Published online Sep 26, 2025. doi: 10.12998/wjcc.v13.i27.108003
Revised: April 30, 2025
Accepted: June 16, 2025
Published online: September 26, 2025
Processing time: 125 Days and 7.5 Hours
To treat flexor pollicis longus (FPL) muscle function loss, the 4th flexor digitorum superficialis (FDS) to the FPL tendon transfer is preferred as a reconstruction method. Various complications can occur during transfer. However, median nerve neuropathy has not been reported yet. We present a case of median nerve neuropathy caused by irritation of suture knots of the 4th FDS to the FPL tendon transfer with a review of the literature.
A 52-year-old male patient presented with paresthesia along median nerve distribution of right hand after tendon transfer. He complained of right thumb flexion limitation due to FPL function loss so authors performed the 4th FDS to FPL transfer using Pulvertaft weave technique. FPL function loss was due to adhesion resulting from repeated surgery of radius shaft. He had a history of radius shaft open fracture 9 years ago and nonunion 7 years ago. During surgery, FPL muscle was severely adhered and indistinguishable. However, tendon continuity remained intact. After tendon transfer, he experienced paresthesia along median nerve distribution upon movement of thumb. He was diagnosed with median nerve neuropathy caused by irritation of tendon suture knots. Exploration was then performed. The median nerve was irritated by suture knots of transferred tendon. Thus, knots were removed. Twelve months later, he demonstrated thumb flexion of 80°. Additionally, median nerve neuropathy symptoms fully resolved.
Median nerve neuropathy can occur after tendon transfer from irritation of suture knots. Covering knots using surrounding tissue is recommended.
Core Tip: Median nerve neuropathy can occur as a complication of flexor tendon reconstruction using the Pulvertaft weave technique at wrist due to irritation of tendon suture knots. Thus, physicians should be aware of nerve irritation as a possible complication of tendon reconstruction and prevent it. The preventive method to cover tendon suture knots using surrounding tissue such as deep transverse carpal ligament dissected during the approach is recommended.
- Citation: Ho JW, Lee YK. Median nerve neuropathy after flexor pollicis longus tendon reconstruction: A case report. World J Clin Cases 2025; 13(27): 108003
- URL: https://www.wjgnet.com/2307-8960/full/v13/i27/108003.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i27.108003
Several treatment options including tendon direct repair, interphalangeal (IP) joint fusion, and tendon reconstruction have been proposed for functional recovery of thumb flexion limitation caused by flexor pollicis longus (FPL) closed rupture or muscle function loss. Among these treatment options, tendon reconstruction has emerged as a more favorable approach[1,2]. Several methods can be used to reconstruct the FPL tendon, including free tendon grafts from the palmaris longus and tendon transfers from the fourth flexor digitorum superficialis (FDS) to the FPL tendon. Among these methods, the 4th FDS to FPL tendon transfer at the wrist level is more commonly used than others, showing good results[1,3].
The Pulvertaft weave technique is frequently used for tendon repair during tendon transfer because it can provide sufficient strength to withstand early exercise after surgery[4]. Complications of tendon transfer for FPL reconstruction have been reported, including adhesion and suture pullout or failure[2,5,6]. However, median nerve neuropathy has not been reported yet. The authors report a case of median nerve neuropathy caused by irritation of tendon suture knots in the 4th FDS tendon transfer using the Pulvertaft weave technique for FPL tendon reconstruction accompanied by a literature review.
A 52-year-old male patient presented with paresthesia along median nerve distribution of right hand after the 4th FDS to FPL tendon transfer surgery.
There were no symptoms immediately after the surgery. A dorsal block splint was applied and his right thumb was immobilized for 1 week. Neurologic symptoms started at 1 week after tendon transfer surgery when he performed active extension-passive flexion exercises of his right thumb with dynamic splint applied.
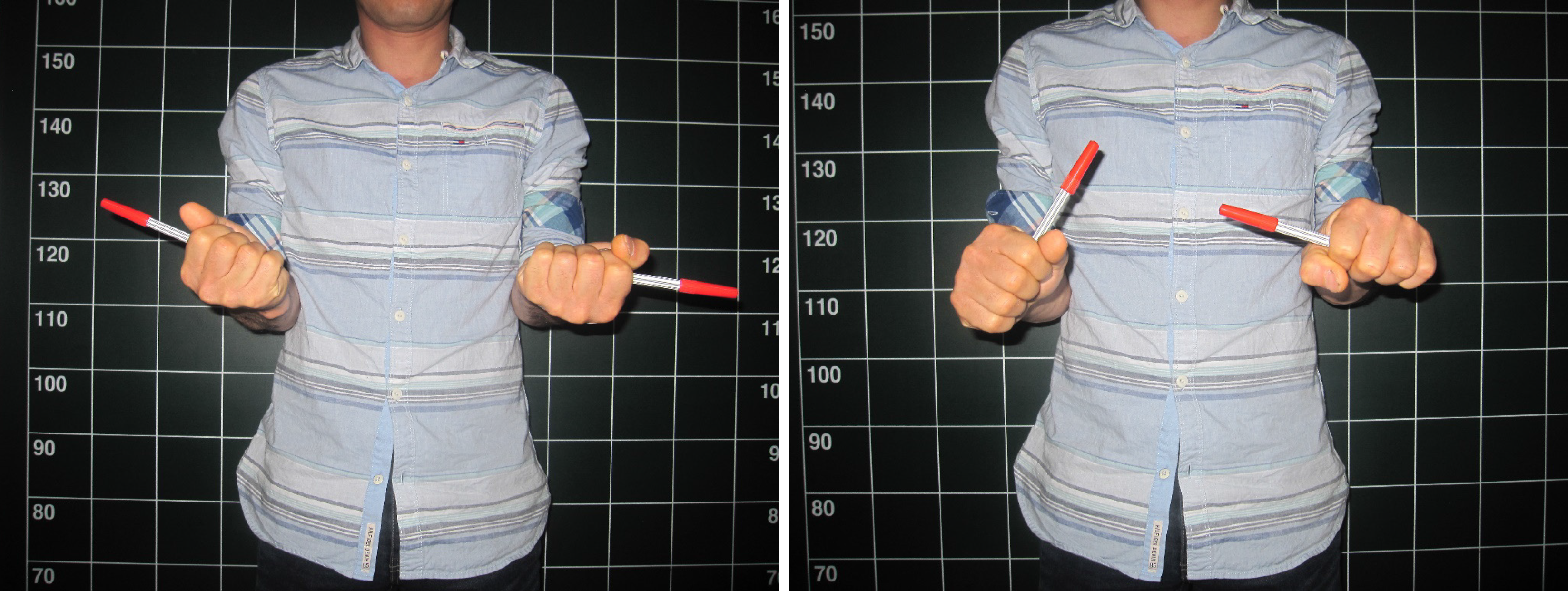
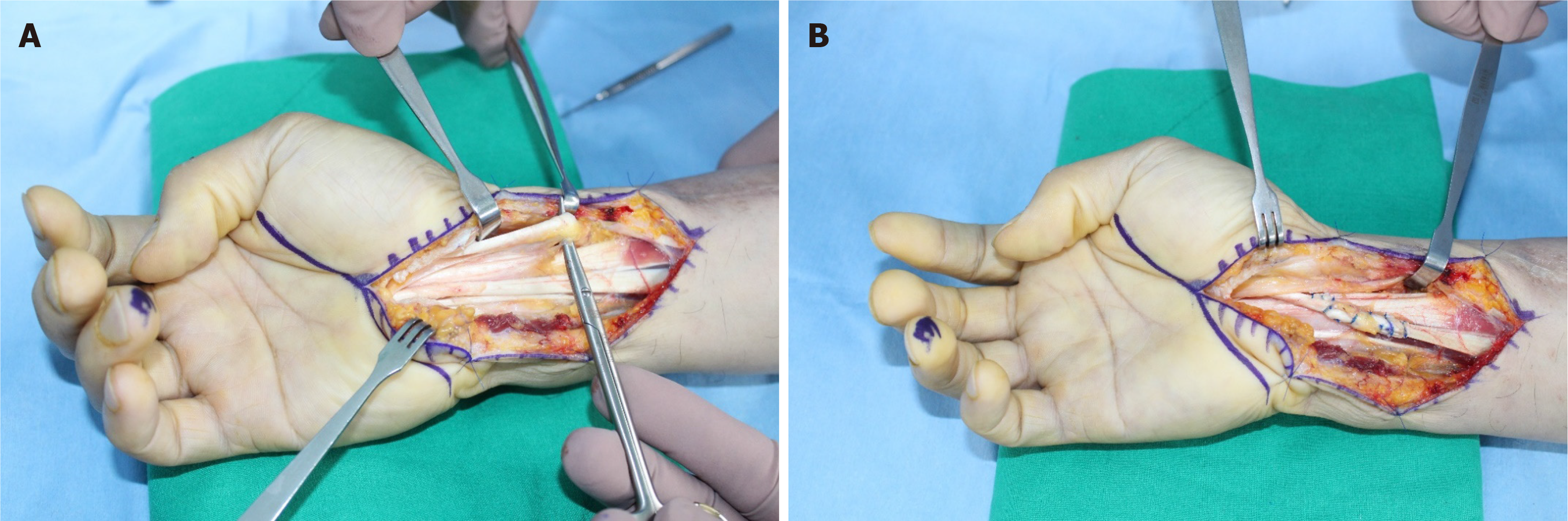
He had a history of radius shaft open fracture in his right forearm 9 years ago. Seven years ago, he presented to our institution with a nonunion and failure of internal fixation and underwent bone grafting. During the bone grafting surgery, there was specific finding of severe adhesion in the FPL muscle, rendering its normal structure indistinguishable. However, the continuity of the FPL remained intact. After that surgery, follow-up was lost. He visited our institution 7 years later due to complaint of thumb flexion limitation. The authors evaluated function and continuity of his FPL with physical examination, ultrasonography (US), nerve conduction study (NCS), and electromyography (EMG). Active flexion of the IP joint of the right thumb was not possible (Figure 1). US showed continuity of FPL tendon. However, there was no contraction of muscle in a dynamic view. NCS and EMG showed no abnormality. He was diagnosed with FPL function loss, which was thought to be due to muscle adhesion resulting from repeated surgery of radius shaft. Thus, the authors planned the 4th FDS to FPL tendon transfer to restore function of thumb flexion. Carpal tunnel release was initially done. The 4th FDS tendon was then harvested and transferred to the FPL tendon using the Pulvertaft weave technique with a 4-0 prolene suture at the wrist level (Figure 2).
In physical examination, the patient complained of paresthesia and tingling in his right hand, especially in his right index and middle fingers during active extension-passive flexion exercises of the thumb.
There was no specific laboratory finding.
No specific imaging examination was done.
The final diagnosis was median nerve neuropathy due to irritation of transferred tendon suture knots.
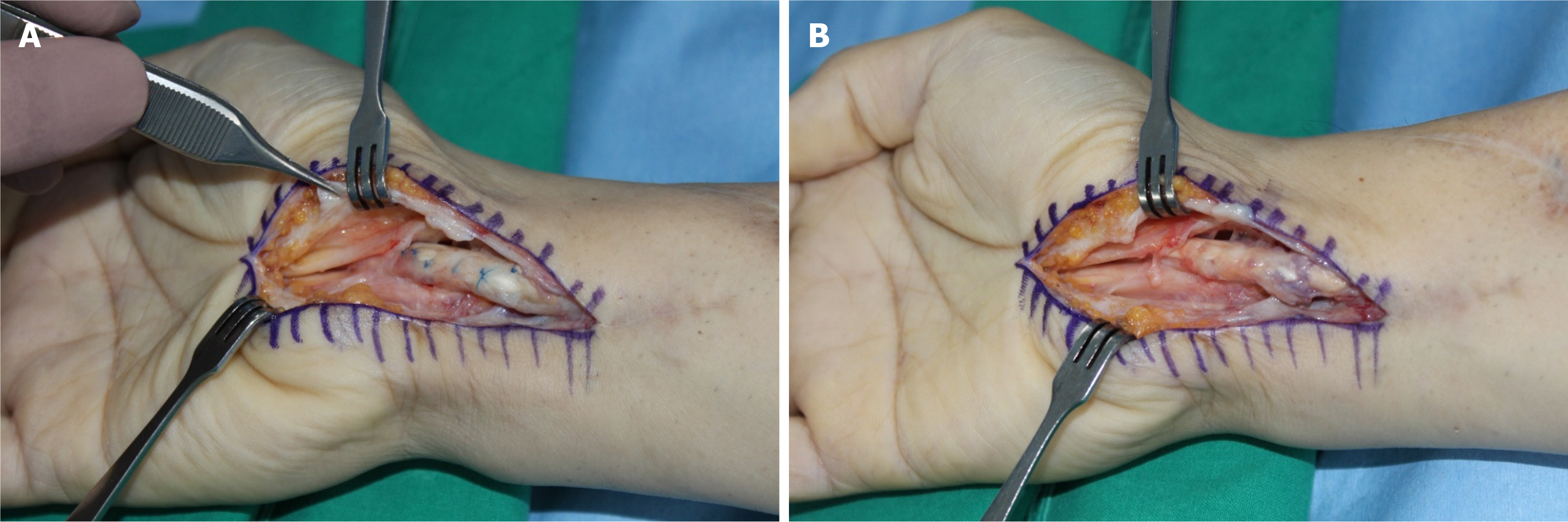
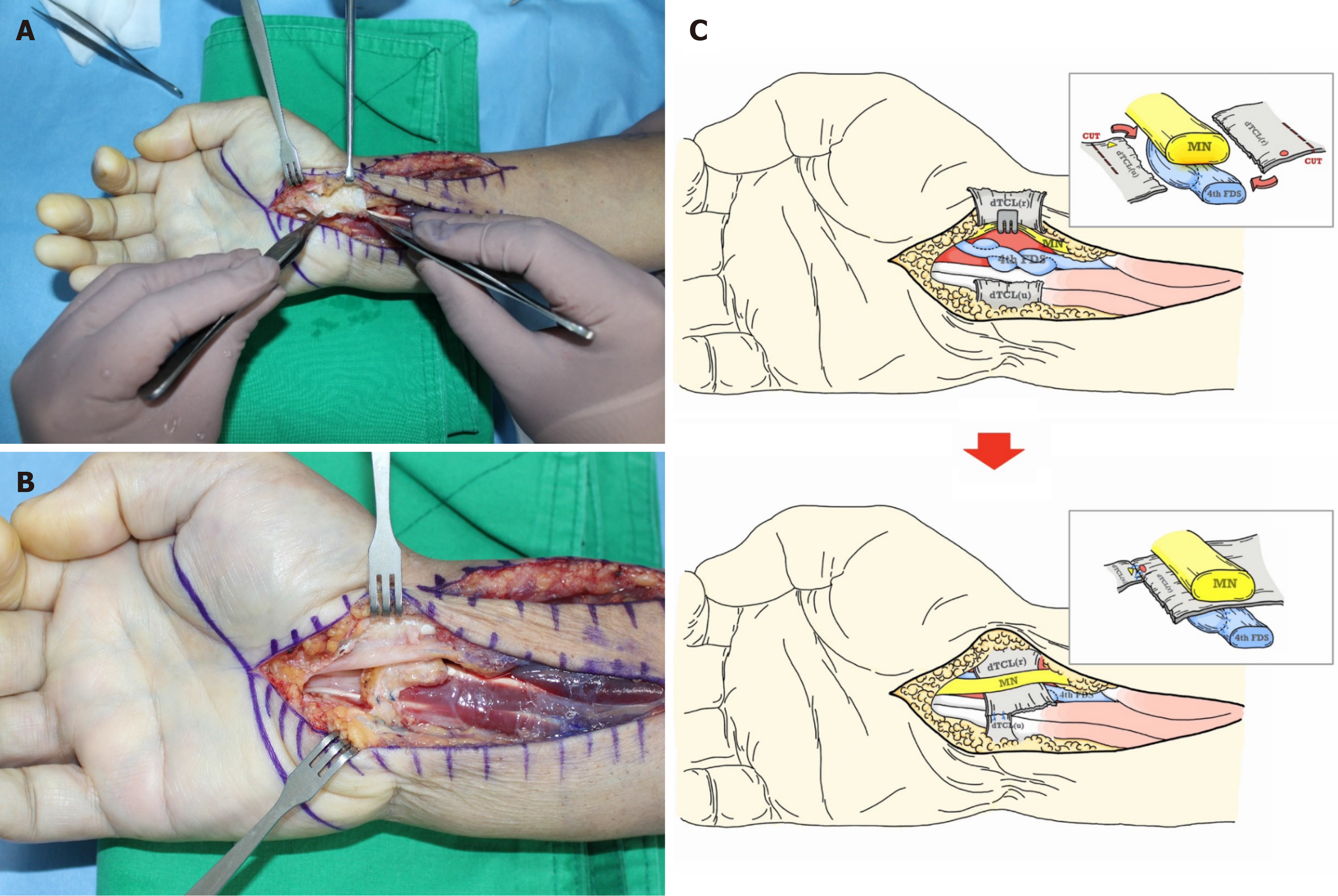
Despite discontinuing thumb exercises and immobilizing the thumb with a splint, there was no improvement in his symptoms. Three months after the tendon transfer surgery, exploration was performed under brachial plexus anesthesia to remove tendon suture knots. The median nerve was irritated by prolene knots at the suture site of the transferred tendon. Those prolene knots were carefully removed. Tendon transfer sites showed signs of healing (Figure 3).
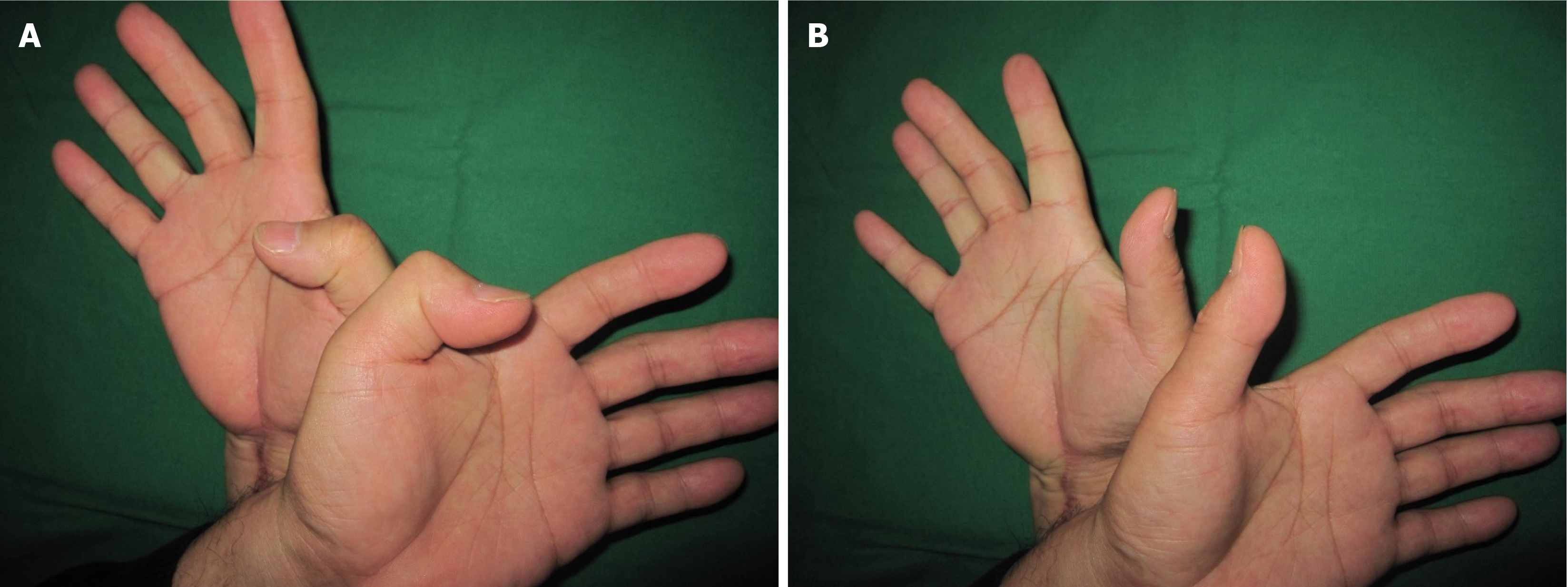
After the exploration, his symptoms of median nerve irritation gradually resolved. An additional 6 weeks of exercise with a dynamic splint was performed. Twelve months after the surgery, all symptoms of median nerve irritation in the right hand improved. On physical examination, active flexion of the right thumb IP joint was 80°, and extension was 0° (Figure 4). His grip strength was 25/25 kg and his pinch strength was 9/10 kg, showing improvement. His Quick Disabilities of Arm, Shoulder and Hand score was 0 points.
Closed rupture of flexor tendons, including the FPL tendon, is known to be caused by various factors, such as attrition of surrounding structures and chronic inflammatory status of the tenosynovium[1,7,8]. Closed tendon rupture of the FPL is often neglected, leading to complaints of limited active flexion of the thumb IP joint[1,3,7]. Thumb IP joint flexion is also restricted in cases with loss of function of the FPL muscle due to neuromuscular causes, such as nerve injury[2].
Thumb functions include flexion, abduction, and opposition. These functions are essential for daily human activities. Any limitations of these functions should be promptly addressed[2,9]. Various treatment options are available to restore these functions, including direct repair of the tendon, IP fusion, and tendon reconstruction techniques such as tendon transfer and free tendon graft[1,2,9]. Among reconstruction techniques for FPL, both tendon transfer and free tendon grafting can be considered. While there is no clear consensus on which technique is superior, tendon transfer is generally preferred because it could utilize the 4th FDS tendon, a viable tendon with normal excursion and strength, as a donor tendon[1]. Thus, it does not require tendon harvest. The Pulvertaft weave technique has long been the standard method for tendon transfer surgery[4]. This technique involves the creation of a slit in the recipient tendon and weaving the donor tendon through the slit. It has the advantage of providing sufficient strength to withstand active motion during early exercise after surgery[4,6]. Several complications of tendon transfer have been reported[2,5,6]. Among them, complications arising from the suture site have been explained to be caused by increased friction between the bulky reconstructed tendon using the Pulvertaft weave technique and surrounding tissues, leading to adhesion[6]. In the case of neurogenic complications, Brutus et al[10] have reported ulnar nerve neuropathy following extensor indicis proprius (EIP) tendon transfer for thumb opposition recovery. They performed ulnar nerve decompression at Guyon's canal in a patient who showed symptoms of ulnar nerve neuropathy after EIP tendon transfer. However, the patient’s symptoms did not improve. Therefore, they explored the tendon transfer site at 3 months after the initial surgery and found that the ulnar nerve was compressed by the transferred EIP tendon just proximal to the wrist. The neuropathy in our case was caused by irritation of the median nerve due to suture knots of the transferred tendon at the wrist level. We initially immobilized the patient with a splint while monitoring the progress and performed exploration and knot removal three months postoperatively. Titan et al[11] have described the healing process after flexor tendon repair in three phases. They reported that it took at least 2 months for the repaired tendon tissue to begin to mature and up to a year to heal through gradual changes. Therefore, premature removal of the suture material might lead to incomplete healing of the tendon repair site with an increased risk of re-rupture. We had experienced a re-rupture of the transferred tendon after suture knot removal 6 weeks postoperatively in a patient with hematoma caused by knot irritation following tendon transfer. Therefore, after careful discussion with the patient, we decided to remove suture knots at 3 months postoperatively when the tingling sensation was not severe. No re-rupture occurred after suture knots were removed. Therefore, surgeons should carefully consider complications (adhesion, pullout, nerve compression, and irritation) associated with tendon suture sites when performing tendon transfers.
To reduce these complications, Koopman et al[6] have proposed a double-sided nonlocking side-to-side (STS) technique and a single-sided locking STS method. These methods offer similar strength to the Pulvertaft weave technique, However, they are less bulky with fewer complications. These two STS techniques could lead a significant increase in strength and a decrease in cross-sectional area compared with the Pulvertaft weave technique. However, the suture material and knots outside the tendon are risk factors as they could cause friction and irritation to surrounding tissues.
Graham et al[4] have conducted a meta-analysis of 15 biomechanical studies on Pulvertaft weave techniques and found that smaller suture materials are preferred for surgeries performed on the hand considering characteristics of the surgery. Smaller suture materials also could minimize tissue injury. Additionally, they reported that braided multifilament sutures had greater strength than monofilament sutures. However, non-braided sutures are generally preferred because braided sutures allow adhesion and pathogens to adhere more easily. Based on these research results, selecting and using appropriate suture size and material can minimize friction and irritation caused by knots. However, there might be a limitation in the strength and an increased risk of pull-out. Neurological complications following tendon transfers are extremely rare. Definitive treatment strategies have not yet been established. Brutus et al[10] have described a solution for this problem. They rerouted the transfer deeper through revision surgery to prevent nerve compression caused by a reconstructed tendon after the onset of neurological complications.
In the present case, the authors aimed to present methods to prevent irritation of surrounding nerves during flexor tendon transfer at the wrist level. After experiencing this case, we had the opportunity to perform the 4th FDS to 2nd flexor digitorum profundus transfer at the wrist level using the Pulvertaft weave technique. The dissected deep transverse carpal ligament (TCL) was used to cover the tendon suture site. The surgical procedure was performed as follows. First, incisions were made on a portion of the attached ulnar leaflet and on a portion of the attached radial leaflet of the deep TCL. Each leaflet was rotated to increase its length. These leaflets were then positioned beneath the median nerve and above the reconstructed tendon repair site. They were sutured together using a 4-0 prolene suture (Figure 5). Using this technique, we were able to avoid contact between tendon suture knots and median nerve. The patient subsequently regained index finger flexion, which was maintained without symptoms of nerve irritation.
Most tendon transfers for closed ruptures of the flexor tendons and flexor muscle function loss are performed at the wrist level[2,3]. During flexor tendon transfer, the median nerve is inevitably exposed to more irritation owing to its anatomical proximity to the flexor tendons. Through this study, the authors suggested a surgical technique to cover the suture site of the transferred tendon utilizing the deep TCL dissected during flexor tendon transfer in the wrist. This method uses exposed structures without additional incisions. It uses the patient's own tissues instead of an allograft. It is also useful considering its risk-benefit, as it can achieve the primary goal of tendon transfer while preventing complications.
For differential diagnoses, the cause of median nerve neuropathy includes compressive neuropathy, neurogenic tumor, and trauma. In our case, compressive neuropathy such as carpal tunnel syndrome was ruled out because we performed carpal tunnel release during the tendon transfer procedure. Neurogenic tumor or traumatic injury was also ruled out during the tendon transfer by directly securing and protecting the median nerve to avoid neurovascular injury. If a neurogenic tumor or trauma had been already present in the nerve, abnormal findings would have been visually confirmed. Furthermore, the patient's symptoms showed sudden onset immediately after tendon transfer. Thus, we were certain that the symptom was due to irritation of transferred tendon suture knots.
One limitation of this study was that the diagnosis of median nerve neuropathy was solely based on clinical presentation. This diagnosis was possible because of the experience of the senior surgeon. Considering that complications in this case were related to problems at the Pulvertaft suture site, further research and analysis of more cases are necessary to find a solution to the root cause.
Surgeons should be aware that median nerve neuropathy could occur as a complication of flexor tendon reconstruction using the Pulvertaft weave technique at the wrist due to irritation of tendon suture knots. This will enable them to provide more accurate explanations to patients, achieve better treatment outcomes, and prevent complications. A preventive method to cover tendon suture knots using the deep TCL dissected during the approach is also suggested in this study.
| 1. | Shafaei Y, Tassallibakhsh M, Akhoondinasab M, Latifi N. Comparison of the Results of Delayed Repair of Flexor Pollicis Longus (FPL) Tendon with Tendon Transfer or with Tendon Graft. World J Plast Surg. 2023;12:64-70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Soucacos PN, Touliatos A, Johnson EO. Tendon transfers for median, radial and ulnar nerve palsies. In: Bentley G, editor. European surgical orthopaedics and traumatology. Berlin: Springer, 2014: 1579-1593. |
| 3. | Schmitt S, Mühldorfer-Fodor M, van Schoonhoven J, Prommersberger KJ. [Restoration of thumb flexion at the interphalangeal joint by transposition of the flexor digitorum superficialis tendon from the ring finger]. Oper Orthop Traumatol. 2013;25:321-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Graham EM, Oliver J, Hendrycks R, Mendenhall SD. Optimizing the Pulvertaft Weave Technique: A Comprehensive Systematic Review of Comparative Biomechanical Studies. Plast Reconstr Surg. 2022;150:357-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 5. | Seiler JG 3rd. Flexor tendon injury. In: Wolfe SW, Pederson WC, Kozin SH, Cohen MS, editors. Green’s operative hand surgery. 8th ed. Amsterdam: Elsevier, 2021: 212-259. |
| 6. | Koopman JE, Hundepool CA, Duraku LS, Kreulen M, Zuidam JM. Biomechanical Study Comparing Pulvertaft, Double Side-to-Side, and Locking Side-to-Side Tendon Suture Techniques. J Hand Surg Am. 2021;46:246.e1-246.e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Netscher DT, Badal JJ. Closed flexor tendon ruptures. J Hand Surg Am. 2014;39:2315-23; quiz 2323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Berger P, Duerinckx J. Flexor Pollicis Longus Tendon Rupture After Volar Wrist Plating : Reconstruction With Palmaris Longus Interposition Graft. Acta Orthop Belg. 2017;83:467-472. [PubMed] |
| 9. | Cannon DL. Flexor and extensor tendon injuries. In: Azar FM, Canale ST, Beaty JH, editors. Campbell’s operative orthopedics. 14th ed. Amsterdam: Elsevier, 2020: 3464-3481. |
| 10. | Brutus JP, Mattoli JA, Palmer AK. Unusual complication of an opposition tendon transfer at the wrist: ulnar nerve compression syndrome. J Hand Surg Am. 2004;29:625-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Titan AL, Foster DS, Chang J, Longaker MT. Flexor Tendon: Development, Healing, Adhesion Formation, and Contributing Growth Factors. Plast Reconstr Surg. 2019;144:639e-647e. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 89] [Article Influence: 17.8] [Reference Citation Analysis (0)] |