Published online Feb 26, 2025. doi: 10.12998/wjcc.v13.i6.100673
Revised: September 27, 2024
Accepted: November 6, 2024
Published online: February 26, 2025
Processing time: 94 Days and 17.6 Hours
Abdominal aortic aneurysm (AAA) repair often involves significant postoperative pain, traditionally managed with systemic opioids, which can cause undesirable side effects. This case report explores the novel use of a surgically-initiated rectus sheath block with a catheter-over-needle assembly for pain management in AAA repair.
A 67-year-old female with hypertension and previous aortic dissection underwent elective open repair of an infrarenal AAA, which had grown from 3.4 cm to 4.3 cm over 14 months. A rectus sheath block was initiated surgically for postoperative pain control. The patient reported low pain scores and did not require systemic intravenous opioids, enabling early ambulation and discharge on postoperative day seven without complications. By preventing complications of systemic opi
Surgically-initiated rectus sheath block as a valuable tool for managing postoperative pain in AAA repair.
Core Tip: This case report highlights the successful use of a surgically-initiated rectus sheath block for postoperative pain management in a patient undergoing elective abdominal aortic aneurysm repair. The technique provided effective analgesia without the need for systemic opioids, enabling early ambulation and discharge on postoperative day seven. The rectus sheath block offers a promising alternative for pain control in abdominal surgeries, minimizing opioid-related side effects. Further research is needed to validate its safety and efficacy in larger patient cohorts.
- Citation: Chen KH, Kang MY, Chang YT, Huang SY, Wu YS. Enhancing postoperative pain control by surgically-initiated rectus sheath block in abdominal aortic aneurysm open repair: A case report. World J Clin Cases 2025; 13(6): 100673
- URL: https://www.wjgnet.com/2307-8960/full/v13/i6/100673.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i6.100673
Abdominal aortic aneurysm (AAA) open repair is known to cause significant postoperative pain, which can lead to delayed recovery and increased morbidity. Postoperative pain restricts the depth of breathing, resulting in a higher incidence of postoperative pulmonary complications. These complications contribute to elevated morbidity and mortality rates, underscoring the critical importance of effective pain management following AAA repair surgery[1].
Instead of relying on systemic opioid analgesics, regional anesthetic techniques such as epidural or spinal anesthesia and peripheral nerve blocks can be utilized to avoid adverse effects like nausea, vomiting, hypotension, respiratory depression, and delayed recovery associated with systemic opioid use. However, the use of spinal opioids is contraindicated in aortic aneurysm surgery due to the common peri- and postoperative use of Heparin, which poses a risk[2].
An alternative option for pain management is rectus sheath catheter analgesia, which does not have the limitation of heparin use. This technique has shown promising results, with significantly lower resting pain scores at 72 hours post
This case report highlights the successful utilization of surgically-initiated rectus sheath block for postoperative pain control in a 67-year-old female patient undergoing AAA repair surgery. Based on our findings, we recommend using this method for pain management in AAA repair surgery, as it offers excellent patient satisfaction and favorable outcomes.
Painless abdominal aorta mass with progressing size by images.
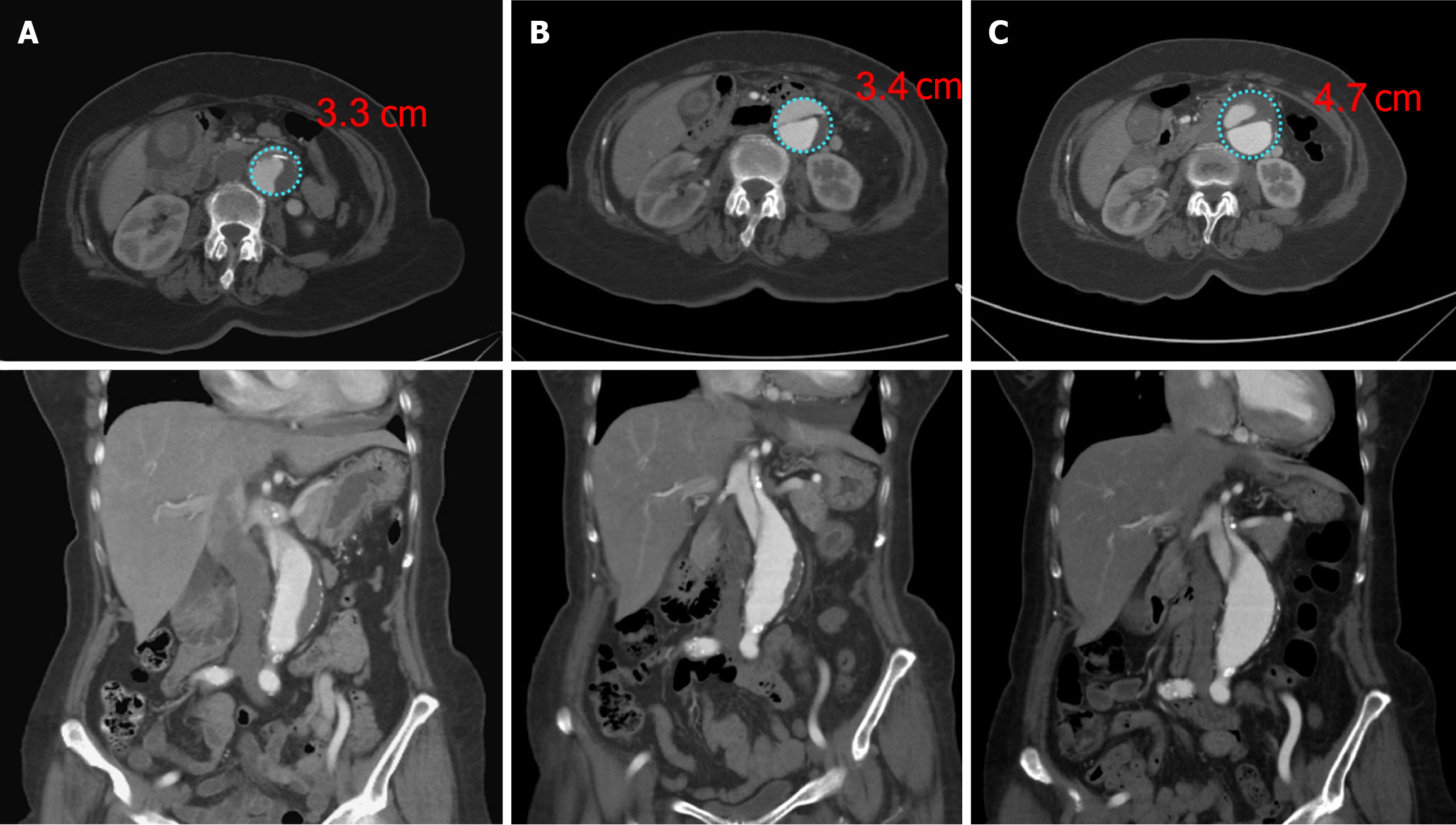
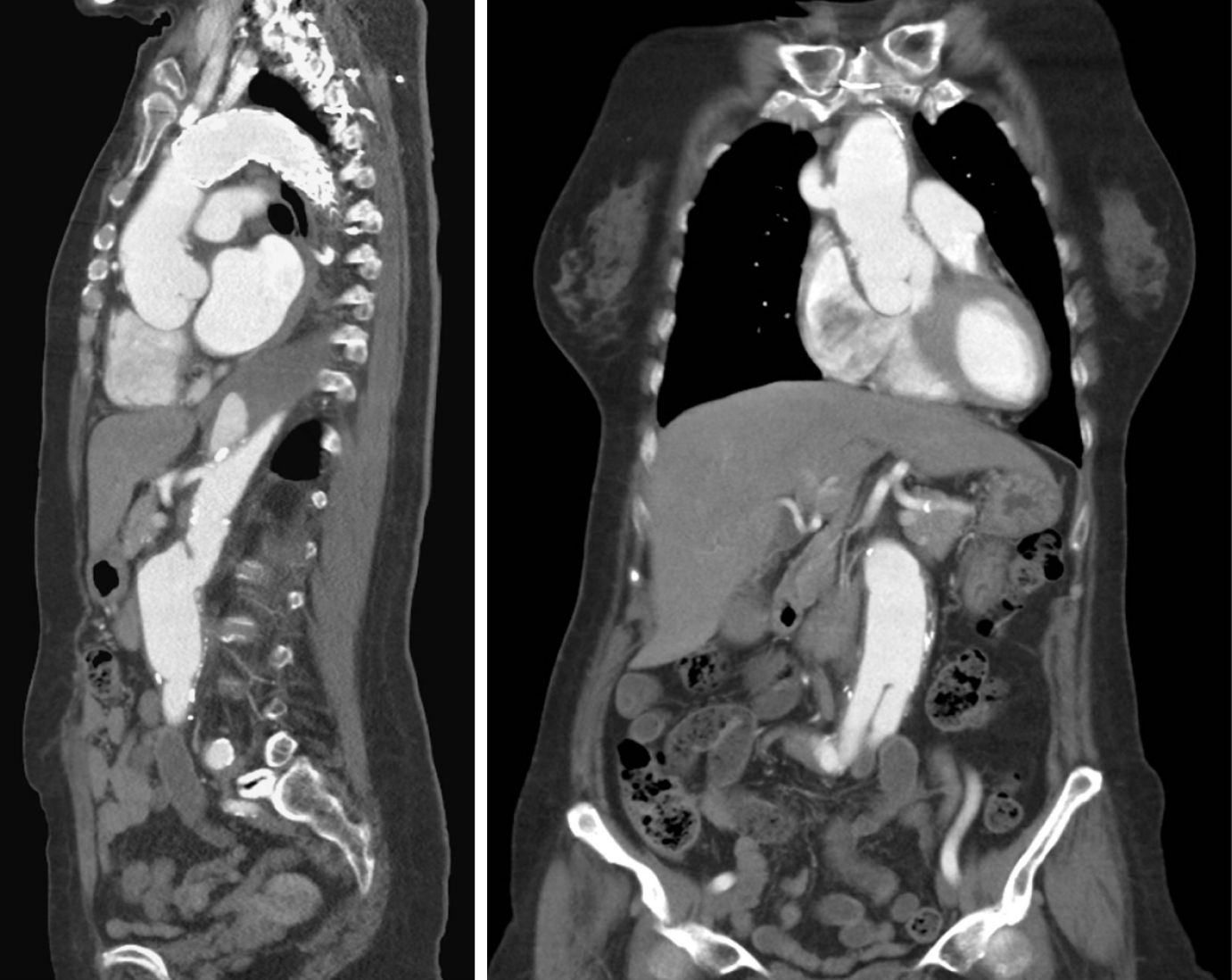
We report the case of a 67-year-old female patient who underwent elective open repair of an infrarenal AAA that had increased in size from 3.4 cm to 4.3 cm over 14 months, as shown in Figure 1A.
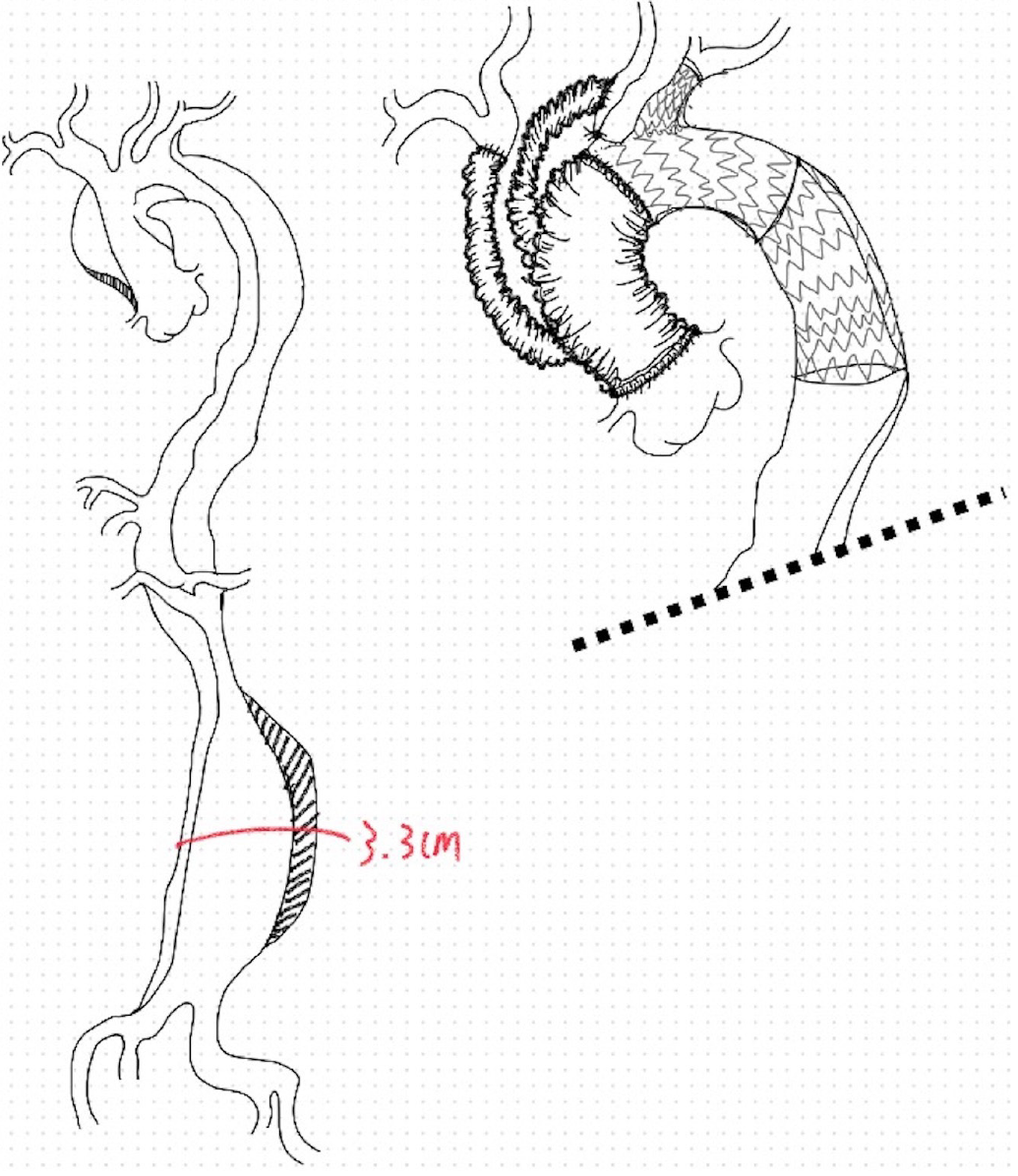
The patient had a history of hypertension and an acute type A aortic dissection with hemopericardium, for which she underwent emergent surgery 16 months earlier, illustrated as Figure 2. The previous procedures included ascending aorta and total arch replacement with a 28 mm 4-branch Gelsoft™ graft and a frozen elephant trunk technique (Thoracic endovascular aortic repair, thoracic endovascular aortic repair, zone 1 landing: GORE C-TAG TGU313110 + TGU2626
On examination, she was stable with normal vital signs. On palpation, she had no abdominal mass. She had no signs of deep venous thrombosis in her legs. She also had no signs of heart failure or lower limb vascular obstruction.
Progression of infra-renal AAA was noted by sequential computed tomography (CT) imaging. The lesion size grew over 1 cm within approximately a year.
Two months after the initial surgery, a CT angiography (CTA) showed an infrarenal AAA measuring 3.4 cm, as shown in Figure 1B. This aneurysm further expanded to 4.3 cm by 16 months post-surgery, as Figure 1C.
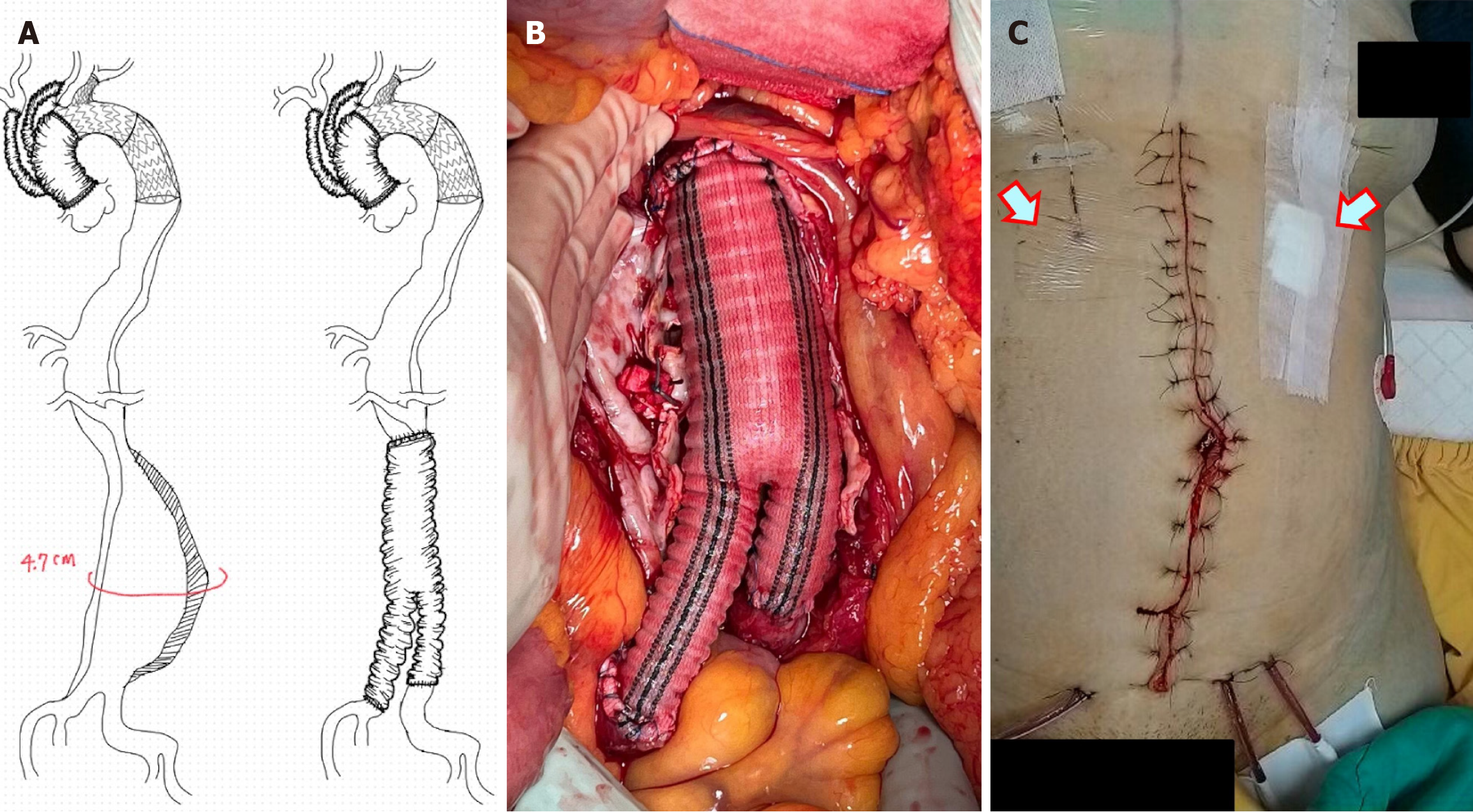
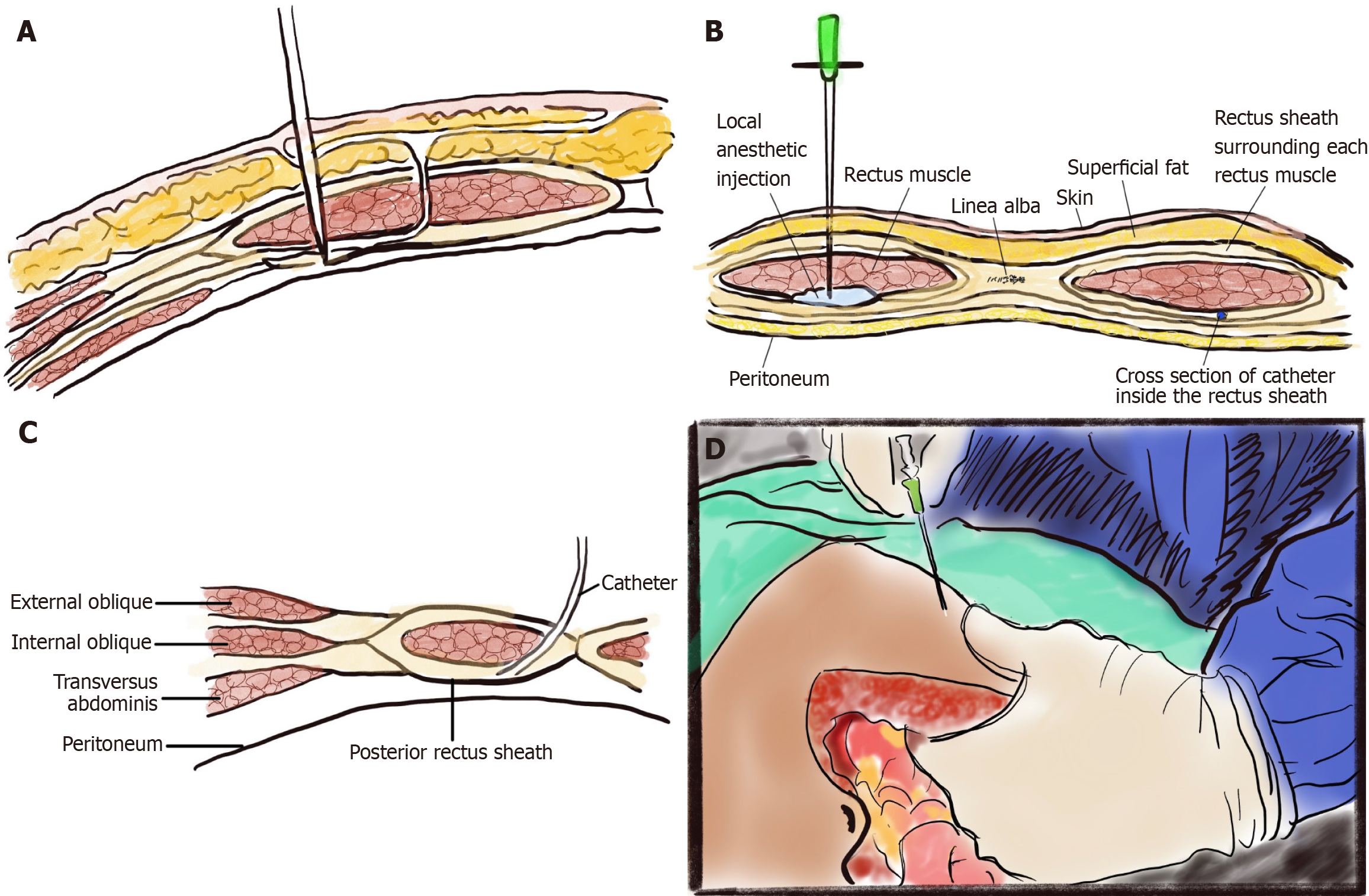
We performed an open surgical reconstruction of the infrarenal abdominal aorta to the bilateral common iliac arteries using a Gelsoft™ Vascular Prosthesis (Y graft, 22-11 mm), as Figure 3A and B; the inferior mesenteric artery was also ligated. The catheter was secured with a subcutaneous tunnel and suture, and connected to a patient-controlled analgesia pump delivering a continuous infusion of ropivacaine for three days postoperatively, as Figure 3C. Intraoperatively, we placed a rectus sheath catheter through the rectus muscle using a catheter-over-needle assembly for postoperative pain control, illustrated in Figure 4.
The patient’s postoperative pain was well-controlled, necessitating only oral analgesics. She was able to ambulate and participate in physical therapy shortly after being transferred to the general ward. The catheter was removed on the third postoperative day, and the patient was discharged on the seventh postoperative day.
Nine months after surgery, a follow-up CTA scan indicated a stable condition of the dissecting flap from the de
Despite advancements in pain management, postoperative pain remains a significant challenge in this patient demo
Furthermore, the rectus sheath block is recognized as a safe and effective technique for managing postoperative pain across a spectrum of surgical procedures, including abdominal surgeries like genitourinary and aortic surgeries, which are often associated with substantial pain and discomfort. Postsurgical pain was reported by 97.1% of patients under
Compared to systemic opioids, the advantages of the rectus sheath block include effective and targeted pain relief without the need for external catheterization, which can lead to side effects such as nausea, vomiting, sedation, and respiratory depression[11]. This approach ultimately enhances patient comfort, accelerates recovery, and reduces hospitalization durations[12].
Moreover, in aortic surgery, the administration of heparin is indispensable for preventing thrombotic complications. However, this necessitates careful consideration of pain management strategies, as heparin is a well-known contraindication for spinal anesthesia[2]. Unlike spinal anesthesia, which has clear contraindications in the presence of heparin due to associated coagulation risks, rectus sheath block emerges as a promising alternative for postoperative pain control in aortic surgery patients. Its few absolute contraindications include patient refusal and allergy to local anesthesia[4].
Rectus sheath block has been employed in various abdominal surgeries and pediatric cardiac surgeries. Typically, anesthetists have applied this technique under the guidance of ultrasonography. In contrast, surgeons find it straightforward to perform this procedure independently, relying on anatomical landmarks, such as laparoscopic guidance, as Figure 4. Consequently, we foresee the potential for the widespread utilization of this technique in open aortic surgery, which could provide more clinical data in the near future.
Surgically-initiated rectus sheath block, employing a catheter-over-needle assembly, represents a promising approach for managing postoperative pain following AAA repair. This method provides efficient and precise pain relief without relying on systemic opioids or external catheterization, ultimately leading to enhanced patient outcomes. In the case described, the patient reported notably low postoperative pain scores, and there was no documented need for systemic intravenous opioids, resulting in satisfactory pain control. However, it is important to emphasize that this technique has not yet been standardized in our patient care protocols. More comprehensive studies are required to validate its safety and efficacy across a broader patient population.
| 1. | Pasin L, Nardelli P, Belletti A, Greco M, Landoni G, Cabrini L, Chiesa R, Zangrillo A. Pulmonary Complications After Open Abdominal Aortic Surgery: A Systematic Review and Meta-Analysis. J Cardiothorac Vasc Anesth. 2017;31:562-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 2. | Champagne K, Fecek C, Goldstein S. Spinal Opioids in Anesthetic Practice. 2023 Apr 2. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 3. | Krige A, Brearley SG, Mateus C, Carlson GL, Lane S. A comparison between thoracic epidural analgesia and rectus sheath catheter analgesia after open midline major abdominal surgery: randomized clinical trial. BJS Open. 2022;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 4. | Rucklidge M, Beattie E. Rectus sheath catheter analgesia for patients undergoing laparotomy. BJA Educ. 2018;18:166-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | De Paulis S, Arlotta G, Calabrese M, Corsi F, Taccheri T, Antoniucci ME, Martinelli L, Bevilacqua F, Tinelli G, Cavaliere F. Postoperative Intensive Care Management of Aortic Repair. J Pers Med. 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Maury T, Elnar A, Marchionni S, Frisoni R, Goetz C, Bécret A. Effect of rectus sheath anaesthesia versus thoracic epidural analgesia on postoperative recovery quality after elective open abdominal surgery in a French regional hospital: the study protocol of a randomised controlled QoR-RECT-CATH trial. BMJ Open. 2023;13:e069736. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Wilkinson KM, Krige A, Brearley SG, Lane S, Scott M, Gordon AC, Carlson GL. Thoracic Epidural analgesia versus Rectus Sheath Catheters for open midline incisions in major abdominal surgery within an enhanced recovery programme (TERSC): study protocol for a randomised controlled trial. Trials. 2014;15:400. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Yassin HM, Abd Elmoneim AT, El Moutaz H. The Analgesic Efficiency of Ultrasound-Guided Rectus Sheath Analgesia Compared with Low Thoracic Epidural Analgesia After Elective Abdominal Surgery with a Midline Incision: A Prospective Randomized Controlled Trial. Anesth Pain Med. 2017;7:e14244. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 9. | Claxton HL, Nevins EJ, McCallum I. Comparison of the effectiveness of thoracic epidural and rectus sheath catheter as analgesic modalities following laparotomy: A systematic review and meta-analysis. J Perioper Pract. 2023;33:332-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Fatma A, Serife K. Experience of Pain in Patients Undergoing Abdominal Surgery and Nursing Approaches to Pain Control. Int J Caring Sci. 2017;10:1456-1464. |