cpmpany 1995; . |
| 26. | Hobo S, Takayama H. Oral rehabilitation clinical determination of occlusion, 1st ed. Tokyo: Quintessence Publishing Company 1997; . |