Published online Sep 26, 2025. doi: 10.12998/wjcc.v13.i27.108693
Revised: May 22, 2025
Accepted: June 20, 2025
Published online: September 26, 2025
Processing time: 106 Days and 20.1 Hours
Foreign body ingestion is a common emergency in clinical practice. While the majority of cases are resolved following successful removal, rare and unexpected complications can arise, such as the spontaneous displacement of a foreign body during the procedure. This report describes a unique case where a foreign body initially lodged in the esophagus was dropped during the procedure, leading to aspiration and migration to the airway.
A 69-year-old Chinese woman presented with a 6-hour history of throat pain and tightness after consuming rabbit meat. She had no fever or bloody stools but had a history of hypertension. Initial imaging, including a neck computed tomography scan, indicated a foreign body in the upper esophagus. Esophageal endoscopy was performed, during which the patient’s vital signs remained stable. The pro
Endoscopic removal of an esophageal foreign body can cause silent aspiration in elderly patients with absent cough reflexes, necessitating bedside imaging and prompt intervention.
Core Tip: This case report highlights the rare occurrence of aspiration during endoscopic foreign body removal, despite the absence of typical coughing reflexes. We emphasize the importance of bedside imaging for early detection of accidentally ingested foreign body and the role of emergency fiberoptic bronchoscopy in successful retrieval. These findings underscore the need for increased awareness and improved procedural strategies to prevent aspiration-related complications in high-risk patients.
- Citation: Qiao HW, Ye YF, Nie LX, Bai S, Du GZ. Disappearing intraesophageal foreign body: A case report. World J Clin Cases 2025; 13(27): 108693
- URL: https://www.wjgnet.com/2307-8960/full/v13/i27/108693.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i27.108693
Foreign body ingestion is a frequent clinical emergency that often necessitates endoscopic intervention[1]. While the majority of cases are resolved following successful removal, rare and unexpected complications can arise, such as the spontaneous displacement of a foreign body during the procedure[2]. This report details a unique case in which a foreign body initially lodged in the esophagus was displaced during endoscopic removal, leading to aspiration and eventual migration into the airway. The foreign body was successfully retrieved using emergency fiberoptic bronchoscopy. In
| Time | Event | Key findings |
| Pre-admission | Rabbit meat ingestion | Initiated FB event |
| Admission | Clinical evaluation | BP 206/74 mmHg; Pharyngeal FB sensation |
| 02:00 am | Cervical CT | 2.6 cm linear FB at C7-T2 with mural edema |
| 11:00 am | EGD under sedation | Mucosal erosion (14 cm); FB dislodged to hypopharynx |
| Intra-procedure | Vital signs | SpO2 94%; ↓breath sounds (LLL) |
| Post-EGD | Chest X-ray | Left lower lobe atelectasis |
| Emergency phase | Bronchoscopy | FB retrieved from airway (8-minute GA) |
| 24-hour post-op | Ward care | Rehydration, BP control, antibiotics |
| Discharge | Follow-up | Stable condition; hypertension regimen adjusted |
A 69-year-old woman was admitted with the persistent sensation of a foreign body in her throat, along with throat pain and tightness over the past 6 hours.
The patient developed a persistent foreign body sensation in her throat, along with throat pain and tightness, six hours after consuming rabbit meat. She denied any additional symptoms such as nausea, vomiting, hematemesis, hemoptysis, or melena.
The patient had a history of hypertension, with fluctuating blood pressure measurements ranging from 180-210/70-90 mmHg, and had not been on regular treatment. She denied any history of diabetes mellitus, tuberculosis, typhoid fever, malaria, heart disease, cerebrovascular disease, or mental illness. There was no history of trauma or surgery, and she also denied any food or drug allergies.
No special personal or family history was noted except a history of cesarean section under general anesthesia.
The patient’s vital signs were stable, with elevated blood pressure of 206/74 mmHg and oxygen saturation measured by pulse oximetry (SpO2) of 97%. Upon auscultation, symmetrical, coarse breath sounds were heard bilaterally.
All blood test results were within normal limits.
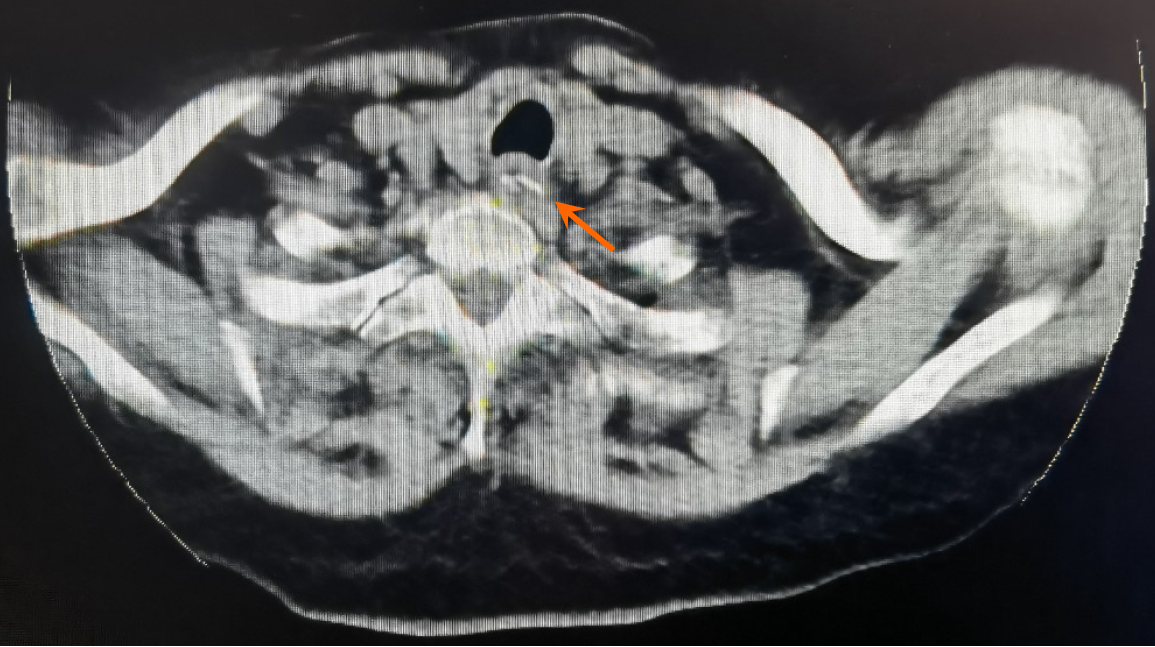
Computed tomography (CT) of the neck showed a 2.6 cm × 0.7 cm strip-shaped hyperdensity in the upper esophagus (C7-T2), along with swelling of the surrounding esophageal wall, suggestive of a foreign body (Figure 1). Chest CT revealed scattered chronic inflammation in both lungs, with partial interstitial changes.
Esophageal foreign body and hypertension grade 3 (very high risk).
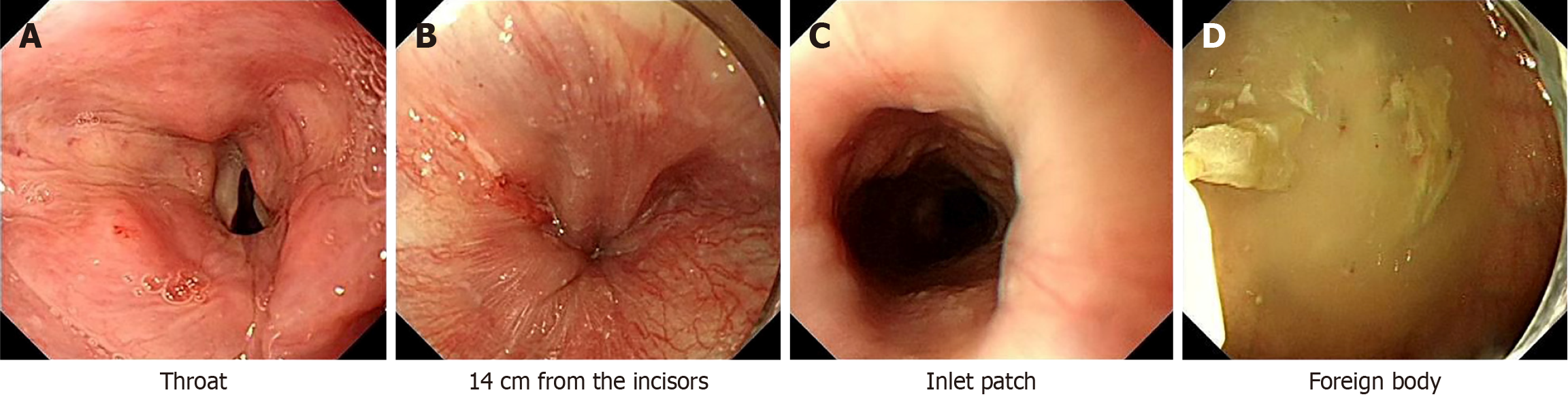
The patient underwent esophageal endoscopy under deep sedation and analgesia induced by midazolam (1 mg), sufen
Postoperatively, the patient was transferred to the emergency ward, where she received rehydration, blood pressure management, and anti-infective therapy. Her vital signs remained stable throughout these interventions, and no compli
Foreign body ingestion and food impactions are common clinical emergencies. While most cases resolve spontaneously, approximately 10%-20% of cases require intervention[1]. While smooth-edged foreign bodies typically do not pose significant issues, sharp-edged ones can lead to serious complications. The most common symptoms include dysphagia, odynophagia, retrosternal pain, throat pain, sensation of a foreign body, retching, vomiting, choking, and hypersalivation. Endoscopy is a reliable and well-established method for removing various types of upper gastrointestinal foreign bodies, with careful pre-procedure evaluation of the foreign body size, shape, location, and its relationship to adjacent structures being essential for optimal management[5-7]. In the present case, dislodgement of the foreign body occurred during gastroscopic clamping, influenced by several contributing factors: First, the foreign body was a sharp bone fragment, a cervical CT scan demonstrated its initial lodgment in the proximal esophagus 14 cm from the incisors. Subsequent endoscopic evaluation revealed migration of the object to the gastric fundus. The fragment exhibited a surface coating with adherent debris and gastric secretions, making it smooth and more prone to dislodgement. Second, the narrow and angular lumen of the pharynx created increased friction against the sharp edges of the bone, facilitating its displacement. Finally, the angle at which the foreign body was clamped might not have aligned with the direction of the gastroscope's travel, which could also have contributed to its dislodgement. These factors underscore the complexities of foreign body retrieval and the critical importance of using a careful technique during endoscopic procedures. Aspi
This case highlights the complexities of foreign body ingestion and the potential for unexpected complications during endoscopic treatment, such as displacement and aspiration. The absence of typical signs, such as coughing, does not rule out aspiration, especially under deep sedation and analgesia. Older patients, with reduced airway reflex sensitivity, are at higher risk of aspiration. Timely interventions, including bedside imaging, play a critical role in diagnosing and ma
| 1. | Geng C, Li X, Luo R, Cai L, Lei X, Wang C. Endoscopic management of foreign bodies in the upper gastrointestinal tract: a retrospective study of 1294 cases. Scand J Gastroenterol. 2017;52:1286-1291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 55] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 2. | Cha MH, Sandooja R, Khalid S, Lao N, Lim J, Razik R. Complication rates in emergent endoscopy for foreign bodies under different sedation modalities: A large single-center retrospective review. World J Gastrointest Endosc. 2021;13:45-55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Erskine RJ, Murphy PJ, Langton JA, Smith G. Effect of age on the sensitivity of upper airway reflexes. Br J Anaesth. 1993;70:574-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 44] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Ebihara S, Ebihara T, Kohzuki M. Effect of aging on cough and swallowing reflexes: implications for preventing aspiration pneumonia. Lung. 2012;190:29-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 67] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 5. | Pokharel R, Adhikari P, Bhusal CL, Guragain RP. Oesophageal foreign bodies in children. JNMA J Nepal Med Assoc. 2008;47:186-188. [PubMed] |
| 6. | Zhao XJ, Yu D K, Wang H H, Li A Q, Wang X, Xie H, Cheng Z M, Sheng J Q. [The experience of endoscopic removal foreign bodies in upper digestive tract]. Weichangbingxue He Ganbingxue Zazhi. 2011;20:829-830. [DOI] [Full Text] |
| 7. | Zhang S, Cui Y, Gong X, Gu F, Chen M, Zhong B. Endoscopic management of foreign bodies in the upper gastrointestinal tract in South China: a retrospective study of 561 cases. Dig Dis Sci. 2010;55:1305-1312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 78] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 8. | Limper AH, Prakash UB. Tracheobronchial foreign bodies in adults. Ann Intern Med. 1990;112:604-609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 232] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 9. | Boyd M, Watkins F, Singh S, Haponik E, Chatterjee A, Conforti J, Chin R Jr. Prevalence of flexible bronchoscopic removal of foreign bodies in the advanced elderly. Age Ageing. 2009;38:396-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Tagaito Y, Isono S, Nishino T. Upper airway reflexes during a combination of propofol and fentanyl anesthesia. Anesthesiology. 1998;88:1459-1466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 116] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 11. | Hayashi H, Abe A, Ota M, Momokita M, Ishihama T, Furuta H, Taniguchi T, Takeuchi K. Endoscopic removal of accidental aspirated and ingested dental foreign bodies: A cross-sectional study. Medicine (Baltimore). 2021;100:e27602. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Hajjar WM, Aljurayyad RS, Al-Jameel NI, Shaheen IS, Al-Nassar SA. Unusual case of inhaled metallic dental bur during dental procedure in a healthy adult. Saudi J Anaesth. 2016;10:465-467. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Leuzzi G, Kawamukai K, Lacava N. An unusual foreign body after dental filling. Lung. 2013;191:677-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Aydin O, Birbilen AZ, User IR, Turer OB, Teksam O. Lung ultrasound findings in children with foreign body aspiration. J Clin Ultrasound. 2023;51:447-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |