Published online Dec 16, 2014. doi: 10.12998/wjcc.v2.i12.757
Revised: October 22, 2014
Accepted: October 31, 2014
Published online: December 16, 2014
Processing time: 128 Days and 9.2 Hours
In the current socio-economic scenario characterized by a growing shortage of resources and progressive budget constraints, the need to better coordinate processes in health institutions appears as a relevant aspect to ensure the future sustainability of system. In this sense, Relational Coordination (RC) provides a valuable opportunity for the reconfiguration of clinical guidelines concerning isolated single-level considerations. In this research the RC model has been applied to explain best results in the process of diagnosing and offering clinical treatments for lung cancer. Lung cancer presents the higher rates of tumor’s mortality worldwide. Through unstructured and informal interviews with clinicians at both levels (Primary/Specialist Care), a diagnosis of the situation in relation to joint management of lung cancer is provided. Solutions of continuity in terms of coordination are explained due to the observation of lack of effective knowledge transfer between the two levels. It is this disconnection which justifies the introduction of a modified model of RC for the study and implementation of transfer relations between the knowledge holders, in order to structure consolidated and cooperative evidence-based models that lead to a substantial shortening in the response times with a marked outcomes improvement. To our knowledge, the application of this model to a Public Health problem bringing together both levels of care, hasn’t been made till now.
Core tip: Innovative managerial frameworks have to be put into practice when treating severe diseases. Relational Coordination makes possible to enhance inter-level knowledge networks to obtain better outcomes from the perspective of the National Health System and the patients. Through systematic revision, it has been checked that only in the fields of Endocrinology and Psychiatry have these frameworks been applied. This model tries to establish a coordinative solution within the field of Oncology, implementing the Theory of Relational Coordination as a tool to get optimal results in lung cancer.
- Citation: Romero JAV, Señarís JDL, Heredero CDP, Nuijten M. Relational coordination and healthcare management in lung cancer. World J Clin Cases 2014; 2(12): 757-768
- URL: https://www.wjgnet.com/2307-8960/full/v2/i12/757.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v2.i12.757
In the current schemes of complex pathologies management, collaborative scenarios are required in order to get to an integral coordination of health problems via multi-level strategies[1-3]. This statement acquires higher importance once we consider some concrete disease processes that, due to their increasing incidence and associated costs from both the patient’s and the National Health System’s (NHS) perspective, constitute core objectives for specific interventions that may reduce time to take accurate decisions headed to resolute, chronify or minimize the pain caused by the disorder. Coordination networks building and optimization of multi-level tacit knowledge transfer, would provide cost containment per patient stay to the NHS and to the social welfare system, contributing this way, to increase Quality Adjusted Life Years decreasing, as well, Disability Adjusted Life Years.
The objective of this study is to apply the Relational Coordination (RC) Model[4-6] to a determined health problem in order to implement the appropriate treatment trajectories based on continual permutation of actions[7] that return positive outcomes on the indicators formerly mentioned. Although, as far as we know, this model has proven very good results in hospitals, nothing has been performed using this model to check out the effectiveness of coordination strategies between levels of care, when considering the design of common pathways to treat successfully neoplasia as a serious Public Health concern.
To enforce this objective, lung cancer has been selected as an example of great relevance disorder. This is due to: its really important Disease Load[8,9], high treatment cost[10,11], social coverage of disabilities, side-effects on productivity[12], assistance discontinuity between Primary (PC) and Specialized Care (SC)[13] and lack of common recognized procedures and pathways between them and within every isolated level.
This study is focused on comparing actual circuits that patients from PC follow until they get to their reference hospital (in this study we consider a high complexity one, Beveridge typology within a National Health System, with its made-to-measure design of Lung Cancer Clinical Pathway), with our proposal of modified, multilevel RC model applied to clinical trajectories that permit assistance continuity.
As a consequence, it is absolutely necessary to build a clinical alert system triggered by proven suspicion of neoplasia. This needs to be in accordance with the next healthcare level (SC) to, under the premise of evidence-based clinical practices, develop quick completion check-lists that enable immediate[14] transference of patients to the adequate level, using information technologies as preferred communication channel[15,16].
With respect to inter-level coordination, we can highlight that this is not a clinical routine. As scientific literature points out, this cooperative strategy is put into practice by medical specialties not or discretely related to Oncology, such as Endocrinology o Psychiatry. Actually, we find no evidence of cooperative inter-level strategies being carried out in the field of Oncology[17]. Difficulties in structuring these kinds of practices lie on the basis of knowledge transfer[18,19] in organizations characterized by the dominance of its tacit component[20,21] that rarely show High-Performance Work Systems (HPWS) practices[22]. Furthermore, organizational designs for effective and efficient management of oncologic diseases have to be both adaptative and dynamic[23] to be aligned with the state-of-the-art advances recognized in gold standards.
To this respect, RC appears as a high-traceable bidirectional tool to provide excellence in neoplastic lung disease treatment. The model theorized by Gittell[5] offers a global coordinative vision of the organizational process, helping to figure out inefficiencies that can be corrected by initializing and implementing cooperative practices and, as a result, proactive organizational designs that tend to rationalize use of resources. Additionally, it contributes to establish optimal relational dimensions for potential efficiencies of scale and scope depending on the attributes of relational and intellectual capital within the organization[24-27].
A noteworthy aspect of the suitability of the model of choice is supported by the complement that offers for the integration of related scientific approaches within the field of Business Organization, such as Operational Management. This will allow the development of further studies to refine reengineering process via supply-chain, thus contributing to the optimization of both the intermediate (surrogate-end-points) and the final results observed in patients (outcomes), and in the income mediated by Risk Adjustment Systems[28] used in health financing. Thus, if the inefficiencies inherent in the coordination process of the disease are debugged, additional financial returns (based on capitation criteria related to the number of processes) could be achieved (even from the health organization’s perspective with regard to cost-efficiency). Another feature that makes Gittell’s[5] model ideal for our purpose, is that it previously develops a series of tables analyzing HPWS practices, correlating its absence or presence with RC and, consequently, with final outcomes. Thus, the same model before being implemented, allows a diagnosis of the situation in terms of the practices mentioned. Once conclusions resulting from field work have been extracted, the implementation of the model can lead to the development of the absent figures, resulting in a multidirectional dynamic feedback identifiable with the continuous improvement cycle[29].
Moreover, and in a methodological approach, given the intangible nature of the concepts that promote operational developments in the organization as well as their interaction and mutual influence, the model enables the application of multivariate analysis techniques focused on structural equations. This has the potential to provide greater rigor and validity when checking the assumptions in a context of real research.
In addition, via RC valuable information it would be possible to extend the network (regarding the possibility of generating “Value Networks”[30] in the process) to other stakeholders such as pharmaceuticals and health technology companies, and even to managerial superstructures committed on public health concerns.
Incorporating the principles of Business Organization to the clinical setting is absolutely essential to promote the reduction of redundant, iterative processes in traditionally knowledge intensive organizations. These have ignored their role as business managers of a huge amount of resources, in interest of a pretended clinical excellence oriented to complex phenomenology and high media impact in terms of prestige, influence and fund raising, but with little residual value in the generation of efficiencies of scale and scope, given the peculiarities involved in tertiary healthcare.
Given the above, the model postulated by Gittell[4,5] having been tested previously[6] in these types of organizations, is an excellent reference for the detailed study of the relationships involved in designing healthcare procedures between the different levels. It provides the basic tools for understanding and constructing a single treatment line that does not register any undesirable delays attributable to gaps in knowledge and other factors, including relational. The model also facilitates the continuous review of the adequacy of the approaches proposed and its comparison with reference standards in relation to screening, extension study, staging, treatment, monitoring and rehabilitation of lung neoplasia.
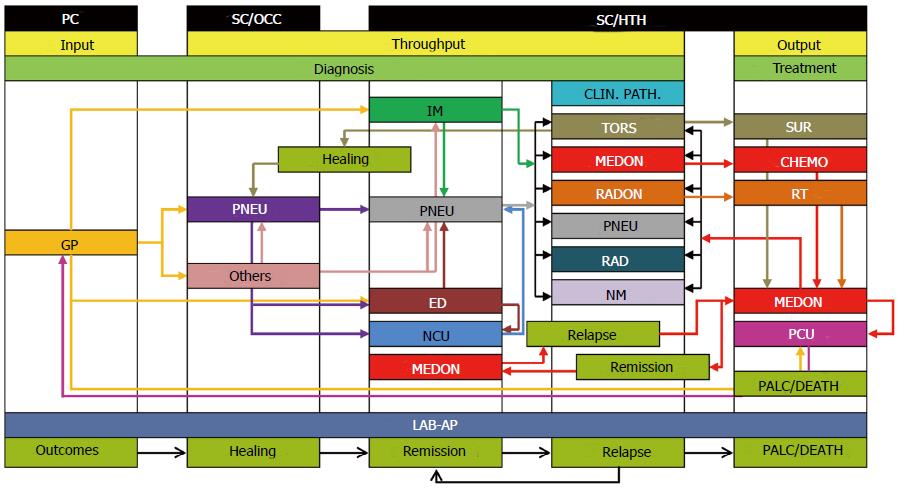
Before accessing the clinical pathway itself, there are many routes to be made by patients in their journey between the two levels of care. This route identifies itself with the diagnosis and treatment of the disease, and represents the transition between access to primary and secondary healthcare (Figure 1). For operational reasons, it excludes access to tertiary level (rehabilitation).
To carry out the process map, unstructured interviews during the months of March, April and May 2012 have been developed with Pneumologists and General Practitioners (GP), as key agents in the user’s address to the specific resources for diagnosis and treatment.
The patient’s contact with the system starts at the level of PC in the Health Center, where the person requests for consultation to GP due to a series of signs and/or symptoms which may be more or less related to tumors. At this point, a series of basic tests as conventional radiology and blood analytics are required. It is here, where they may be starting to produce the first delayed diagnosis attributable to the transfer of knowledge not based on evidence, since these blood tests not always include non-specific tumor markers, but indicators of malignancy. Furthermore, in many cases, treatment is initiated based on empirical diagnosis of pneumonia, since the neoplastic process can be masked or not being clearly visible by conventional radiology.
From this first GP visit, a second one is requested for reevaluation of improvement and/or worsening of the patient. Also in this second visit, imaging and laboratory results are delivered. This time period can vary from one week to fifteen days (period in which the empirical treatment of antibiotic action produces noticeable changes in the patient’s condition and laboratory data). At the persistence of symptoms or onset of signs clearly suggestive of clinical suspicion, inter-consultation part is issued to the specialty of Pneumology (SC) based at an Outpatient Care Center (OCC). This will lead to an additional delay, although it may be attenuated in case of emergency.
While the above, it should be noted that this path is followed if the clinical manifestations clearly compromise the patient’s respiratory status. However, there are not always reliable evidences of pathology as they may be semi-hidden or produce “a priori” events unrelated to the disease. This can lead to other specialties not specifically connected with the process, due to the absence of effective knowledge transfer between levels.
Consider, for example, the case in which the disease is indirectly manifested through referred pain in locations as knee or scapula, with inconclusive imaging tests and non-specific tumor markers requested either. In this case, when a person with referred pain consults GP and also has a history of degenerative joint disease, the first inclination is based on the therapeutic application of trauma imaging at the involved location. If this do not show alterations, to an extension diagnosis, the patient maybe referred to other specialties, via interconsultation, at the level of OCC, as may be Rheumatology or Traumatology (again, we would have another delay in the issuance of a firm diagnosis). To this must be added, the additional delay in the appointment date for new consultations, delays in the completion of tests that are to be applied in these services and the appointment date for review. Note, that the pain reported by the patient could be produced as a result of neurological compression due to tumor growth.
Once the presence of specific pathology related to other specialties different to Oncology is ruled out, and for a possible occurrence of respiratory and/or systemic signs, the patient may be referred back to the GP (who will likely refer the patient to another specialist in the short-term, as for example an Internal Medicine practitioner at the hospital level) or Pneumologist at OCC level.
It is vitally important to consider that these successive accumulated delays entail delayed diagnosis and may incur progression of the disease from an early stage potentially curable, to an irreversible stage where only palliative measures can be adopted.
Special mention deserves the situation in which the patient attends a first GP consultation when the disease is in an advanced stage. In this case, the GP may take two decisions: one would be immediate referral to the reference hospital emergency department. The other one would be derivation, equally immediate and avoiding waiting list, to Pneumology at OCC.
The tours in both situations are as follow. In the case of referring the patient to the high-tech hospital emergency department considered for the study, the user would be admitted in the lower course of time. Alternatively, the physician at SC may order scheduled or urgent admission according to his criteria, and even via emergency if the clinic is accused and limiting.
Returning to the circuit in which the disease is not clearly delimited, and placing the patient back to Pneumology at OCC, application of tumor markers and more specific diagnostic imaging tests with their corresponding waiting times will be issued. This will finally lead to a first diagnosis of neoplastic disease, although in many cases progress is relentless, having passed the tipping point between curability and elongation of survival.
Once the diagnosis has been confirmed (after issuance of radiological and pathological opinion), the Pneumologist at OCC (based on clinical signs) will apply for patient admission at the Respiratory Unit at the reference hospital or at the Neoplasia consulting Unit (staffed by Pneumologists), also located at the hospital but belonging to the outpatient section (OCC/HTH), who predictably will speed his admission to the Respiratory Unit.
It has to be taken into consideration that, as reflected in Figure 1, in cases of nonspecific symptoms the GP or the specialist physician from other disciplines different to Pneumology, can request patient admission at an Internal Medicine Unit. Once there, and after confirming diagnosis, the patient will be placed in charge of the service consulted (Pneumology) or included directly in the clinical pathway in order to be admitted to the Respiratory Unit.
As it has been explained, to reach this clinical decision, the circuits followed by patients are often redundant and inefficient incurring incremental health expenditure and associated loss of productivity, with the aggravating factor of disease progression, which dramatically affects the effective resolution of the process due to a probability increasing of metastatic dissemination. The next step is the inclusion of the patient in the clinical pathway itself.
The Clinical Pathway Commission is a multidisciplinary board delegated by the Chief Medical Officer of the hospital, whose mission is to take collective decisions about the individualized treatment for each patient given the specific types of lung neoplasia presented. It consists of various clinical services such as Thoracic Surgery, Oncology, Radiation Oncology, Pneumology, Radiology and Nuclear Medicine, and meets in session once a week to discern treatment strategies addressing cases that present criteria for inclusion.
Previously, and once the patient has already been admitted in hospital, sequential examinations to limit the spread of the disease and rule out metastasis are conducted.
Once all results are available, which will generate a new lengthening of waiting times due to internal procedures, they are presented in clinical session to elucidate what the best combination of medical and surgical options is. In this regard, it is noteworthy to point out several strategies that, in turn, generate new decisional and time-restricted flows around the patient.
First, and once the kind of broncho-pulmonary neoplastic lesion is typified, in case that the option of surgery is the one chosen, the patient is transferred to Thoracic Surgery (which acts only in relation to the surgical process) being the customer the Respiratory Unit. Upon resolution of this action, the patient can follow two routes depending on the characteristics of the disease. If the lesion was curable with just surgery, if it is in a nearly stage, the subject is again brought back to the customer service where periodic reassessments continue on an OCC basis. If clinical pathway was structured in a combined plan of several therapeutic strategies, the patient will be assigned to Medical Oncology and submitted to treatment schemes consisting of chemotherapy and/or radiotherapy (if appropriate), acting as coadjutor service, Radiation Oncology.
Following this, we have to clarify the types and purposes of cancer treatments and their relationship with Thoracic Surgery, as well as with the alternative circuits of patients arising as a result. These treatments can be neoadjuvant or adjuvant. If a neoadjuvant treatment is preferred, the patient will be referred to Medical Oncology from Pneumology, where after receiving the appropriate treatments, will be referred to Thoracic Surgery, and once its performance has concluded, he will be returned to Medical Oncology where the patient will ultimately be assigned. If the adjuvant treatment option was considered, the bypass sequence would start from Pneumology to Thoracic Surgery and from the latter to Oncology, where, likewise, the patient would stay finally allocated.
In the case (very common) that Radiation Oncology intervenes, the customer service would be Medical Oncology, and the role of Radiotherapy would be the imposition of costs derived from treatment processes to the original customer.
While all of the above, it is another distinct possibility in case the lesion is unresectable. In this situation, the Commission may choose the administration of chemotherapy and/or radiotherapy to ensure the stabilization of the process. In this sense, the patient is finally moved to Medical Oncology where clinical decisions and treatments are provided, appearing again the interactions described above for the Radiation Oncology department.
After running all the steps above, the circuit would continue in different ways to transfer responsibilities between services and even between levels, depending on the clinical outcome. Thus, we would obtain the following sequences: (1) healing: The patient would return to Pneumology at the OCC level for regular checkups; (2) remission: If partial or complete remission, the patient would be discharged and would attend appointed checkups at Oncology Day Hospital (OCC/HTH); (3) relapse: In this case, the patient re-enters in charge of Medical Oncology, without his case again be subjected to clinical pathway for application of second-and subsequent lines; and (4) palliative Care/Death: For unsolvable progression of the disease, the patient is transferred from Medical Oncology to Palliative Care Unit (PCU), where treatment is merely symptomatic. Nevertheless, depending on the patient’s general condition and in respect of his decision making capacity (if this was preserved or had been previously stated), the patient can be treated at home through a collaborative partnership between PCU (SC) and GP.
Restructuring of patient inter-and intra-level flows is absolutely needed. It requires corporate collaborative systems providing knowledge to one medical act. Therefore, the role of the RC model acquires great relevance as it acts as mediator and promotor of joint strategies aimed at improving results ,from both, the patient’s and the NHS’ viewpoint.
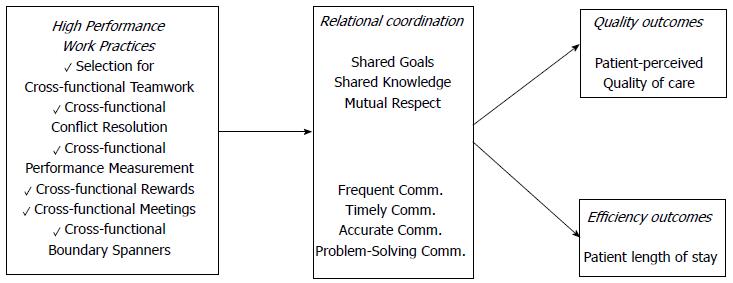
Based on previous studies grounded in mutual adjustment[31-35] and coordination approaches based on relationships[14,36-40] in corporate environments of high/low interdependence/uncertainty, Gittell develops her model (Figure 2) as a contribution to the study of relational dynamics.
In this sense, Gittell[5] defines her model as a mutually reinforcing process of interaction between communication and relationships carried out for the purpose of task integration. She also states that her theory differs from others due to the proposition of three specific relational dimensions that are necessary for effective coordination.
While many other recent theories emphasize the importance of shared knowledge, RC argues that while this is necessary, is not sufficient. Accordingly, to achieve effective coordination, the members must also be connected through the possession of shared goals and mutual respect.
As mentioned in the previous section, role-based coordination has an advantage over coordination based on personal ties. While the former may require more investment for being implemented, role-based coordination fosters a role exchange that encourages corporate flexibility to adapt to changing environments within a high uncertainty and interdependence frame over time.
The model is structured around two types of dimensions: Communication and Relationship.
Within the dimensions of communication, we find: (1) frequent communication: Frequent communication helps to establish relationships among roles through the closeness generated as a result of repeated interaction[5]; (2) timely communication: Delays in communication may have negative implications for organizational performance. Hence, the importance of timely communication, and at the right time, for successful development of organizational tasks[41]; (3) accurate communication: Accurate communication, regarding the content of relevant information, plays a critical role in the effectiveness of group tasks performance[42]; and (4) problem-Solving communication: Effective coordination requires that those involved in the task, engage in communication to solve the problems that appear in a group performance characterized by high interdependence (rather than blame others involved or evading the responsibilities). This can lead to negative consequences that singularly affect performance[29].
Within relational dimensions in Gittell’s model we find: (1) shared goals: This aspect plays a key role on the coordination of highly interdependent tasks[43,44]. Using a set of shared goals regarding the work process, involved individuals develop ties that allow them to reach conclusions that are compatible with the different ways of thinking and acting as new information is available[5]; and (2) shared knowledge: While Dougherty[45] points out that communication among those involved in the various tasks that constitute a process is not always effective because of different social backgrounds, training and/or experience, Gittell[5] states that when members know how their tasks are related to other members within the same process, it creates a dynamic in which everyone knows the impact that each change will reflect on each task and each role; and (3) mutual respect: Respect for the competence of others involved in the process, provides a powerful tie that will be implemented in a comprehensive way across the whole process generating, as a result, an effective coordination[5].
Through this design, it follows that the RC model turns into a model of intensive coordination in communication and relationships, particularly useful to achieve higher levels of performance under high levels of interdependence among tasks, uncertainty and time constraints. So, it is an example of process improvement that allows a work group department or organization, raise their production possibility frontier to more favorable positions while achieving higher efficiency and quality[5].
It is, therefore, to achieve work processes improvement through improving the quality of labor relations among the actors that play different roles in these processes, thus leading to a higher quality of communication. Through this procedure, it is intended to reduce errors delays and redundancies observable among tasks interdependences within the critical organizational processes.
Model measurement is done through validated surveys to participants in a given process, on the activities of communication and relationships with others involved in the same process, with whom relations of interdependence are kept for achieving the same common objective. Related to the above, the first step would be the selection of a work process that serves a population of interest. Then, the roles or functional groups embroiled in the development of the focal process must be identified. The third step would consist on identifying which of those groups could be accessed by the researcher in order to develop matrices (symmetric/asymmetric) of RC links.
Once the previous steps have been run, likert-type survey would be delivered to the participants consisting of seven questions: four on communication and three concerning relations between different process roles. In order to reduce possible bias attributable to socially desirable responses, RC’s survey asks participants about behaviors of other roles, except for organizational behavior feature represented by the frequency of communication. In addition, questions are referenced to habitual patterns of behavior, rather than be directed towards identifying specific events, that are part of the current patterns in the time of evaluation. Thus, avoiding erroneous response patterns based on retrospective response biases.
The characteristics of the model applied to the investigation of coordination practices in the management of interdependent processes, allow multi-functionality in analytical and exploratory orientation, presenting four complementary and inclusive perspectives that give great versatility in building research designs. Thus, the model can be used with the next main purposes: (1) analysis of the effect of RC on organizational performance: Determination of the impact of the model on improving the quality and efficiency of a given process characterized by high levels of interdependence, uncertainty and time constraints; (2) analysis of predictive factors of RC: Determination of the effects of organizational practices to use on the model; (3) analysis of the mediating effect of RC: Determination of the influence of the model on existing organizational practices and their impact on results; and (4) analysis of the moderating effect on RC: Determination of the influence of a/some given factor/s on the effect of the model on organizational performance measurement.
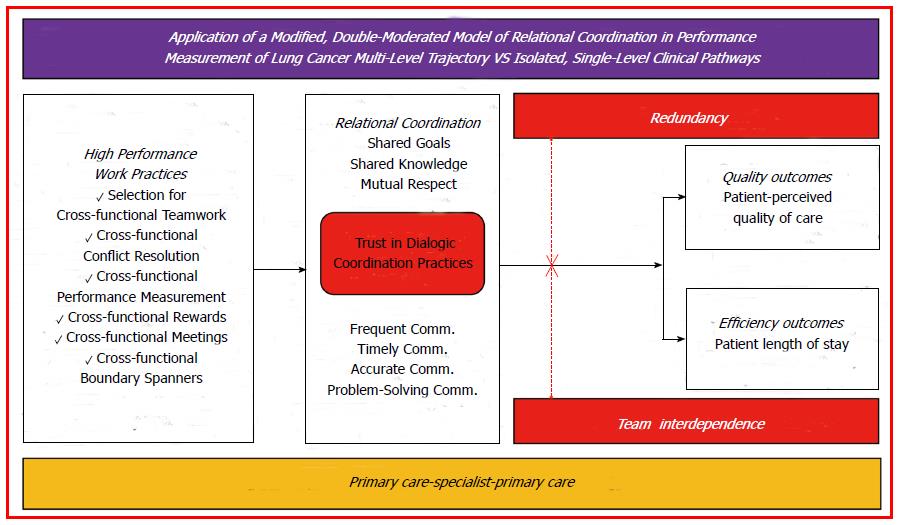
Next, we describe the proposed model for this paper based on RC modified at its core by adding two features of organizational behavior that are interrelated. Also, we introduce two moderating factors to analyze the mediating effect of it and its impact on organizational performance, taking as a critical process multilevel management of health institutions in relation to lung cancer. To increase consistency and operational development in the future, a comparison with institutional practices currently applied (particularly single level clinical pathways) is made.
APPLICATION OF A MODIFIED, DOUBLE-MODERATED MODEL OF RELATIONAL COORDINATION IN PERFORMANCE MEASUREMENT OF LUNG CANCER MULTI-LEVEL TREATMENT TRAJECTORY VS ISOLATED, SINGLE-LEVEL CLINICAL PATHWAYS
As it has been previously described, the main objective of this paper is the proposal of a modified, double-moderated model of RC (Figure 3), to investigate the degree of development of the theory proposed by Gittell[5] and the impact of its implementation on HPWS practices and outcomes obtained by the institution. In reference to the above, the greatest achievement of this study is supported by theoretically increased times of disease-free survival (DFS) as a consequence of optimal-efficient redesign of coordination strategies between levels involved in diagnosis and treatment. In addition, the potential gains highlighted would imply healthcare costs containment that would return positive savings on other important health problems, being possible to achieve true clinically-oriented corporate strategies.
First, and as a previous step for defining the implications of the proposed model on performance, we need to identify HPWS practices currently observable at health organization level (Table 1) and at the level of diagnosis and treatment of broncho-pulmonary carcinoma (Table 2) for both care providers (PC/SC).
| HPWS Practices | Level | ||
| PC | SC | Inter-level | |
| Selection for Cross-Functional Teamwork | Health Plans | Clinical Pathway Commission Hospital Commissions | Non-existent |
| Cross-Functional Conflict Resolution | Managing Director at Primary Care Center | Hospital Board of Managers | Deputy Medical Care Continuity (Since October 2010) |
| Cross-Functional Performance Measurement | Primary Care Center | Clinical Units | Non-existent |
| Cross-Functional Rewards | Professional Categories at Primary Care Center (Pre-established at 100% Objective Compliance) | Professional Categories at Clinical Units (Pre-established at 100% Objective Compliance) | Non-existent |
| Cross-Functional Meetings | Primary Care Center | Hospital Board of Managers, Hospital Technical Commissions, Medical Services Commissions | Health Area Managing Board |
| Cross-Functional Boundary Spanners | Managing Director at Primary Care Center | Hospital General Manager | Deputy Medical Care Continuity (Since October 2010) |
| HPWS Practices | Level | ||
| PC | SC | Inter-level | |
| Selection for Cross-Functional Teamwork | Non-existent | Clinical Pathway Commission | Only at Palliative Care Level |
| Cross-Functional Conflict Resolution | Non-existent | Clinical Pathway Commission/Chief Medical Officer | Non-existent |
| Cross-Functional Performance Measurement | Non-existent | Clinical Pathway Commission (No. of patients included in the clinical pathway) | Non-existent |
| Cross-Functional Rewards | Non-existent | Non-existent | Non-existent |
| Cross-Functional Meetings | Non-existent | Clinical Pathway Commission | Non-existent |
| Cross-Functional Boundary Spanners | Non-existent | Clinical Pathway Commission | Non-existent |
As seen on Table 1, HPWS practices in the health care organization have a wide variability and segmentation that result in continuity of care disconnection. Furthermore, the absence of inter-level operational relations in critical aspects emphasizes the fact pointed out, generating a discontinuity of the care process that could lead to very significant increases in transaction costs, as well as duplication of health expenditure and intangible consumption.
This situation is much more serious when looking at data provided in Figure 2, referred to the specific coordination process of the pathology. In this case, it highlights the virtual absence of joint strategies for the management of the disease. In light of this information, the existence of redundant and iterative processes (that create delays in the effective application of therapeutic measures associated with consequent costs due to disabilities and/or productivity losses), gets verified.
The comparison of data shown in Tables 1 and 2 has been made through unstructured interviews with senior doctors at a health center, which has as reference hospital the one mentioned throughout this work, and that is very representative due to the volume of population served (approximately 22000 health cards).
It justifies the introduction of a modified model of RC for the study and implementation of transfer relations among knowledge holders, in order to structure consolidated, evidence-based cooperative models that would lead to a substantial shortening of response times with a marked improvement in outcomes.
The sequential development of our model is based on the examination of the organizational behavior considered by Gittell, using the methodology annexed to the theoretical approach[5]. Then, it will be complemented by a combination of studies of other authors in the field of management, which postulate the study of trust relationships[21,46] and dialogic practices[14] as effective methods of organizational coordination.
These are especially relevant for high-uncertainty processes requiring quick and adaptative replies.
Related to the above, trust is a predictor and a consequence of interpersonal relationships[21]. In this sense, a higher degree of trust acts as a stimulating factor for communication accessibility, promotes greater effort from those involved in a task and reduces conflict in work teams, fostering better results in performance[47,48]. It could be inferred that it acts as an enhancer of RC.
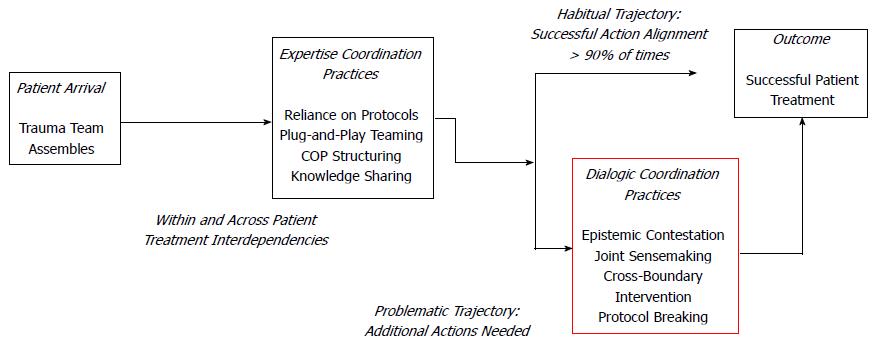
Moreover, dialogic practices tested in high-uncertainty hospital services[14] appear as coordinative solutions (from a point of view focused on process trajectories[7]), by which cooperative guidelines are structured (Figure 4). This fact is particularly important, given the high variability inherent to the process of diagnosis and treatment, and the consequences of a not entirely optimal assembly of tasks committed with the successful resolution within a framework of time-coordinated action.
Related to approaches focused on trajectories[7], these are described as goal achievement oriented sequences of action that emphasize contingencies and interactions among those involved in, differing from routines in that the latter merely emphasizes a sequence of steps that can’t be extrapolated to work situations characterized by novelty, unpredictability and changing environments in relation to tasks, actors and resources[14].
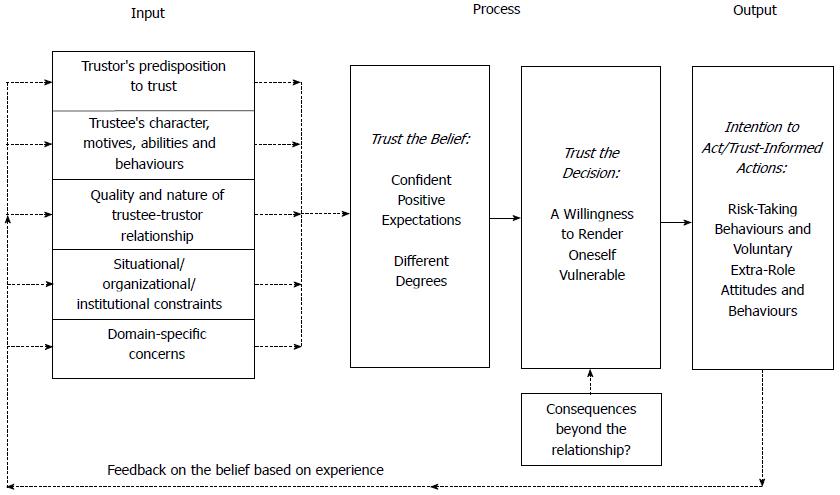
So, it is about measuring the degree of trust that the different professionals at both levels have in dialogic practices, following the methodology used by Dietz and Hartog[46] (Figure 5). This evaluation methodology would be applied to the PC level on the SC level and vice-versa.
In a structured way, it would be done a pre-test evaluation of the RC status (for a given level of trust in dialogic practices) at an early stage at both levels, applied to the target health problem. These data would be correlated with the evidence about HPWS developments.
Subsequently, a series of actions would be designed to strengthen relational ties between the two levels. For example, formal assistance on regular basis of one PC-GP to the meetings of the Clinical Pathway Commission (SC), with the aim of promoting the practices mentioned as of excellence, can be suggested. As a consequence, the development of inter-level HPWS practices would be promoted, development that could materialize in creating joint Clinical Practice Guidelines which would contribute to early detection of lung cancer.
Furthermore, to streamline the circuit followed by the patient, direct referring to specific knowledge resources located on SC is intended, always ensuring the traceability of the patient’s health status via widespread use of shared databases.
In this sense, it is about promoting the representativeness of the Continuity of Care Coordinator (see Table 1) in bidirectional management of patients affected.
Secondly, the interdependence of tasks generated under the prism pointed by Van de Ven et al[35] would be considered in terms of work flows at the team level. Participating GP’s would be enrolled in a training program of High-Fidelity Clinical Simulation following a methodology of Objective Structured Clinical Examination[49-51] that would be taught by specialist physicians specifically trained in this type of methodology. Once these actions have been carried out, a new post-test measure of the degree of trust in RC and dialogic practices would be done at the same time that HPWS practices are re-evaluated.
From this point on, it is necessary to evaluate (retrospectively/prospectively) the time passed since the first contact with the system takes place until the patient receives the first therapeutic action for treatment, prior to and after the implementation of measures aimed at encouraging the development of RC and dialogic practices. Also, as a control measure that would reinforce the theoretical assumptions (raised by some a priori confirmatory hypotheses for the model proposed vs. single level clinical pathways), TNM staging category (at the time of diagnosis confirmation) and estimation of DFS would be done. In closing, costs related to hospital stays savings (as a result of early detection) would be calculated.
The proposed model goes from an exploratory qualitative design to (after an inductive process) an explanatory type, which generates synergies in the use of scarce resources through coordinative economies of scope.
In the current socio-economic scenario characterized by a growing shortage of resources and progressive budget constraints, coordinated process management in health institutions appears as a relevant need to ensure the sustainability of the medium/long term.
The fact that a health system is strategic for a country (particularly if this system is public and universal), together with the sheer volume of resources associated with healthcare provision, makes mandatory to impose a rational logic in the clinical management of public health concerns. This logic has to be even more intense, when it comes to diseases on the rise and rate of disability and/or mortality as the one we are considering in this paper.
In this sense, RC provides a valuable opportunity for the reconfiguration of clinical guidelines concerning isolated single-level considerations, to turn them into cooperative inter-level ones.
Through unstructured and informal interviews with clinicians at both levels (Primary/Specialist Care), diagnosis of the situation in relation to joint management of lung cancer is made, noting that solutions of continuity (in terms of coordination) are observed due to the lack of effective knowledge transfer between the two levels as a result of RC practices absence[52].
Is in this way, where it is theoretically inferred that delays secondary to ineffective coordination would be attenuated if launching and implementation of cooperative schemes (including relational trust in dialogic practices) had been run. In turn, these strategies would result in the generation of “ad hoc” Clinical Practice Guidelines (equivalent to HPWS in other corporate environments), which would strengthen the mission of RC. In this regard, it is worth highlighting the flexibility provided by Gittell’s theory[5]. It allows adaptation and modeling of its precepts to the organizational conditions of actual practice, providing a specific management architecture for knowledge intensive organizations that remains under heavy pressure on casuistic, uncertainty and technological changes.
The model proposed in this research, advocates a regularization and training of new skills and relational attitudes arising from the collaboration between the two levels of care involved. This consideration is particularly relevant if we return to the defining characteristics of health systems in which advances in the state of the art occur constantly and must be properly transferred.
The operational implications of the suggested theoretical alternative pursue a dual purpose on results. So on the one hand, facilitating diagnosis in early stages of broncho-pulmonary carcinoma, allows more cost-efficient measures, which will return a decrease in rates of morbidity and mortality and a significant reduction in opportunity costs from the patient’s point of view. This would be translated into tangible gains in DFS and the appearance of negative costs obtained from savings in productivity loss avoiding and containment of hospital stays per process.
On the other hand, the second approach is characterized by the impact on health spending of Medical Care Variation. Because physicians are resource allocators, this scheme of coordination is intended to reduce duplication in diagnostic tests and clinical times. Here appears again the concept of opportunity cost, but in this case, from the point of view of the NHS. If the process is clearly predefined, there would be a bidirectional action sequence that would lead up to a regulated and bottom-up asset allocation from an optimum-efficiency criteria based on clinical excellence and non-repetitive processes. The savings generated by this approach can, in turn, be reinvested in the process itself or moved to other singular processes of great clinical significance.
The research model is, therefore, to efficiently redirect health expenditure incurred by the disease through proactive inter-level and inter-professional coordinative solutions, achieving, this way, improvements in quality of life and survival of patients affected.
It should be noted that the health organization is not to stay longer away from the improvement proposals dropped from the corporate world, because it is in itself a great company if we pay attention to budget, employability and management processes underlying their daily operation.
In this sense, this document is made taking into account the feasibility and methodological orientations arising from the healthcare business world and academia, providing a new strategic vision of the organization of clinical processes in high complexity health corporations.
P- Reviewer: Kawai H, Sugawara I, Wang HY S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Canino G, McQuaid EL, Rand CS. Addressing asthma health disparities: a multilevel challenge. J Allergy Clin Immunol. 2009;123:1209-1217; quiz 1218-1219. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 172] [Cited by in RCA: 167] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 2. | McMahon T, Gallagher RM, Little D. Psychiatry--family practice liaison: a collaborative approach to clinical training. Gen Hosp Psychiatry. 1983;5:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Wagner EH, Glasgow RE, Davis C, Bonomi AE, Provost L, McCulloch D, Carver P, Sixta C. Quality improvement in chronic illness care: a collaborative approach. Jt Comm J Qual Improv. 2001;27:63-80. [PubMed] |
| 4. | Gittell JH. High performance healthcare: using the power of relationships to achieve quality, efficiency and resilience. New York, NY: Mc Graw-Hill 2009; . |
| 5. | Gittell JH. Relational coordination: guidelines for theory, measurement and analysis (Internet) 2010 (accessed 2013 May 23). Available from: http://rcrc.brandeis.edu/downloads/Relational_Coordination_Guidelines_8-25-11.pdf. |
| 6. | Gittel JH. Coordinating mechanisms in care provider groups: relational coordination as a mediator and input uncertainty as a moderator of performance effects. Manage Sci. 2002;48:1408-1426. [DOI] [Full Text] |
| 7. | Strauss AL. Continual permutations of action. Hawthorne, NY: Aldyne de Gruyter 1993; . |
| 8. | Globocan, (IARC). Section of Cancer Information (Internet). World Health Organization. Hawthorne, NY: Aldyne de Gruyter 2008; (accessed 2013 May 23) Available from: http://www.who.int/. |
| 9. | Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet. 1997;349:1498-1504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4227] [Cited by in RCA: 4048] [Article Influence: 144.6] [Reference Citation Analysis (2)] |
| 10. | Warren JL, Yabroff KR, Meekins A, Topor M, Lamont EB, Brown ML. Evaluation of trends in the cost of initial cancer treatment. J Natl Cancer Inst. 2008;100:888-897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 277] [Cited by in RCA: 302] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 11. | Yabroff KR, Lamont EB, Mariotto A, Warren JL, Topor M, Meekins A, Brown ML. Cost of care for elderly cancer patients in the United States. J Natl Cancer Inst. 2008;100:630-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 503] [Cited by in RCA: 562] [Article Influence: 33.1] [Reference Citation Analysis (0)] |
| 12. | Bradley CJ, Yabroff KR, Dahman B, Feuer EJ, Mariotto A, Brown ML. Productivity costs of cancer mortality in the United States: 2000-2020. J Natl Cancer Inst. 2008;100:1763-1770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 181] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 13. | Safran DG, Miller W, Beckman H. Organizational dimensions of relationship-centered care. Theory, evidence, and practice. J Gen Intern Med. 2006;21 Suppl 1:S9-S15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 101] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 14. | Faraj S, Xiao Y. Coordination in fast-response organizations. Manage Sci. 2006;52:1155-1169. [DOI] [Full Text] |
| 15. | Davidow WH, Malone MS. The virtual corporation: structuring and revitalizing the corporation for the 21st century. New York, NY: Harper Collins 1992; . |
| 16. | Porter ME, Millar VE. How information gives you competitive advantage. Harvard Bus Rev. 1985;63:149-160. [DOI] [Full Text] |
| 17. | Foy R, Hempel S, Rubenstein L, Suttorp M, Seelig M, Shanman R, Shekelle PG. Meta-analysis: effect of interactive communication between collaborating primary care physicians and specialists. Ann Intern Med. 2010;152:247-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 120] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 18. | Grant RM. Toward a knowledge-based theory of the firm. Strategic Manage J. 1996;17:109-122. [DOI] [Full Text] |
| 19. | Nonaka I, Takeuchi H. The knowledge-creating company. New York, NY: Oxford University Press 1995; . |
| 20. | Davenport TH, Thomas RJ, Cantrell S. The mysterious art and science of knowledge-worker performance. Mit Sloan Manage Rev. 2002;44:23-30. [DOI] [Full Text] |
| 21. | Hopp WJ, Iravani SMR, Liu F. Managing white-collar work: an operations-oriented survey. Prod Oper Manag. 2009;18:1-32 [DOI 10.1111/j.1937-5956.2009.01002.x]. |
| 22. | Becker BE, Huselid MA. Strategic human resources management: where do we go from here? J Manage. 2006;32:898-925. [DOI] [Full Text] |
| 23. | Teece DJ, Pisano G, Shuen A. Dynamic capabilities and strategic management. Strategic Manage J. 1997;18:509-533. [DOI] [Full Text] |
| 24. | Bontis N. Intellectual capital: an exploratory analysis that develops measures and models. Manage Decis. 1998;36:63-76. [DOI] [Full Text] |
| 25. | Grant RM. The resource-based theory of competitive advantage: implications for strategy formulation. Calif Manage Rev. 1991;33:114-135. [DOI] [Full Text] |
| 26. | Hatch NW, Dyer JH. Human capital and learning as a source of sustainable competitive advantage. Strategic Manage J. 2004;25:1155-1178. [DOI] [Full Text] |
| 27. | Wernerfelt B. A resource-based view of the firm. Strategic Manage J. 1984;5:171-180. [DOI] [Full Text] |
| 28. | Peiró S. Métodos de medición de casuística y ajuste de severidad y riesgos. Manuales de dirección médica y gestión clínica: gestión clínica desarrollo e instrumentos. Madrid: Ed. Díaz de Santos 2006; 145-200. |
| 29. | Deming WE. Out of the crisis. Cambridge, MA: MIT Press 1986; . |
| 30. | Vanhaverbeke W, Cloodt M. “Open innovation in value networks”. Open innovation: researching a new paradigm. Oxford: Oxford University Press 2006; 258-281. |
| 31. | Argote L. Input uncertainty and organizational coordination in hospital emergency units. Adm Sci Q. 1982;27:420-434. [PubMed] [DOI] [Full Text] |
| 32. | Kogut B, Zander U. What firms do? Coordination, identity and learning. Organ Sci. 1996;7:502-518. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1799] [Cited by in RCA: 1818] [Article Influence: 62.7] [Reference Citation Analysis (0)] |
| 33. | Thompson JD. Organizations in action: social science bases of administrative theory. New York, NY: McGraw-Hill 1967; . |
| 34. | Tushman M, Nadler D. Information processing as an integrating concept in organizational design. Acad Manage Rev. 1978;3:613-624. [DOI] [Full Text] |
| 35. | Van de Ven AH, Delbecq AL, Koenig R. Determinants of coordination modes within organizations. Am Sociol Rev. 1976;41:322-328. [DOI] [Full Text] |
| 36. | Heckscher C, Adler P. The firm as collaborative community: reconstructing trust in the knowledge economy. Oxford: Oxford University Press 2007; . |
| 37. | Heckscher C, Rubinstein SA, Flynn L, Erhardt N, Boniface M. Collaboration and the quality of health care delivery. Working Paper (Internet). Oxford: Oxford University Press 2009; (accessed 2013 May 23) Available from: http://www.lera.uiuc.edu/IndustryCouncils/healthcare/Heckscher-CollaborationQualityHealthcareDelivery.pdf. |
| 38. | Liang DW, Moreland R, Argote L. Group versus individual training and group performance: the mediating role of group transactive memory. Pers Soc Psychol Bull. 1995;21:384-393. [RCA] [DOI] [Full Text] [Cited by in Crossref: 620] [Cited by in RCA: 600] [Article Influence: 66.7] [Reference Citation Analysis (0)] |
| 39. | Quinn R, Dutton JE. Coordination as energy-in-conversation. Acad Manage Rev. 2005;30:36-57. [DOI] [Full Text] |
| 40. | Weick KE. The collapse of sense-making in organizations: the mann gulch disaster. Admin Sci Quart. 1993;38:628-652. [DOI] [Full Text] |
| 41. | Waller MJ. The timing of adaptative group responses to non-routine events. Acad Manage J. 1999;42:127-137. [DOI] [Full Text] |
| 42. | O’Reilly CA, Roberts K. Task group structure, communication and effectiveness in three organizations. J Appl Psychol. 1977;62:674-681. [RCA] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 115] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 43. | Saavedra R, Earley PC, Van Dyne L. Complex interdependence in task-performing groups. J Appl Psychol. 1993;78:61-72. [RCA] [DOI] [Full Text] [Cited by in Crossref: 443] [Cited by in RCA: 435] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 44. | Wageman R. Interdependence and group effectiveness. Admin Sci Quart. 1995;40:145-180. [DOI] [Full Text] |
| 45. | Dougherty D. Interpretive barriers to successful product innovation in large firms. Organ Sci. 1992;3:179-202. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1573] [Cited by in RCA: 1587] [Article Influence: 48.1] [Reference Citation Analysis (0)] |
| 46. | Dietz G, Hartog DND. Measuring trust inside organizations. Pers Rev. 2006;35:557-588. [DOI] [Full Text] |
| 47. | Dirks KT. The effects of interpersonal trust on work group performance. J Appl Psychol. 1999;84:445-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 395] [Cited by in RCA: 172] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 48. | Porter T, Lilly B. The effects of conflict, trust and task commitment on project team performance. Int J Confl Manage. 1996;7:361-376. [DOI] [Full Text] |
| 49. | Epstein RM, Hundert EM. Defining and assessing professional competence. JAMA. 2002;287:226-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1587] [Cited by in RCA: 1357] [Article Influence: 59.0] [Reference Citation Analysis (0)] |
| 50. | Epstein RM. Assessment in medical education. N Engl J Med. 2007;356:387-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 927] [Cited by in RCA: 889] [Article Influence: 49.4] [Reference Citation Analysis (0)] |
| 51. | Wass V, Van der Vleuten C, Shatzer J, Jones R. Assessment of clinical competence. Lancet. 2001;357:945-949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 620] [Cited by in RCA: 563] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 52. | Pisano GP. Knowledge, integration and the locus of learning: an empirical analysis of process development. Strategic Manage J. 1994;15:85-100. [DOI] [Full Text] |