Published online Oct 6, 2025. doi: 10.12998/wjcc.v13.i28.108437
Revised: May 27, 2025
Accepted: July 9, 2025
Published online: October 6, 2025
Processing time: 115 Days and 7.6 Hours
Mirizzi syndrome is a rare complication of chronic gallstone disease in which an impacted stone causes compression or erosion of the common hepatic duct. Accurate preoperative diagnosis is crucial but often challenging. We report a case that was preoperatively diagnosed as type 1 Mirizzi syndrome but was found intraoperatively to be type 4, involving a cholecysto-biliary fistula and complete erosion of the common hepatic duct.
A 74-year-old woman presented with right upper quadrant discomfort. Initial workup including ultrasound and magnetic resonance cholangiopancreatography suggested Mirizzi syndrome type 1 due to extrinsic compression of the common hepatic duct. Endoscopic retrograde cholangiopancreatography confirmed a large stone without evidence of fistula. The patient underwent robotic-assisted chole
Preoperative imaging may fail to identify fistula formation in Mirizzi syndrome. Intraoperative assessment remains critical for accurate diagnosis and safe surgical management.
Core Tip: This case highlights the diagnostic challenge of Mirizzi syndrome, where advanced imaging modalities including endoscopic retrograde cholangiopancreatography and cholangioscopy suggested type 1 disease, but intraoperative findings revealed a type 4 cholecysto-biliary fistula. Robotic-assisted surgery with intraoperative cholangioscopy allowed precise diagnosis and primary biliary repair. The case underscores the importance of surgical vigilance and the role of minimally invasive techniques in managing complex biliary pathology.
- Citation: Gupta AK, Surendranath A. Cholecysto-biliary fistula mimicking type 1 Mirizzi syndrome: A case report. World J Clin Cases 2025; 13(28): 108437
- URL: https://www.wjgnet.com/2307-8960/full/v13/i28/108437.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i28.108437
Symptomatic cholelithiasis is one of the most common conditions encountered in general surgery[1]. Laparoscopic cholecystectomy is considered the gold standard treatment for biliary colic and uncomplicated gallstone disease[2]. However, gallstones can manifest in a broad clinical spectrum, ranging from asymptomatic presentations to severe complications such as acute cholecystitis, choledochoenteric fistulas, and obstructive jaundice[3,4]. Effective management must therefore be individualized, taking into account the location of the stone, the clinical scenario, and the patient's comorbid profile[5].
Mirizzi syndrome is a rare complication of gallstone disease, characterized by external compression or erosion of the common hepatic duct due to an impacted gallstone in the cystic duct or gallbladder neck[6]. In advanced stages, it may result in cholecystoenteric fistulas or gallstone ileus[4,7]. Although cholecystectomy remains the definitive treatment, the surgical approach often deviates from standard protocols due to distorted anatomy, inflammation, or fistulous communications. These anatomical alterations can preclude achievement of the critical view of safety in Calot’s triangle, which is a fundamental principle of safe laparoscopic cholecystectomy[8,9].
A 74-year-old woman presented with intermittent right upper quadrant abdominal discomfort for approximately 2 weeks.
The patient reported intermittent episodes of dull, aching pain in the right upper quadrant without radiation. The symptoms were not associated with nausea, vomiting, fever, jaundice, or changes in bowel habits. The episodes increased in frequency and intensity, prompting evaluation by her primary care provider.
The patient had a history of well-controlled hypertension and hyperlipidemia. She had no prior history of gallbladder disease, biliary intervention, or abdominal surgeries.
There was no personal or family history of gastrointestinal malignancies, gallbladder disease, or liver pathology. She denied alcohol or tobacco use.
On physical examination, the patient was afebrile and hemodynamically stable. Abdominal examination showed no tenderness, guarding, or rebound. There were no palpable masses or hepatosplenomegaly. Murphy’s sign was negative.
Complete blood count, comprehensive metabolic panel, and liver function tests (including aspartate transaminase, alanine transaminase, alkaline phosphatase, and bilirubin) were within normal limits. Inflammatory markers such as C-reactive protein and white blood cell count were unremarkable.
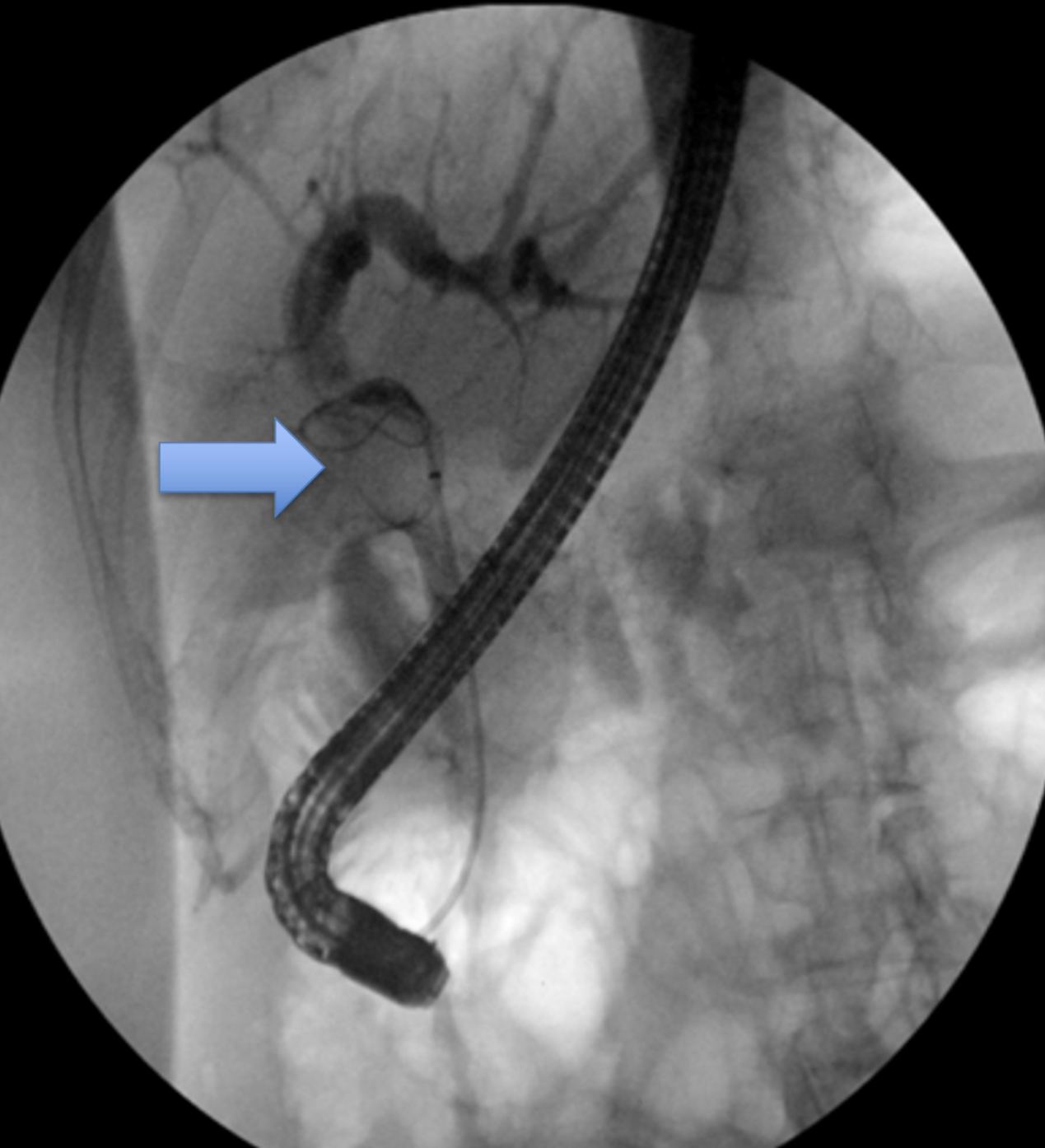
Abdominal ultrasonography revealed multiple gallstones and a dilated common bile duct measuring 8.3 mm (Figure 1). No pericholecystic fluid or gallbladder wall thickening was noted. Magnetic resonance cholangiopancreatography (MRCP) demonstrated intrahepatic biliary ductal dilation and compression of the common hepatic duct, consistent with type 1 Mirizzi syndrome. Endoscopic ultrasound and endoscopic retrograde cholangiopancreatography (ERCP) confirmed extrinsic compression of the common hepatic duct by an impacted stone (Figure 2). Cholangioscopy showed no evidence of intraductal lesions or fistula at that time.
The patient’s case was reviewed in a multidisciplinary team setting involving general surgery, gastroenterology, and radiology. Imaging studies, including MRCP and ERCP findings, were discussed. The consensus was that the patient most likely had type 1 Mirizzi syndrome based on extrinsic compression without clear evidence of fistula formation. Gastroenterology confirmed no intraductal lesion on cholangioscopy. The surgical team recommended robotic-assisted cholecystectomy with intraoperative cholangioscopy to further evaluate and treat the biliary pathology.
Type 4 Mirizzi syndrome characterized by a cholecysto-biliary fistula with complete erosion of the common hepatic duct wall, initially misdiagnosed as type 1 Mirizzi syndrome based on preoperative imaging.
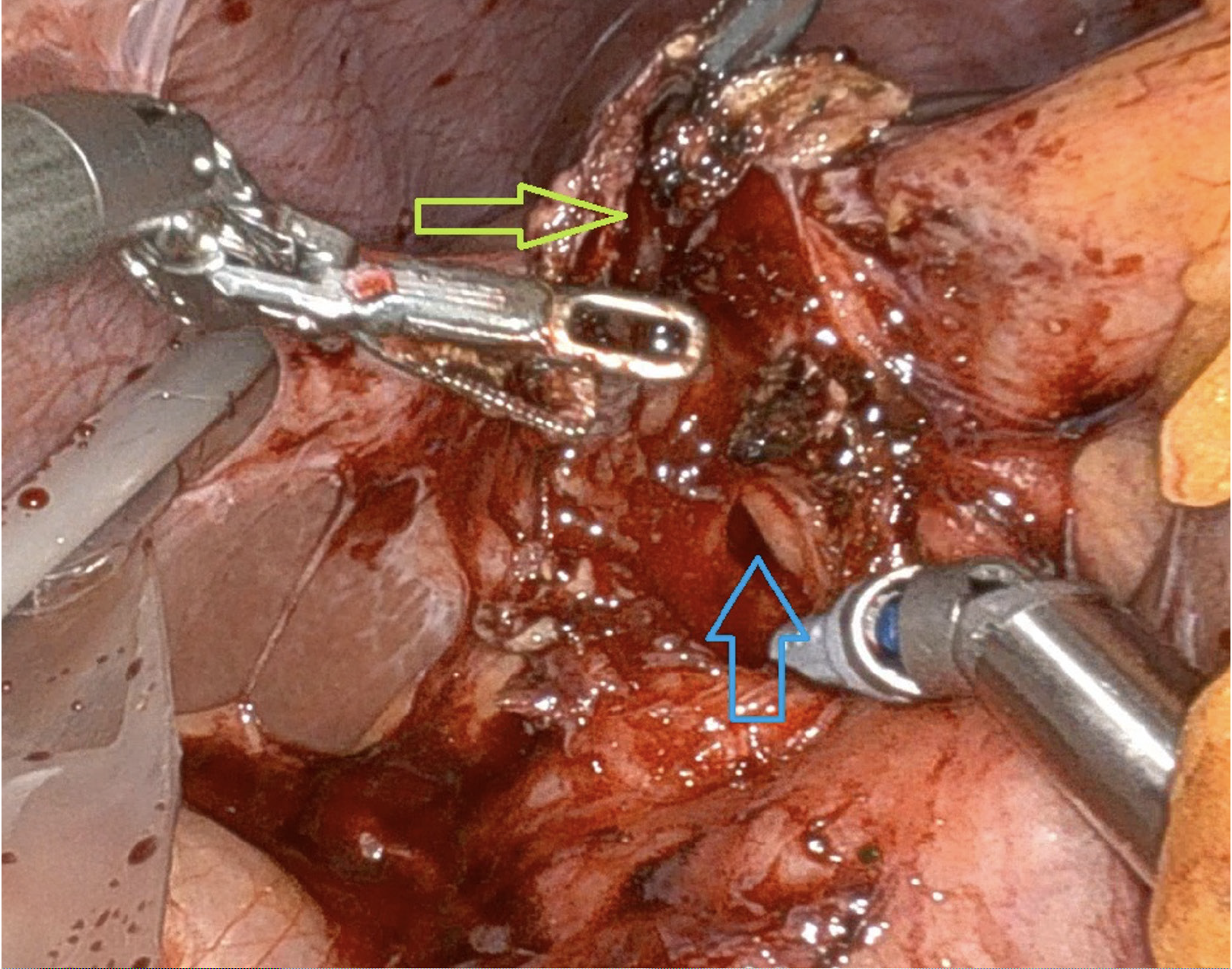
The patient underwent robotic-assisted cholecystectomy using a four-port technique. Intraoperatively, the gallbladder was noted to be contracted and densely adherent to the common hepatic duct. Upon opening the gallbladder, a large 4 cm stone was identified eroding into the wall of the common hepatic duct, consistent with type 4 Mirizzi syndrome.
The erosion of the common hepatic duct was confirmed using indocyanine green (ICG) dye, which was observed pouring directly from the duct, indicating a full-thickness fistula. Intraoperative cholangioscopy was then performed through the cystic duct remnant and confirmed the presence of a cholecysto-biliary fistula. It also verified the patency of the proximal intrahepatic ducts and distal common bile duct, with no evidence of intraductal stones, malignancy, or residual pathology.
A primary repair of the common hepatic duct was performed using a running absorbable suture. The duct was noted to be dilated, which facilitated tension-free closure without the need for ductoplasty or a biliary-enteric anastomosis. A closed suction drain was placed in the subhepatic space, and the procedure was completed robotically without complications or need for conversion to an open approach.
The patient tolerated the robotic-assisted procedure well and was discharged on the same day of surgery with a closed suction drain in place. No immediate postoperative complications were noted.
At the two-week outpatient follow-up, the patient reported resolution of symptoms. The surgical drain was removed at that time after confirming the absence of bile leakage and ensuring proper wound healing.
At the three-month follow-up visit, the patient remained asymptomatic. She reported normal appetite, bowel function, and no abdominal discomfort. Liver function tests were within normal limits, and there was no clinical or biochemical evidence of biliary stricture or recurrent disease.
Cholelithiasis is a ubiquitous presentation. The precipitation of salt in bile leads to the formation of crystals, which progressively grow to form stones[10]. The Presentation, location of gallstones, and associated inflammatory findings can drastically change the management[11,12]. It is crucial to determine the presentation for preoperative planning and assessment and to select the appropriate procedure[13].
Mirizzi syndrome is an unusual presentation described by Argentinian surgeon Pablo Louis Mirizzi[14]. The presence of gallstones in Hartmann's pouch or cystic duct can cause compression of the common hepatic duct, and progressive compression can lead to fistulization[15]. One large stone or multiple small compacted stones can cause this mass effect. Mirizzi syndrome is a rare condition that occurs in 0.1% of patients with gallstones, typically presenting between the ages of 40 and 70[16]. Based on the compression and fistulization, Mirizzi syndrome is categorized by Csendes classification as: Type 1- compression of the common hepatic duct with no fistulization; type 2 - fistulization into the common hepatic duct less than 33%; type 3- fistulization into the common hepatic duct from 33%-66%; type 4- fistulization into the common bile duct more than 66%[17].
Presentation and categorization are essential for identifying and surgically planning patients. Patients can present with Mirizzi syndrome as asymptomatic when it is just compressing the bile duct, jaundice, or cholangitis if the compression of fistulization is significant[17,18]. Mirizzi syndrome can be diagnosed with ultrasound or magnetic resonance cholangiopancreatography; however, endoscopic retrograde cholangiopancreatography is regarded as the most effective method for preoperative diagnosis[19].
Mirizzi syndrome may not be picked up initially and may be found intraoperatively with a difficult Calot's triangle dissection or postoperatively with a biliary tract leak. Alternatively, it may present with jaundice and cholangitis when there is extensive fistulization into the biliary tree. The condition can also mimic cholangiocarcinoma. Many authors consider Mirizzi syndrome, which causes prolonged inflammation, to be a predisposing factor for cholangiocarcinoma[18-20].
During the workup of Mirizzi syndrome, it was essential to rule out cholangiocarcinoma and understand the biliary tract anatomy appropriately[20-23].
Failure to identify biliary Mirizzi syndrome increases chances and is also an independent factor for common bile duct injury in patients during cholecystectomy. dissection in and around the Calot's triangle with the energy source can lead to biliary stricture formation in the future. It was essential to realize the anatomy early and change the surgical approach to move away from the Calot's triangle to avoid complications involving the common bile duct and the biliary tree[24]. The surgical approach should be away from the Calot’s triangle to open the gallbladder like that of subtotal cholecystectomy[25]. During a cholecystectomy, the gallbladder should be opened distal to the cystic duct with removal and evacuation of all stones and closure of the stump of the gallbladder. Intraoperative cholangiogram and indocyanine green administration prior to surgery can help evaluate and delineate the anatomy better and identify the site of subtotal chole
In our patient largely asymptomatic presentation, liver function tests being normal, magnetic resonance imaging and subsequently an endoscopic retrograde cholangiogram pancreaticography with cholangioscopy failed to reveal an obvious fistula. Intraoperative on opening the gallbladder we identified complete cholecysto-biliary fistula needing common bile duct exploration and reconstruction of common bile duct.
Mirizzi syndrome remains a complex diagnostic and surgical challenge, particularly when preoperative imaging fails to reveal the true extent of biliary involvement. This case of type 4 Mirizzi syndrome, initially misdiagnosed as type 1, underscores the limitations of non-invasive imaging and the importance of intraoperative assessment. The use of indocyanine green dye and intraoperative cholangioscopy facilitated accurate identification of a cholecysto-biliary fistula. Robotic-assisted primary ductal repair in a dilated duct enabled successful management without the need for biliary-enteric diversion. Early recognition, surgical adaptability, and use of advanced intraoperative tools are critical in ensuring optimal outcomes in such complex biliary cases.
| 1. | Gupta AK, Farshchian JN, Hus N. A Retrospective Study Comparing Radiological to Histopathological Diagnosis After Laparoscopic Cholecystectomy for Suspected Cholecystitis. Cureus. 2020;12:e10817. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 2. | Shenoy R, Kirkland P, Hadaya JE, Tranfield MW, DeVirgilio M, Russell MM, Maggard-Gibbons M. Management of symptomatic cholelithiasis: a systematic review. Syst Rev. 2022;11:267. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 3. | Ahmed A, Cheung RC, Keeffe EB. Management of gallstones and their complications. Am Fam Physician. 2000;61:1673-1680, 1687. [PubMed] |
| 4. | Gupta AK, Vazquez OA, Yeguez JF, Brenner B. Laparoscopic Approach for Gallstone Ileus in Geriatric Patients. Cureus. 2020;12:e8642. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Mencarini L, Vestito A, Zagari RM, Montagnani M. The Diagnosis and Treatment of Acute Cholecystitis: A Comprehensive Narrative Review for a Practical Approach. J Clin Med. 2024;13:2695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 6. | Toursarkissian B, Holley DT, Kearney PA, McGrath PC, Zweng TN. Mirizzi's syndrome. South Med J. 1994;87:471-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Valderrama-Treviño AI, Granados-Romero JJ, Espejel-Deloiza M, Chernitzky-Camaño J, Barrera Mera B, Estrada-Mata AG, Ceballos-Villalva JC, Acuña Campos J, Argüero-Sánchez R. Updates in Mirizzi syndrome. Hepatobiliary Surg Nutr. 2017;6:170-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 39] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 8. | Lacerda Pde S, Ruiz MR, Melo A, Guimarães LS, Silva-Junior RA, Nakajima GS. Mirizzi syndrome: a surgical challenge. Arq Bras Cir Dig. 2014;27:226-227. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Lai W, Yang J, Xu N, Chen JH, Yang C, Yao HH. Surgical strategies for Mirizzi syndrome: A ten-year single center experience. World J Gastrointest Surg. 2022;14:107-119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 2] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Reshetnyak VI. Concept of the pathogenesis and treatment of cholelithiasis. World J Hepatol. 2012;4:18-34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 103] [Cited by in RCA: 96] [Article Influence: 7.4] [Reference Citation Analysis (5)] |
| 11. | Shaffer EA. Gallstone disease: Epidemiology of gallbladder stone disease. Best Pract Res Clin Gastroenterol. 2006;20:981-996. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 444] [Cited by in RCA: 488] [Article Influence: 25.7] [Reference Citation Analysis (6)] |
| 12. | Abraham S, Rivero HG, Erlikh IV, Griffith LF, Kondamudi VK. Surgical and nonsurgical management of gallstones. Am Fam Physician. 2014;89:795-802. [PubMed] |
| 13. | Lavin A, Gupta A, Lopez-Viego M, Buicko JL. Incarcerated Spigelian Hernias: A Rare Cause of a High-grade Small Bowel Obstruction. Cureus. 2020;12:e7397. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Leopardi LN, Maddern GJ. Pablo Luis Mirizzi: the man behind the syndrome. ANZ J Surg. 2007;77:1062-1064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Wu J, Cai SY, Chen XL, Chen ZT, Shi SH. Mirizzi syndrome: Problems and strategies. Hepatobiliary Pancreat Dis Int. 2024 Jun;23(3):234-240. doi: 10.1016/j.hbpd.2024.01.005. Epub 2024 Jan 30. PMID: 38326157. |
| 16. | Koo JGA, Tham HY, Toh EQ, Chia C, Thien A, Shelat VG. Mirizzi Syndrome-The Past, Present, and Future. Medicina (Kaunas). 2023;60:12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 17. | Klekowski J, Piekarska A, Góral M, Kozula M, Chabowski M. The Current Approach to the Diagnosis and Classification of Mirizzi Syndrome. Diagnostics (Basel). 2021;11:1660. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 18. | Pemberton M, Wells AD. The Mirizzi syndrome. Postgrad Med J. 1997;73:487-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | Pariani D, Zetti G, Galli F, Cortese F. Mirizzi syndrome: from ultrasound diagnosis to surgery-a case report. Case Rep Surg. 2013;2013:268760. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 20. | Shirah BH, Shirah HA, Albeladi KB. Mirizzi syndrome: necessity for safe approach in dealing with diagnostic and treatment challenges. Ann Hepatobiliary Pancreat Surg. 2017;21:122-130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 21. | Beltrán MA. Mirizzi syndrome: history, current knowledge and proposal of a simplified classification. World J Gastroenterol. 2012;18:4639-4650. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 104] [Cited by in RCA: 116] [Article Influence: 8.9] [Reference Citation Analysis (2)] |
| 22. | Gupta AK, Parker BM. Bleeding After a Single Dose of Ketorolac in a Postoperative Patient. Cureus. 2020;12:e8919. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 23. | Clemente G, Tringali A, De Rose AM, Panettieri E, Murazio M, Nuzzo G, Giuliante F. Mirizzi Syndrome: Diagnosis and Management of a Challenging Biliary Disease. Can J Gastroenterol Hepatol. 2018;2018:6962090. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 24. | Chen H, Siwo EA, Khu M, Tian Y. Current trends in the management of Mirizzi Syndrome: A review of literature. Medicine (Baltimore). 2018;97:e9691. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 72] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 25. | Koike D, Suka Y, Nagai M, Nomura Y, Tanaka N. Laparoscopic Management of Mirizzi Syndrome Without Dissection of Calot's Triangle. J Laparoendosc Adv Surg Tech A. 2017;27:141-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 26. | Boni L, David G, Mangano A, Dionigi G, Rausei S, Spampatti S, Cassinotti E, Fingerhut A. Clinical applications of indocyanine green (ICG) enhanced fluorescence in laparoscopic surgery. Surg Endosc. 2015;29:2046-2055. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 279] [Cited by in RCA: 361] [Article Influence: 32.8] [Reference Citation Analysis (0)] |
| 27. | Cawich SO, Wilson C, Simpson LK, Baker AJ. Stump cholecystitis: laparoscopic completion cholecystectomy with basic laparoscopic equipment in a resource poor setting. Case Rep Med. 2014;2014:787631. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |