Published online Aug 16, 2025. doi: 10.12998/wjcc.v13.i23.106532
Revised: April 6, 2025
Accepted: April 24, 2025
Published online: August 16, 2025
Processing time: 96 Days and 11 Hours
Non-operative management (NOM) for uncomplicated acute appendicitis (AA) has been gaining popularity in recent years. One of the major concerns with NOM is the recurrence rate of AA following NOM.
To investigate the impact of the presence of an appendicolith and its specific characteristics on the recurrence rate of AA following NOM.
A retrospective analysis identified all patients treated with NOM for AA, at our institute between 2016 and 2024. Patients with an appendicolith on imaging were identified and their course and outcomes were compared with patients who were treated with NOM without an appendicolith. The primary outcome was defined as a recurrence of AA.
During the study period, 797 patients were treated with NOM for AA. Their mean age was 25.4 years ± 14.4 years, and 45.4% were females. Only 68 patients (8.5%) had an appendicolith identified on imaging. Patients with an appendicolith had a larger appendix diameter (10.2 mm ± 4 mm vs 8.5 mm ± 2.1 mm, P = 0.001). There was no difference in the recurrence rate of patients with and without an appendicolith (26.5% vs 19.1%, P = 0.14), however patients with an appendicolith presented with a shorter time to recurrence of appendicitis (3.9 months ± 10.4 months vs 5.9 months ± 8.1 months, P = 0.04). In a sub analysis, the number of appendicoliths, its size, and its location, did not influence the recurrence rate.
This study demonstrates that patients with appendicoliths have a shorter time to recurrence after NOM of AA, but do not experience higher overall recurrence rates.
Core Tip: This study evaluates the impact of appendicolith presence and characteristics on recurrence after non-operative management (NOM) of acute appendicitis. While appendicoliths do not increase overall recurrence rates, they are associated with a shorter time to recurrence. These findings contribute to risk stratification and may help refine patient selection and follow-up strategies for NOM.
- Citation: Kupietzky A, Bar-Moshe Y, Lavie N, Drayer Lichtman M, Dover R, Juster EY, Maden A, Mazeh H, Mizrahi I. Leaving no stone unturned: Impact of appendicolith and characteristics on long-term recurrence after non-operative appendicitis. World J Clin Cases 2025; 13(23): 106532
- URL: https://www.wjgnet.com/2307-8960/full/v13/i23/106532.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i23.106532
Acute appendicitis (AA) has been traditionally treated surgically with an appendectomy. Recent evidence suggests that uncomplicated AA can be managed effectively with non-operative management (NOM). However, a major concern with NOM for AA is the recurrence rate, which has been reported to range from 5% to 39%[1-3].
AA is caused by luminal obstruction, leading to increased intraluminal pressure, compromising blood flow, causing inflammation, bacterial overgrowth, necrosis, and infection, which in turn can lead to perforation. An appendicolith, a calcified deposit within the appendix, is thought to be the cause of this specific pathophysiological process in 10%-30% of AA cases[4,5]. An appendicolith can be identified radiologically via ultrasound (US) or computed tomography (CT) scans. On ultrasound, it appears as a highly echogenic, round or oval focus with posterior acoustic shadowing, while on CT, it is seen as a high-density, calcified structure within the lumen of the appendix[6]. Appendicolith vary in number, size, and location within the appendix.
Recently, the Comparing Outcomes of Antibiotic Drugs and Appendectomy (CODA) trial found that the presence of an appendicolith in patients with appendicitis who were treated with NOM, is associated with higher rates of compli
Our institutions' protocol for the treatment of acute uncomplicated appendicitis has been previously published[11]. Based on the studies mentioned above, patients with AA who presented with an appendicolith were offered surgery to avoid the reported complications and recurrence rates. However, in real life, patients often refused surgery despite having appendicolith on imaging, and were therefore treated with NOM.
This study aimed to investigate the impact of the presence of an appendicolith and its specific characteristics such as number, size, and location within the appendix on the recurrence rate of AA following NOM.
Following the approval of the institutional review board, a retrospective analysis was conducted to identify all consecutive patients who presented to our emergency department between March 2016 and March 2024 with a diagnosis of AA. Patients of all ages with a diagnosis of AA confirmed by ultrasound, computed tomography, or both, without evidence of an abscess or phlegmon on imaging, and who were selected for NOM, were included in the analysis. The Institutional Review Board waived the requirement for informed consent.
Our institutions' protocol for the treatment of acute uncomplicated appendicitis has been previously published[11]. After diagnosing uncomplicated AA based on clinical presentation and radiological findings, patients are offered either laparoscopic appendectomy or NOM. Up until March 2021, our institutional protocol advised patients with any of the following criteria to undergo a laparoscopic appendectomy: (1) Pain lasting more than 3 days; (2) Fever upon admission; (3) Pregnancy; (4) White blood cell (WBC) count greater than 15 × 109/L; (5) C-reactive protein (CRP) level greater than 5 mg/dL; (6) Appendix diameter greater than 1 cm; (7) Presence of an appendicolith on imaging; (8) Prior episode of AA; and (9) Evidence of peritonitis on physical examination. However, patients who refused surgery despite meeting these criteria including patients with appendicoliths on imaging, were treated with NOM.
Our NOM protocol for uncomplicated appendicitis included the administration of intravenous cefuroxime and metronidazole, with a minimum inpatient follow-up of 24 hours. All patients began with a bowel rest of 12 hours with intravenous fluid support, followed by gradual enteral feeding to ensure adequate intake prior to discharge. The patient's clinical condition was evaluated twice daily by the attending surgeon. Patients who did not improve under NOM underwent laparoscopic appendectomy. Those who responded well to antibiotic therapy and achieved adequate enteral intake were discharged with oral antibiotic therapy to complete a total of 10 days of treatment. All patients were in
Patients’ records were reviewed for demographic variables as well as baseline clinical characteristics including comor
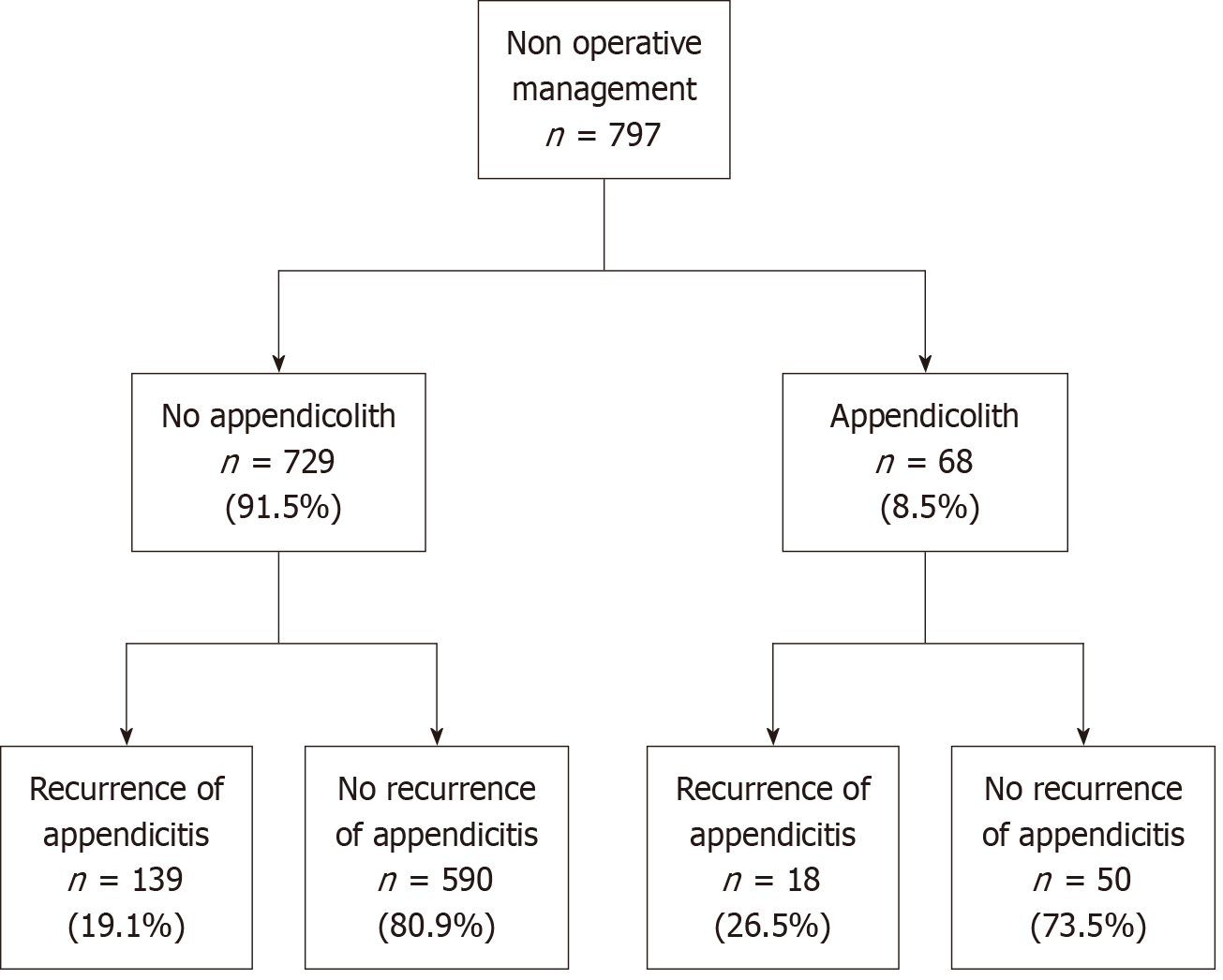
The study group included all patients with radiological evidence of an appendicolith [appendicolith group (AG)] who were treated with NOM for uncomplicated AA. This cohort was compared to a cohort of patients without radiological evidence of an appendicolith (non-AG) who were treated with NOM for uncomplicated AA (Figure 1).
The primary outcome measured was the recurrence rate of AA following NOM. A secondary analysis was performed to detect specific features such as the number of appendicoliths, size, and location within the appendix which might influence recurrence rates of AA.
To identify differences between the study groups, univariate analysis was performed using a χ² or Fisher’s exact test for ordinal or categorical variables. For continuous variables, distribution normality was evaluated using the Shapiroe Wilk test, and either the Manne Whitney U test or the Student’s t-test were used appropriately. Statistical calculations were performed using Statistical Package for the Social Sciences (version 25; SPSS, Inc). A P value of 0.05 or less was considered statistically significant for all comparisons. Data were described using medians with interquartile ranges (IQRs) for discrete data, means for continuous variables and counts with percentages for categorical variables.
During the study period, 797 patients with uncomplicated AA were treated with NOM. The median age was 25.4 years ± 14.4 years, and 45.4% were females. Among the entire cohort, 157 patients (19.8%) experienced recurrent AA during a mean follow-up period of 44.2 (IQRs = 31.9-63.1) months. The study group: Patients with an appendicolith on imaging (AG group) included 68 patients (8.5%), with a median age of 25.3 years ± 14.4 years and 42.7% were females. The study group was compared to patients with no appendicolith on imaging (non-AG) which consisted of the remaining 729 patients. This group had a median age of 25.4 years ± 14.4 years and 45.8% were females.
The two groups were comparable in terms of age, gender, incidence of fever at home, and temperature upon admission. Additionally, inflammatory markers (CRP and WBC) upon admission were similar between the groups. The imaging modalities used for diagnosis were also comparable, with similar rates of ultrasound and CT scans performed.
There was no difference in the recurrence rate of patients with and without an appendicolith (26.5% vs 19.1%, P = 0.14). However, patients with an appendicolith presented with a shorter time to recurrence of appendicitis (3.9 months ± 10.4 months vs 5.9 months ± 8.1 months, P = 0.04). When analyzing the radiological findings, the appendix diameter was significantly larger in the AG group (10.2 mm ± 4 mm vs 8.5 mm ± 2.2 mm, P = 0.001). The LOS was similar between both groups (2.6 days ± 1.5 days vs 2.8 days ± 2 days, P = 0.43). Table 1 summarizes the comparison of demographics and clinical data, between the groups.
| Variable | Total (n = 797) | No appendicolith (non-AG) (n = 729) | Appendicolith (AG) (n = 68) | P value | |
| Gender | Female | 362 (45.4) | 333 (45.8) | 29 (42.7) | 0.62 |
| Male | 434 (54.6) | 395 (54.3) | 39 (57.3) | ||
| Age (years) mean ± SD | 25.4 ± 14.4 | 25.5 ± 14.4 | 25.3 ± 14.4 | 0.94 | |
| Length of pain prior to admission (hours), mean ± SD | 39.3 ± 61.5 | 38.8 ± 62.3 | 44.2 ± 52.3 | 0.94 | |
| Fever at home | 85 (10.6) | 79 (10.9) | 6 (8.8) | 0.75 | |
| Temperature at admission (celsius), mean ± SD | 36.7 ± 0.6 | 36.7 ± 0.6 | 36.8 ± 0.7 | 0.94 | |
| Heart rate on admission, mean ± SD | 89.0 ± 19.5 | 89.1 ± 19.5 | 87.9 ± 18.8 | 0.62 | |
| White blood count (× 109/L), mean ± SD | 11.4 ± 3.9 | 11.4 ± 3.9 | 11.8 ± 4.5 | 0.62 | |
| C-reactive protein (mg/dL), mean ± SD | 3.3 ± 5.4 | 3.2 ± 5.2 | 3.7 ± 6.9 | 0.62 | |
| Ultrasound performed | 462 (58.0) | 422 (58.1) | 40 (58.8) | 0.88 | |
| Computed tomography performed | 460 (57.7) | 419 (57.6) | 41 (60.3) | 0.65 | |
| Radiological findings | Largest appendix diameter (mm), mean ± SD | 8.7 ± 2.4 | 8.5 ± 2.2 | 10.2 ± 1.4 | 0.001 |
| Free fluid on imaging | 229 (28.7) | 203 (27.9) | 26 (38.2) | 0.08 | |
| Length of stay, median (IQR), day | 2.6 (2-3) | 2.6 (2-3) | 2.8 (1-3) | 0.43 | |
| Recurrence of appendicitis | 158 (19.8) | 139 (19.1) | 18 (26.5) | 0.14 | |
| Time to recurrence (months), mean ± SD | 5.7 ± 8.3 | 5.9 ± 8.1 | 3.9 ± 10.4 | 0.04 | |
| Pathology at readmission | Normal appendix | 11 (1.4) | 10 (1.4) | 1 (1.5) | 0.01 |
| Inflamed | 126 (15.8) | 117 (16.1) | 9 (13.2) | ||
| Perforated | 10 (1.3) | 6 (0.8) | 4 (5.9) | ||
| Neoplasia | 5 (0.6) | 4 (0.5) | 1 (1.5) | ||
| Follow up, median (IQR), months | 44.2 (31.9-63.1) | 46.2 (32.1-65.0) | 35.8 (24.0-53.4) | 0.001 |
Of the entire cohort, 68 (8.5%) patients presented with an appendicolith, of whom 18 (26.5%) experienced a recurrence of AA. A focused analysis of appendicolith characteristics revealed that most patients (77.9%) had a single appendicolith, 20.6% had two appendicoliths, and a single patient (1.5%) had three appendicoliths. The locations of the appendicolith were equally distributed throughout the three thirds of the appendix, with 32.3% in the proximal third, 23.5% in the mid-third, and 36.9% in the distal third. When comparing these features between the subgroup of patients who experienced a recurrence and those who did not, none of the factors, including the size of the appendicolith, were found to be associated with recurrence (Table 2).
| Variable | Total (n = 68) | Non-recurrence (n = 50) | Recurrence (n = 18) | P value | |
| Number of appendicolith | 1 | 53 (77.9) | 41 (82) | 12 (66.7) | 0.18 |
| 2 | 14 (20.6) | 8 (16) | 6 (33.3) | ||
| 3 | 1 (1.5) | 1 (2) | 0 (0) | ||
| Appendicolith location | Proximal third | 22 (32.4) | 18 (36) | 4 (22.2) | 0.69 |
| Mid third | 16 (23.5) | 10 (20) | 6 (33.3) | ||
| Distal third | 25 (36.9) | 18 (36) | 7 (38.9) | ||
| Second appendicolith location | Proximal | 4 (5.9) | 3 (6) | 1 (5.6) | 0.80 |
| Mid | 5 (7.4) | 2 (4) | 3 (16.7) | ||
| Distal | 5 (7.4) | 3 (6) | 2 (11.1) | ||
| Appendicolith size (mm) | Length | 7.1 ± 3.7 | 7.3 ± 3.9 | 6.6 ± 3.1 | 0.68 |
| Width | 4.2 ± 2.4 | 4.3 ± 2.7 | 3.7 ± 1.2 | 0.93 | |
| Length to size ratio | 1.8 ± 0.4 | 1.8 ± 0.6 | 1.8 ± 0.8 | 0.52 | |
| Second appendicolith size length (mm) | 4.7 ± 1.8 | 5.5 ± 1.7 | 3.6 ± 1.4 | 0.02 | |
| Second sppendicolith size wide (mm) | 2.8 ± 0.9 | 3.1 ± 1 | 2.4 ± 0.8 | 0.36 | |
| Largest diameter of appendix on imaging modality (mm) | 10.2 ± 1.4 | 10.2 ± 1.2 | 10.3 ± 1.5 | 0.64 |
Additional analysis was conducted to compare clinical characteristics and outcomes between patients who presented with recurrence (n = 157, 19.7%) and between patients who did not (n = 640, 80.3%). The groups were found to be comparable in terms of age, gender, incidence of fever at home, and temperature upon admission. The WBC count and CRP at presentation were similar between the groups as well. The imaging modalities used for diagnosis were com
| Variable | Total (n = 797) | No recurrence (n = 640) | Recurrence (n = 157) | P value | |
| Gender | Female | 362 (45.4) | 290 (45.4) | 72 (45.6) | 0.91 |
| Male | 434 (54.5) | 349 (54.6) | 85 (53.8) | ||
| Age (years) mean ± SD | 25.4 ± 14.4 | 25.5 ± 13.7 | 25.4 ± 14.6 | 0.96 | |
| Length of pain prior to admission (hours), mean ± SD | 39.3 ± 61.5 | 38.8 ± 59.0 | 41 ± 70.6 | 0.70 | |
| Fever at home | 79 (9.9) | 68 (10.6) | 11 (7.0) | 0.17 | |
| Temperature at admission (Celsius), mean ± SD | 36.7 ± 0.6 | 36.7 ± 0.6 | 36.7 ± 0.5 | 0.77 | |
| Heart rate on admission, mean ± SD | 89.0 ± 19.5 | 88.2 ± 18.0 | 89.2 ± 19.8 | 0.59 | |
| White blood count (× 109/L), mean ± SD | 11.4 ± 3.9 | 11.3 ± 3.9 | 11.8 ± 4.0 | 0.14 | |
| C-reactive protein (mg/dL), mean ± SD | 3.3 ± 5.3 | 3.2 ± 5.3 | 3.5 ± 5.7 | 0.60 | |
| Ultrasound performed | 462 (58.0) | 379 (59.3) | 83 (52.5) | 0.12 | |
| Computed tomography performed | 460 (57.7) | 367 (57.4) | 93 (59.0) | 0.75 | |
| Appendicolith | 68 (8.5) | 50 (7.8) | 18 (11.5) | 0.08 | |
| Radiological findings | Largest appendix diameter (mm), mean ± SD | 8.7 ± 2.4 | 8.6 ± 2.4 | 9.1 ± 2.6 | 0.03 |
| Free fluid on imaging | 229 (28.7) | 178 (27.9) | 51 (32.3) | 0.32 | |
| Length of stay, median (interquartile ranges) (day) | 2.6 (2-3) | 2.6 (2-3) | 2.7 (2-3) | 0.53 |
This investigation involved 797 patients with uncomplicated AA who were treated with NOM. The study aimed to analyze the impact of an appendicolith and its characteristics on the recurrence rate specifically in patients with uncomplicated AA. The findings show that there was no difference in the recurrence rate of patients with and without an appendicolith (P = 0.14). However, patients with an appendicolith presented with a shorter time to recurrence (P = 0.04). Additionally, specific characteristics of the appendicolith, including the number, location, and size, did not predict recurrence.
Previous studies have shown that an appendicolith, the calcified deposit within the appendix, is associated with a higher risk of complicated appendicitis and a higher rate of failure of NOM for AA[12-15]. In a recent Finnish analysis by Mällinen et al[16], the histopathological features of patients with CT-verified AA presenting with an appendicolith were compared with those of patients with uncomplicated AA enrolled in the surgical treatment arm of the randomized Appendicitis Acuta trial. Statistically significant differences were detected, with an appendicolith correlating with a more severe histopathological inflammatory process. This analysis underscores that the presence of an appendicolith is associated with a worse inflammatory response. However, the studies mentioned above included in their analysis patients with complicated and uncomplicated AA. In our analysis, we purposely included only patients with uncompli
In 2020, the large multi-center, randomized CODA trial conducted in the United States published their results[7]. In their analysis, the authors randomized a total of 1552 adults, of which 414 had an appendicolith, to receive either antibiotics (776 patients) or an appendectomy (776 patients). This randomized clinical study aimed to determine whether antibiotics are as effective as surgery (appendectomy) for treating AA. They found that in the antibiotics group, 29% had undergone appendectomy by 90 days, including 41% of those with an appendicolith and 25% of those without an appendicolith. They concluded that participants with an appendicolith were at a higher risk for appendectomy and complications than those without an appendicolith. In 2021, the CODA trial group published a follow-up paper updating their longer-term outcomes, including the risk of recurrence of appendicitis and the rate of eventual appendectomy among patients who were assigned to receive antibiotic therapy[18]. They found that appendectomy was more common among patients who had an appendicolith, but the risk decreased over time and was almost negligible after 30 days (hazard ratio for appendectomy among patients with an appendicolith compared with those without an appendicolith was 1.1; 95%CI: 0.8-1.6, from 31 days to 2 years). Even though the results of this well-conducted large trial shed light on the impact of appendicoliths on NOM for AA, the trial was not strictly limited to uncomplicated AA. In fact, it included more severe cases of appendicitis, with 16% of patients in the surgery group presenting with a perforation upon appendectomy.
While the CODA trial provided substantial evidence, it highlighted the need for more granular analyses regarding the characteristics of appendicoliths and their precise impact on treatment outcomes. In a recent publication, Kubota et al[19] retrospectively reviewed records of 479 consecutive patients with AA. Appendicoliths were identified in 214 patients (44.6%). NOM was initially selected for 158 patients and was successful in 128 patients (81%), of whom 36 patients had an appendicolith. Of the 30 patients who failed NOM, 10 patients had an appendicolith. They found that patients with appendicoliths who completed the medication regimen had smaller stones (P < 0.001) and concluded that patients with an appendicolith measuring less than 5 mm were appropriate candidates for NOM. The authors did not address the location or number of appendicoliths, nor did they discuss the recurrence rate. The present study included a long-term follow up [mean 44.2 (31.9-63.1) months] and demonstrated no difference in recurrence rates of patients with and without appendicoliths. Furthermore, in a subgroup analysis, the number, size, and location of appendicoliths did not influence the recurrence rate.
A recent investigation by Lie et al[8], aimed to identify predictors for recurrent appendicitis in patients who were previously treated non-operatively. Their cohort included 74 patients with complicated or uncomplicated disease who were treated non-operatively. Twenty-one patients (29%) in their cohort experienced recurrent appendicitis. On univa
The Jerusalem guidelines from the World Society of Emergency Surgery advise against NOM of AA in the presence of an appendicolith because of its higher failure rate, quoting a failure rate as high as 60% at a median follow-up of less than 5 months[20]. This recommendation is based on small studies, which have included cases of uncomplicated appendicitis alongside patients with complicated appendicitis, perforated appendicitis and peri-appendicular abscess, in their NOM protocols. In our research we deliberately included only patients with uncomplicated AA and an appendicolith, to try and isolate the impact of the appendicolith on clinical outcomes. Our results indicate that the presence of an appendi
This study has several limitations. First, it is a retrospective analysis conducted at a single institution, which subjects it to biases including selection bias, reporting bias, and data collection bias. Second, the patients in the study were managed by multiple surgeons, who may have introduced variability in management, including patients’ selection for NOM, and clinical judgment throughout the admission, which might also affect the findings. Third, the AG had a significantly shorter follow-up period, potentially underestimating the true long-term recurrence rate. However, our data also indicates that most recurrences occur within the first year after NOM, suggesting that our follow-up timeframe for both cohorts captures essentially all clinically relevant recurrences. Nonetheless, future prospective studies with standardized, long-term follow-up are needed to further clarify the recurrence risk in patients with appendicoliths undergoing NOM. Despite these limitations, our investigation is exceptional as it includes the largest cohort of patients presenting with uncomplicated AA and an appendicolith with a long-term follow-up period and is the first to explore specific characteristics of appendicoliths. This study is an outcome of an expanding pool of patients with uncomplicated AA who elect NOM despite having an appendicolith on their imaging studies. We believe the results contribute to the growing knowledge on the risk-benefit ratio of NOM for acute uncomplicated appendicitis. Furthermore, the study provides healthcare providers with in-depth knowledge to guide patients in making this shared treatment decision.
This study demonstrated that, within the available follow-up period, there is no difference in recurrence rates of patients presenting with uncomplicated AA with and without an appendicolith. While the shorter follow-up in the appendicolith group warrants caution in interpreting long-term recurrence rates, our findings suggest that most recurrences occur within the first year. We believe that the presence of an appendicolith should be factored into the decision-making process when considering NOM vs surgery. Nevertheless, it should not be regarded as a definitive contraindication for NOM. In carefully selected patients, NOM remains a safe and effective alternative to surgery, even in the presence of an appendicolith.
| 1. | Salminen P, Tuominen R, Paajanen H, Rautio T, Nordström P, Aarnio M, Rantanen T, Hurme S, Mecklin JP, Sand J, Virtanen J, Jartti A, Grönroos JM. Five-Year Follow-up of Antibiotic Therapy for Uncomplicated Acute Appendicitis in the APPAC Randomized Clinical Trial. JAMA. 2018;320:1259-1265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 315] [Article Influence: 45.0] [Reference Citation Analysis (2)] |
| 2. | de Almeida Leite RM, Seo DJ, Gomez-Eslava B, Hossain S, Lesegretain A, de Souza AV, Bay CP, Zilberstein B, Marchi E, Machado RB, Barchi LC, Ricciardi R. Nonoperative vs Operative Management of Uncomplicated Acute Appendicitis: A Systematic Review and Meta-analysis. JAMA Surg. 2022;157:828-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 55] [Article Influence: 18.3] [Reference Citation Analysis (102)] |
| 3. | Emile SH, Sakr A, Shalaby M, Elfeki H. Efficacy and Safety of Non-Operative Management of Uncomplicated Acute Appendicitis Compared to Appendectomy: An Umbrella Review of Systematic Reviews and Meta-Analyses. World J Surg. 2022;46:1022-1038. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 4. | Engin O, Muratli A, Ucar AD, Tekin V, Calik B, Tosun A. The importance of fecaliths in the aetiology of acute appendicitis. Chirurgia (Bucur). 2012;107:756-760. [PubMed] |
| 5. | Ramdass MJ, Young Sing Q, Milne D, Mooteeram J, Barrow S. Association between the appendix and the fecalith in adults. Can J Surg. 2015;58:10-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 6. | Babington EA. Appendicoliths, the little giants: A narrative review. Radiography (Lond). 2023;29:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 7. | CODA Collaborative, Flum DR, Davidson GH, Monsell SE, Shapiro NI, Odom SR, Sanchez SE, Drake FT, Fischkoff K, Johnson J, Patton JH, Evans H, Cuschieri J, Sabbatini AK, Faine BA, Skeete DA, Liang MK, Sohn V, McGrane K, Kutcher ME, Chung B, Carter DW, Ayoung-Chee P, Chiang W, Rushing A, Steinberg S, Foster CS, Schaetzel SM, Price TP, Mandell KA, Ferrigno L, Salzberg M, DeUgarte DA, Kaji AH, Moran GJ, Saltzman D, Alam HB, Park PK, Kao LS, Thompson CM, Self WH, Yu JT, Wiebusch A, Winchell RJ, Clark S, Krishnadasan A, Fannon E, Lavallee DC, Comstock BA, Bizzell B, Heagerty PJ, Kessler LG, Talan DA. A Randomized Trial Comparing Antibiotics with Appendectomy for Appendicitis. N Engl J Med. 2020;383:1907-1919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 332] [Article Influence: 66.4] [Reference Citation Analysis (0)] |
| 8. | Lie JJ, Nabata K, Zhang JW, Zhao D, Park CM, Hameed SM, Dawe P, Hamilton TD. Factors associated with recurrent appendicitis after nonoperative management. Am J Surg. 2023;225:915-920. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Flum DR; writing group for the CODA Collaborative. Factors associated with recurrent appendicitis after successful treatment with antibiotics. Br J Surg. 2023;110:1482-1489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Scott A, Lee SL, DeUgarte DA, Shew SB, Dunn JCY, Shekherdimian S. Nonoperative Management of Appendicitis. Clin Pediatr (Phila). 2018;57:200-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Shay S, Kupietzky A, Weiss DJ, Dover R, Lourie NEE, Mordechay-Heyn T, Mazeh H, Mizrahi I. Composite Criteria for Non-Operative Management of Acute Non-Complicated Appendicitis Result in Low Failure Rates. World J Surg. 2022;46:69-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Sakran JV, Mylonas KS, Gryparis A, Stawicki SP, Burns CJ, Matar MM, Economopoulos KP. Operation versus antibiotics--The "appendicitis conundrum" continues: A meta-analysis. J Trauma Acute Care Surg. 2017;82:1129-1137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 13. | Mahida JB, Lodwick DL, Nacion KM, Sulkowski JP, Leonhart KL, Cooper JN, Ambeba EJ, Deans KJ, Minneci PC. High failure rate of nonoperative management of acute appendicitis with an appendicolith in children. J Pediatr Surg. 2016;51:908-911. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 75] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 14. | Huang L, Yin Y, Yang L, Wang C, Li Y, Zhou Z. Comparison of Antibiotic Therapy and Appendectomy for Acute Uncomplicated Appendicitis in Children: A Meta-analysis. JAMA Pediatr. 2017;171:426-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 159] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 15. | Kaewlai R, Wongveerasin P, Lekanamongkol W, Wongsaengchan D, Teerasamit W, Tongsai S, Khamman P, Chatkaewpaisal A, Noppakunsomboon N, Apisarnthanarak P. CT of appendicoliths in adult appendicitis: clinical significance and characteristics of overlooked cases. Eur Radiol. 2024;34:2534-2545. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Mällinen J, Vaarala S, Mäkinen M, Lietzén E, Grönroos J, Ohtonen P, Rautio T, Salminen P. Appendicolith appendicitis is clinically complicated acute appendicitis-is it histopathologically different from uncomplicated acute appendicitis. Int J Colorectal Dis. 2019;34:1393-1400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 42] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 17. | Lee MS, Purcell R, McCombie A, Frizelle F, Eglinton T. Retrospective cohort study of the impact of faecoliths on the natural history of acute appendicitis. World J Emerg Surg. 2023;18:18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 18. | CODA Collaborative, Davidson GH, Flum DR, Monsell SE, Kao LS, Voldal EC, Heagerty PJ, Fannon E, Lavallee DC, Bizzell B, Lawrence SO, Comstock BA, Krishnadasan A, Winchell RJ, Self WH, Thompson CM, Farjah F, Park PK, Alam HB, Saltzman D, Moran GJ, Kaji AH, DeUgarte DA, Salzberg M, Ferrigno L, Mandell KA, Price TP, Siparsky N, Glaser J, Ayoung-Chee P, Chiang W, Victory J, Chung B, Carter DW, Kutcher ME, Jones A, Holihan J, Liang MK, Faine BA, Cuschieri J, Evans HL, Johnson J, Patton JH, Coleman N, Fischkoff K, Drake FT, Sanchez SE, Parsons C, Odom SR, Kessler LG, Talan DA. Antibiotics versus Appendectomy for Acute Appendicitis - Longer-Term Outcomes. N Engl J Med. 2021;385:2395-2397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 44] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 19. | Kubota A, Yokoyama N, Sato D, Hashidate H, Nojiri S, Taguchi C, Otani T. Treatment for Appendicitis With Appendicolith by the Stone Size and Serum C-Reactive Protein Level. J Surg Res. 2022;280:179-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 20. | Di Saverio S, Podda M, De Simone B, Ceresoli M, Augustin G, Gori A, Boermeester M, Sartelli M, Coccolini F, Tarasconi A, De' Angelis N, Weber DG, Tolonen M, Birindelli A, Biffl W, Moore EE, Kelly M, Soreide K, Kashuk J, Ten Broek R, Gomes CA, Sugrue M, Davies RJ, Damaskos D, Leppäniemi A, Kirkpatrick A, Peitzman AB, Fraga GP, Maier RV, Coimbra R, Chiarugi M, Sganga G, Pisanu A, De' Angelis GL, Tan E, Van Goor H, Pata F, Di Carlo I, Chiara O, Litvin A, Campanile FC, Sakakushev B, Tomadze G, Demetrashvili Z, Latifi R, Abu-Zidan F, Romeo O, Segovia-Lohse H, Baiocchi G, Costa D, Rizoli S, Balogh ZJ, Bendinelli C, Scalea T, Ivatury R, Velmahos G, Andersson R, Kluger Y, Ansaloni L, Catena F. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020;15:27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 697] [Cited by in RCA: 601] [Article Influence: 120.2] [Reference Citation Analysis (109)] |