Published online Sep 16, 2025. doi: 10.12998/wjcc.v13.i26.108308
Revised: May 8, 2025
Accepted: May 28, 2025
Published online: September 16, 2025
Processing time: 92 Days and 17.3 Hours
Retroperitoneal liposarcoma (RPLS) is a rare malignant tumor initiated in adipo
The patient, a 62-year-old woman, presented to the hospital complaining of abdo
Surgical resection is the only radical treatment for giant RPLS. Preoperative pre
Core Tip: Retroperitoneal liposarcoma (RPLS) is a rare malignant tumor. When its diameter exceeds 30 cm or its weight is no less than 20 kg, it is classified as giant RPLS, which significantly increases the complexity of surgical intervention. Giant RPLS may necessitate concomitant resection of adjacent organs and cannot be completely resected, leading to a high recurrence rate and suboptimal treatment outcomes.
- Citation: Cheng LL, Tang B, Liu H, Zhu F, Chen YF, Zhang W. Thoughts and challenges of giant retroperitoneal liposarcoma: A case report. World J Clin Cases 2025; 13(26): 108308
- URL: https://www.wjgnet.com/2307-8960/full/v13/i26/108308.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i26.108308
Retroperitoneal liposarcoma (RPLS) is a rare malignant tumor originating from adipose tissue and accounts for < 1% of all malignant tumors[1]. The age of onset is primarily between 55 years and 75 years, and there are slightly more males than females[2]. Due to its deep location and concealed onset, the clinical manifestations of RPLS are not obvious, and there are no typical symptoms or signs. A few patients only experience compression symptoms of abdominal organs, which are often massive tumors at diagnosis, especially those with a diameter of > 30 cm or a weight of ≥ 20 kg, called giant RPLS[3], which seriously increases the difficulty of surgery. It may be combined with other organ resection or may not be completely resected, the recurrence rate is high, and the treatment effect is not ideal. This article describes a case of a giant RPLS with a maximum diameter of 35 cm and a weight of 17 kg. The tumor adhered tightly to the bilateral ure
Abdominal distension for over six months.
The patient, a 62-year-old female, was admitted to Yichang Central Hospital with a chief complaint of "abdominal distension for over six months". Abdominal ultrasound revealed a large retroperitoneal mass suspected to be a lipoma (extending from the subxiphoid region to the pubic symphysis, right to the adrenal gland, and left to the splenic flexure of the colon). For further evaluation and treatment, she was admitted to Tongji Hospital, Affiliated with Tongji Medical College of Huazhong University of Science and Technology, on February 7, 2025, with a provisional diagnosis of retro
Her medical history included hypertension for 5 years that was adequately managed with oral nifedipine sustained-release tablets.
The patient's family history had no notable findings.
Physical examination revealed marked abdominal distension (abdominal circumference: 95 cm), with a palpable, massive, soft and ill-defined abdominal mass, without tenderness or rebound pain.
Laboratory examinations show no significant abnormalities.
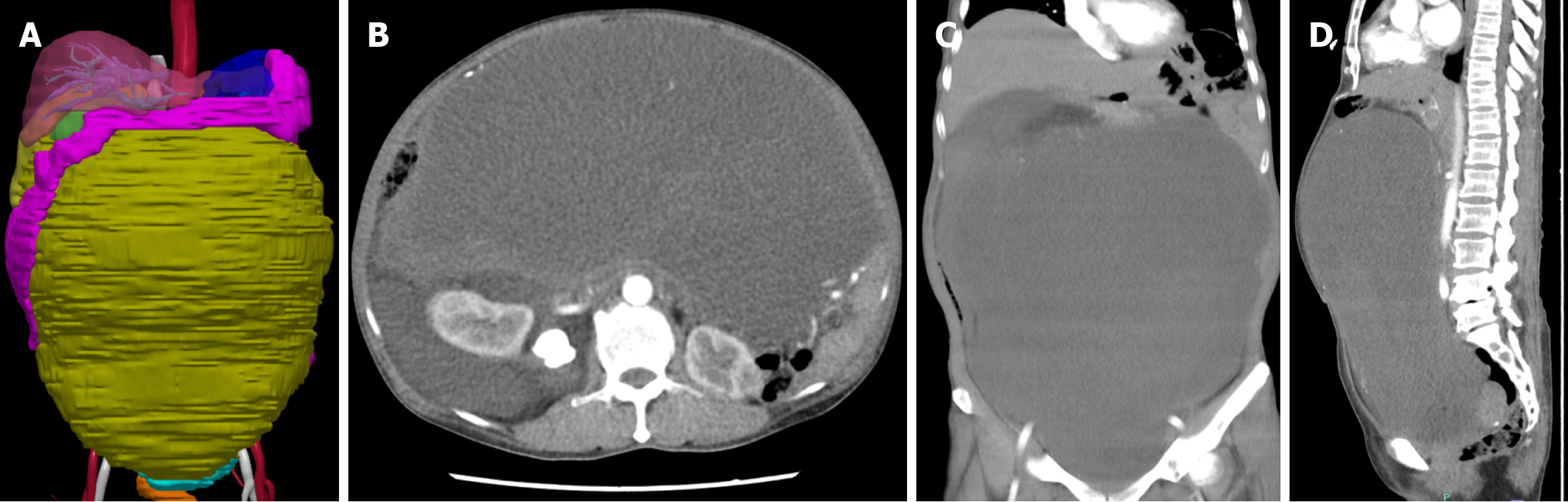
Contrast-enhanced abdominal computed tomography (CT) further revealed a giant retroperitoneal mass, suggestive of a neoplastic lesion, likely liposarcoma. Additional findings included a nodule in the right hepatic lobe (suspected heman
Giant RPLS (high differentiation).
Ultrasound-guided tumor biopsy was performed, and histopathological analysis revealed a mesenchymal tissue-derived tumor. Subsequent immunohistochemical and molecular detection confirmed the diagnosis of liposarcoma (considering high differentiation). To prevent intraoperative ureteral injury, bilateral ureteral stents were preoperatively placed via cystoscopy under general anesthesia. The surgery was performed on February 19, 2025, and involved resection of the giant retroperitoneal mass.
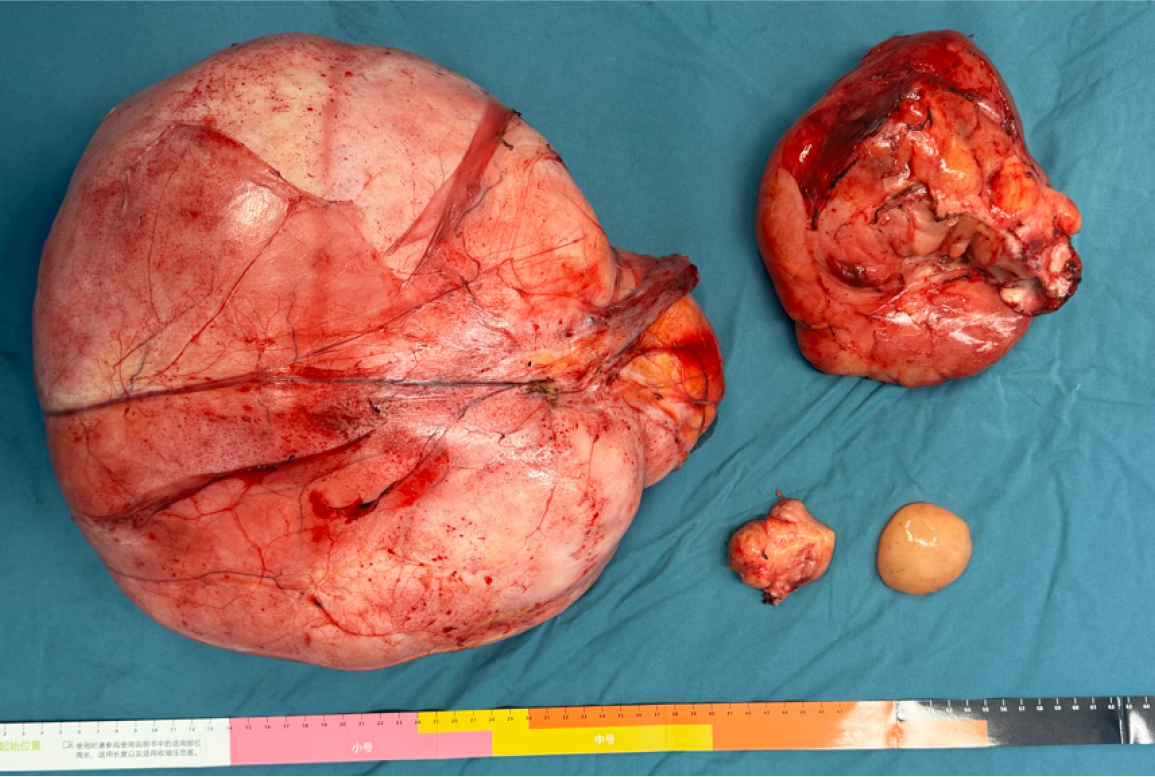
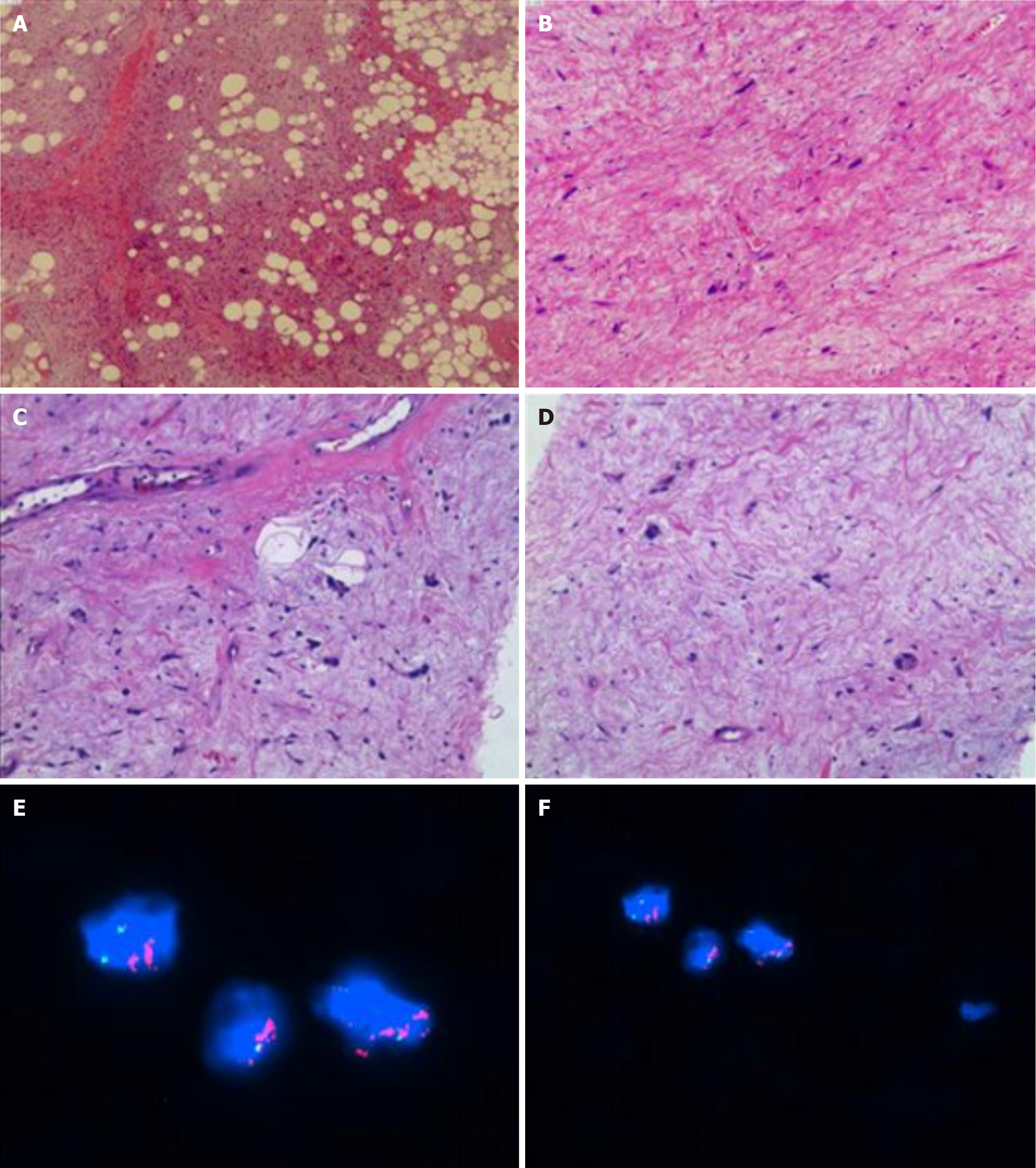
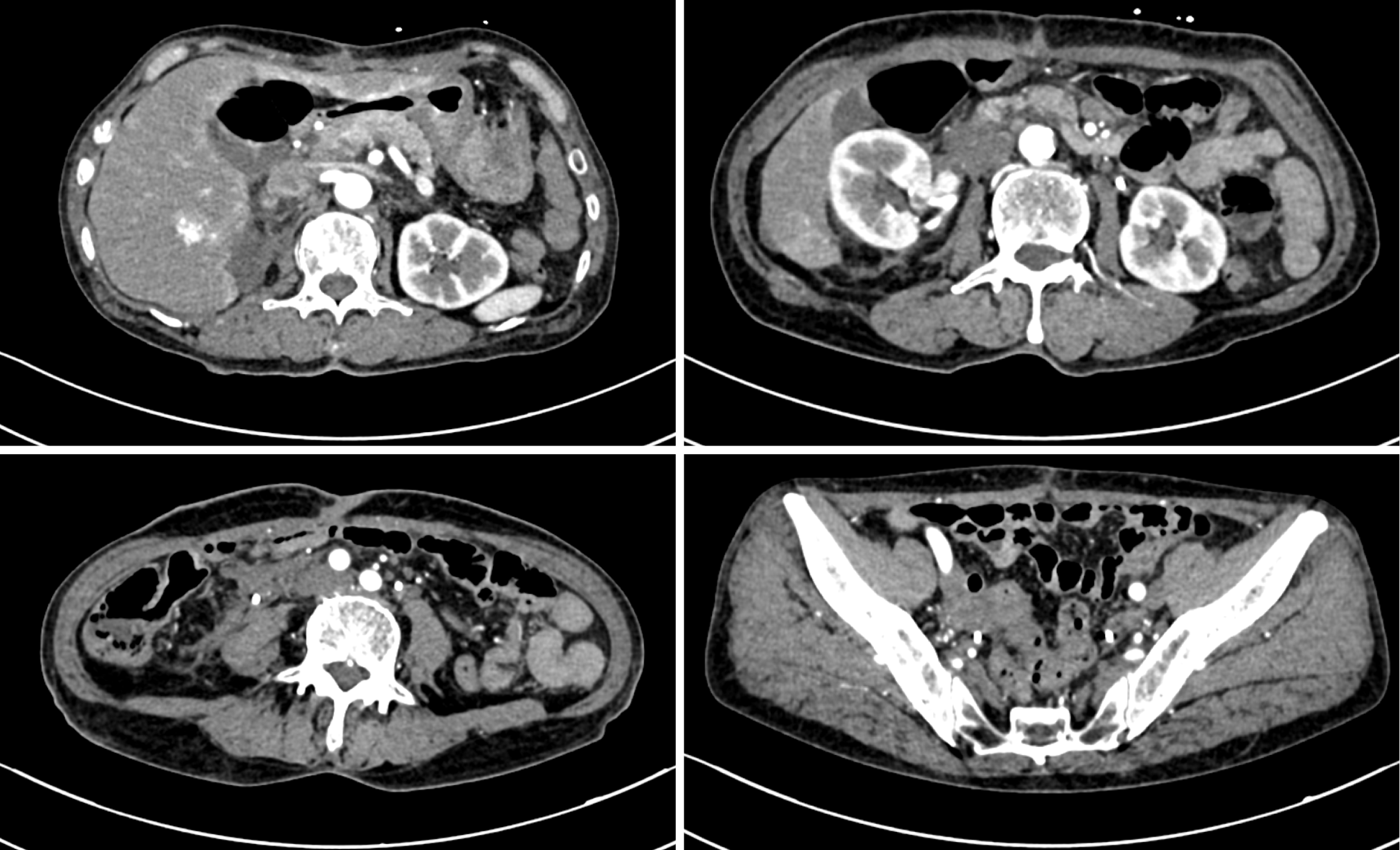
The tumor was completely removed and consisted of multiple masses, with a total weight of 17 kg and the largest mass size of 35 cm × 28 cm × 14 cm (Figure 2). Postoperative pathological examination and molecular results of the puncture specimen (II25-08446) confirmed a well-differentiated liposarcoma (WDLS)/atypical lipomatous tumor. Immunohistochemical analysis revealed the following marker profile: (1) Mouse double minute 2 (MDM2) (+); (2) Cyclin-dependent kinase 4 (CDK4) (+); (3) P16 (+); (4) S-100 (+); and (5) Ki-67 (labeling index of approximately 10%). Molecular detection revealed MDM2 gene expansion (Figure 3). The patient recovered uneventfully and was discharged on postoperative day 15. Later, radiation therapy was performed in the oncology department. At a follow-up of 2 months, a reexamination of contrast-enhanced CT of the whole abdomen revealed no evidence of recurrence (Figure 4).
RPLS is insidious and usually asymptomatic in the early stage. Due to the loose anatomical structure of the retroperitoneal space and the absence of rigid bony boundaries, retroperitoneal tumors often grow rapidly. As the mass grows, patients may develop abdominal distension and pain, and these symptoms are particularly exacerbated postprandially and accompanied by mild dyspepsia[4]. Patient evaluation is frequently delayed until palpable abdominal masses or local compressive symptoms manifest. By the time of hospital consultation, these tumors commonly exceed 20 cm in diameter, with an average weight of 15–20 kg[5]. Sun et al[6] conducted a comprehensive review of all the literature in the PubMed database and identified only 34 reported cases of giant RPLS (RPLS exceeding 30 cm in diameter). Among these 35 patients, 23 patients were male (65.7%), and 12 were female (34.3%). Giant RPLS is extremely rare. At present, there is a lack of clinical experience in its diagnosis, treatment, prognosis and follow-up, which poses a great challenge to doctors. Based on the literature, the difficulties in the diagnosis and treatment, surgical decision-making and long-term prognosis of giant RPLS are discussed below.
The preoperative diagnosis of giant RPLS relies heavily on imaging evaluation; however, distinguishing it from benign lipomas remains challenging. Previous reports indicate that well-differentiated RPLS typically presents on CT or magnetic resonance imaging (MRI) as predominantly lipomatous lesions. However, the presence of lipomatous lesions accompanied by septations or nodular enhancement should raise suspicion for malignancy[7-9]. However, the accuracy of imaging modalities in predicting histological subtypes is limited. In the present case, preoperative imaging revealed that the patient was initially misdiagnosed with "retroperitoneal lipoma", similar to the misdiagnosis reported by Nureta et al[10]. These findings emphasize the need to maintain a high degree of clinical suspicion for malignancy when evalua
Surgery remains the primary treatment for giant RPLS. A comprehensive evaluation of the tumor size, growth rate and clinical symptoms is needed to determine the optimal timing of surgery. Studies have recommended early surgery for patients with tumors > 5 cm in diameter or those presenting with compression symptoms, whereas immediate resection is advised for giant RPLS (diameter > 30 cm) upon diagnosis[11]. Achour et al[12] reported a case of giant RPLS mea
Preoperative preparation necessitates comprehensive imaging evaluation (CT/MRI) to delineate tumor-to-surrounding structural relationships, supplemented by multidisciplinary team consultation if necessary[13]. For hypervascular tumors, preoperative arterial embolization serves to mitigate the risk of intraoperative hemorrhage[5]. Given the substantial tumor burden of giant RPLS and the inherent complexity of the retroperitoneal anatomy, iatrogenic injury to adjacent structures—including the descending colon, pancreas, kidneys, and ureters—is a critical concern. Surgical challenges increase significantly when tumors infiltrate neighboring organs, tissues, or musculature. To address these risks, three-dimensional visualization reconstruction may be employed preoperatively. Compared with conventional CT and MRI, this advanced modality has enhanced spatial resolution, enabling comprehensive anatomical mapping of tumor inter
Complete surgical resection (R0/R1) constitutes the cornerstone for giant RPLS management, improving the 5-year survival rates from 16.7% to 58%[6]. For giant RPLS, resection of the involved organs is frequently required to achieve R0 margins. Santangelo et al[15] systematically reviewed 157 RPLS resection cases and reported that approximately 65% necessitated the resection of adjacent organs (such as the kidneys, colon or musculature), which significantly increased the recurrence rates observed in patients who underwent tumor debulking alone compared with multivisceral resection cohorts. However, the literature also indicates that multivisceral resection may increase the risk of postoperative complications, so there is a particular need to carefully evaluate organ preservation in younger patients to balance functional outcomes[16]. Notably, some scholars advocate for organ preservation in the absence of definitive histopathological invasion. For example, Rachman and Hardja[3] reported a case of a 30-cm RPLS managed via tumor resection alone, achieving 3-month recurrence-free survival, suggesting that meticulous fascial plane dissection without radical resection may suffice for well-differentiated subtypes. Nevertheless, the pseudocapsule structure of RPLS often adheres to adjacent tissues, rendering intraoperative determination of "safe margins" heavily reliant on the experience of the surgeon. Wei et al[17] reported that a series of giant RPLS resulted in severe compression and deviation of the left ureter. During the operation, the iliac vessels, mesenteric vessels and other large vessels and tumor tissues were finely separated, and the ureter was protected to achieve complete resection of the tumor. The peripheral blood vessels and ureter were protected. Consequently, preoperative planning should be integrated with three-dimensional image reconstruction and intraoperative frozen pathology to dynamically adjust the resection boundaries.
The debate persists regarding whether tumor size is an independent risk factor for recurrence. Marjiyeh-Awwad et al[11], in a comprehensive review, emphasized that while large, well-differentiated RPLS has a high recurrence risk, histological subtype and margin status (R0 vs R1) remain the paramount prognostic determinants. The World Health Organization classifies liposarcoma into five principal subtypes: (1) WDLS; (2) Dedifferentiated liposarcoma (DDLS); (3) Myxoid liposarcoma; (4) Pleomorphic liposarcoma (PLS); and (5) Myxoid PLS[18]. The histological subtype serves as the primary prognostic indicator for local recurrence and distant metastasis. While well-differentiated variants demonstrate favorable prognoses, the presence of dedifferentiated components markedly increases malignant potential. The literature has shown that WDLS accounts for 40%-50% of RPLS cases and is characterized by strong local proliferative capacity but low metastatic rates, whereas DDLS and PLS are associated with significantly greater risks of recurrence and metastasis[19]. In the present case, postoperative pathology confirmed WDLS with focal dedifferentiation, a feature that aligns with the clinicopathological profile reported by Mansour et al[5]. This underscores the inherent heterogeneity of such tumors and the need for extensive tissue sampling to avoid underdiagnosis of aggressive components. A recent systematic analysis revealed that recurrence is not significantly correlated with tumor volume but is strongly associated with the presence of dedifferentiated components and margin status[15].
The efficacy of postoperative radiotherapy or chemotherapy in reducing the recurrence rate remains unclear. It is gene
In light of the high local recurrence risk of RPLS (40%-80%)[15], contrast-enhanced abdominal CT or MRI is recom
Giant RPLS is a rare malignancy with insidious onset that is often diagnosed at an advanced stage. Surgical resection is the only radical treatment, and CT and MRI serve as cornerstone diagnostic tools. Three-dimensional visualization/reconstruction aids in preoperative planning. Reoperation can still be performed to treat local recurrence. For metastatic or unresectable tumors, radiotherapy and neoadjuvant therapies may be reasonably selected. In addition, multidisciplinary collaboration is critical, particularly in cases involving adjacent organ infiltration. Long-term postoperative surveillance is imperative because of the disease’s propensity for recurrence.
| 1. | Díaz de León-Romero CE, Jiménez-Yarza M, Pérez-Tristán CE, Jiménez-Yarza LE, Valdes-Ramos RL, Ortiz-Cisneros JD. Giant myxoid retroperitoneal liposarcoma in a 41-year-old patient: A case report. Int J Surg Case Rep. 2023;109:108572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 2. | Nirhale DS, Modi V, Kulkarni AA. Giant Retroperitoneal Liposarcoma: A Rare Surgical Occurrence. Cureus. 2024;16:e76192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | Rachman Y, Hardja Y. Giant retroperitoneal liposarcoma: A case report. Int J Surg Case Rep. 2022;97:107465. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 4. | Xu C, Ma Z, Zhang H, Yu J, Chen S. Giant retroperitoneal liposarcoma with a maximum diameter of 37 cm: a case report and review of literature. Ann Transl Med. 2020;8:1248. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 5. | Mansour S, Azzam N, Kluger Y, Khuri S. Retroperitoneal Liposarcoma: The Giant Type. J Med Cases. 2022;13:517-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 6. | Sun JN, Yang R, Jiang XL, Zhang F, Zhao HW. Giant retroperitoneal liposarcoma with multiple organ involvement: a case report and literature review. BMC Nephrol. 2024;25:281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 7. | Lam-Chung CE, Rodríguez-Orihuela DL, Arízaga-Ramírez R, Almeda-Valdés P, Castillo-Valdez AK, Magaña-Pérez K, Ventura-Gallegos JL, Gamboa-Domínguez A, De Anda González J, Gómez-Pérez FJ, Cuevas-Ramos D. Acromegaly and a Giant Retroperitoneal Liposarcoma Producing IGF-1. AACE Clin Case Rep. 2020;6:e165-e169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 8. | Ayoub M, Leila B, Yassin M, Achraf M, Rachid J, Mohamed PB. Surgical management of giant recurrent retroperitoneal liposarcoma: a case report and review of the literature. Ann Med Surg (Lond). 2023;85:2130-2134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 9. | Lieto E, Cardella F, Erario S, Del Sorbo G, Reginelli A, Galizia G, Urraro F, Panarese I, Auricchio A. Giant retroperitoneal liposarcoma treated with radical conservative surgery: A case report and review of literature. World J Clin Cases. 2022;10:6636-6646. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Nureta TH, Shale WT, Belete TD. Giant retroperitoneal well differentiated liposarcoma: A case report and literature review. Int J Surg Case Rep. 2023;110:108679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 11. | Marjiyeh-Awwad R, Mansour S, Khuri S. Giant Retroperitoneal Liposarcoma: Correlation Between Size and Risk for Recurrence. World J Oncol. 2022;13:244-248. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 12. | Achour Y, Bakali Y, Bahij M, Sekkat H, Mhamdi Alaoui M, Sabbah F, Hrora A, Raiss M. Surgical management of giant retroperitoneal liposarcoma: Case report. Rare Tumors. 2024;16:20363613241266047. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Tani A, Tarumi Y, Kakibuchi A, Aoyama K, Kokabu T, Kataoka H, Yoriki K, Nagamine M, Mori T. Giant retroperitoneal dedifferentiated liposarcoma mimicking ovarian cancer: A case report. Gynecol Oncol Rep. 2022;44:101088. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 14. | Ye MS, Wu HK, Qin XZ, Luo F, Li Z. Hyper-accuracy three-dimensional reconstruction as a tool for better planning of retroperitoneal liposarcoma resection: A case report. World J Clin Cases. 2022;10:268-274. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (1)] |
| 15. | Santangelo A, Fernicola A, Santangelo D, Peluso G, Calogero A, Crocetto F, Jamshidi A, Pelosio L, Scotti A, Tammaro V, Tranquillo V, Tammaro D, De Cocinis C, Della Gaggia F, Capezio E, Carlomagno N, Santangelo M. Dark Topics on Giant Retroperitoneal Liposarcoma: A Systematic Review of 157 Cases. Cancers (Basel). 2025;17:740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Evola G, Schillaci R, Reina M, Caruso G, D'Angelo M, Reina GA. Giant retroperitoneal well-differentiated liposarcoma presenting in emergency with intestinal occlusion: Case report and review of the literature. Int J Surg Case Rep. 2022;95:107152. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 17. | Wei X, Qin Y, Ouyang S, Qian J, Tu S, Yao J. Challenging surgical treatment of giant retroperitoneal liposarcoma: A case report. Oncol Lett. 2022;24:314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 18. | Li Y, Wang X, Yan Y, Du X, Yang X. Giant retroperitoneal liposarcoma: A case report. Asian J Surg. 2022;45:563-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 19. | Kanthala L, Ray S, Aurobindo Prasad Das S, Nundy S, Mehta N. Recurrent giant retroperitoneal liposarcoma: Review of literature and a rare case report. Ann Med Surg (Lond). 2021;65:102329. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 20. | Mori K, Igarashi T, Noguchi A, Ito M, Nagaoka Y, Takeshita C, Takeda N, Watanabe T, Yoshioka I, Hirabayashi K, Fujii T. Giant retroperitoneal myolipoma mimicking liposarcoma: report of a resected case and review of the literature. Int Cancer Conf J. 2024;13:144-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Trajkovski G, Antovic S, Kostovski O, Trajkovska V, Nikolovski A. Giant retroperitoneal low grade liposarcoma with left kidney displacement: A case report. Radiol Case Rep. 2022;17:4091-4095. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 22. | Herrera-Almario G, Cabrera LF, Londoño-Schimmer EE, Pedraza M. Giant retroperitoneal liposarcoma surgical management. Ann R Coll Surg Engl. 2022;104:e54-e56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 23. | Carboni F, Valle M, Federici O, Covello R, Garofalo A. Giant Primary Retroperitoneal Dedifferentiated Liposarcoma. J Gastrointest Surg. 2019;23:1521-1523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 24. | Luo P, Cai W, Yang L, Wu Z, Chen Y, Zhang R, Yan W, Shi Y, Wang C. Retroperitoneal dedifferentiated liposarcoma: Analysis of 61 cases from a large institution. J Cancer. 2018;9:3831-3838. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 25. | Moshref LH. A Successful En Bloc Excision of a Giant Retroperitoneal Liposarcoma With Distal Splenopancreatectomy. Cureus. 2021;13:e18903. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 26. | World Health Organization Classification of Tumours Editorial Board. World Health Organization Classification of Tumours of Soft Tissue and Bone. 5th ed. Lyon: IARC, 2020. |