Published online Aug 16, 2025. doi: 10.12998/wjcc.v13.i23.106329
Revised: March 30, 2025
Accepted: April 25, 2025
Published online: August 16, 2025
Processing time: 102 Days and 4.7 Hours
Middle meningeal artery embolization (MMAE) is emerging as a promising treatment for chronic subdural hematoma (CSDH), serving both as an adjunct to surgery and as a primary therapeutic option depending on patient presentation. Due to its low recurrence rate and minimal complications, MMAE has gained increasing acceptance among clinicians in recent years. This report presents a case of diplopia following MMAE due to the presence of a potential anastomotic artery, aiming to enhance awareness of this complication.
A 60-year-old male patient presented with a headache following head trauma, and cranial computed tomography revealed a left-sided CSDH. The patient underwent left MMAE; however, polyvinyl alcohol particles inadvertently flowed into the lacrimal artery through an anastomotic artery, resulting in diplopia due to impaired abduction of the left eye. The diplopia resolved by postoperative day 40. The patient’s headache resolved by postoperative day 7, and the hematoma completely resolved by postoperative day 108.
Potential anastomotic arteries in the middle meningeal artery (MMA) can lead to serious complications. Superselective angiography of the MMA or its branches prior to embolization is essential. Performing embolization distal to potential anastomotic sites can reduce risks, and the presence of an anastomosis may warrant coil embolization or termination of the procedure.
Core Tip: Middle meningeal artery embolization is emerging as a potential treatment for chronic subdural hematoma. However, the presence of anastomotic arteries in the middle meningeal artery can complicate the procedure, potentially leading to severe complications if not identified preoperatively.
- Citation: Zhao F, Su CH, Hu SX, Feng L. Diplopia after middle meningeal artery embolization for chronic subdural hematoma: A case report. World J Clin Cases 2025; 13(23): 106329
- URL: https://www.wjgnet.com/2307-8960/full/v13/i23/106329.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i23.106329
Chronic subdural hematoma (CSDH) is a common neurosurgical condition characterized by headache and limb weakness due to hemorrhage accumulation beneath the dura mater, exerting pressure on brain tissue. Traditional surgical treatments are associated with high recurrence rates. In recent years, middle meningeal artery embolization (MMAE) has gained traction due to its lower recurrence rates and fewer complications.
We present a case of diplopia following MMAE for CSDH. Informed consent was obtained from the patient, and the ethics committee waived approval for this report. To our knowledge, this is the first study to provide detailed insights into the development of diplopia after MMAE for CSDH. Shotar et al[1] reported two cases of transient diplopia associated with abducens nerve palsy following MMAE, while Raviskanthan et al[2] documented a case of bilateral abducens nerve palsies after bilateral MMAE. However, neither study thoroughly elucidated the underlying mechanisms. This case report details a patient with a clear risk of anastomosis, as demonstrated by imaging.
A 67-year-old male presented with a mild traumatic brain injury and a progressively worsening headache over 40 days.
The patient sustained a head injury from a bicycle accident 40 days prior. One week before admission, he developed a headache that gradually worsened, accompanied by nausea and vomiting one day prior. Cranial computed tomography (CT) revealed a left-sided chronic subdural hematoma.
The patient underwent lumbar spine surgery 10 years ago and had a history of alcohol consumption and smoking for over 40 years.
No significant personal or family medical history.
The patient’s temperature was 36.3 °C, heart rate was 70 beats per minute, and blood pressure was 164/108 mmHg. No significant abnormalities were noted on physical examination.
No abnormalities were detected in laboratory tests.
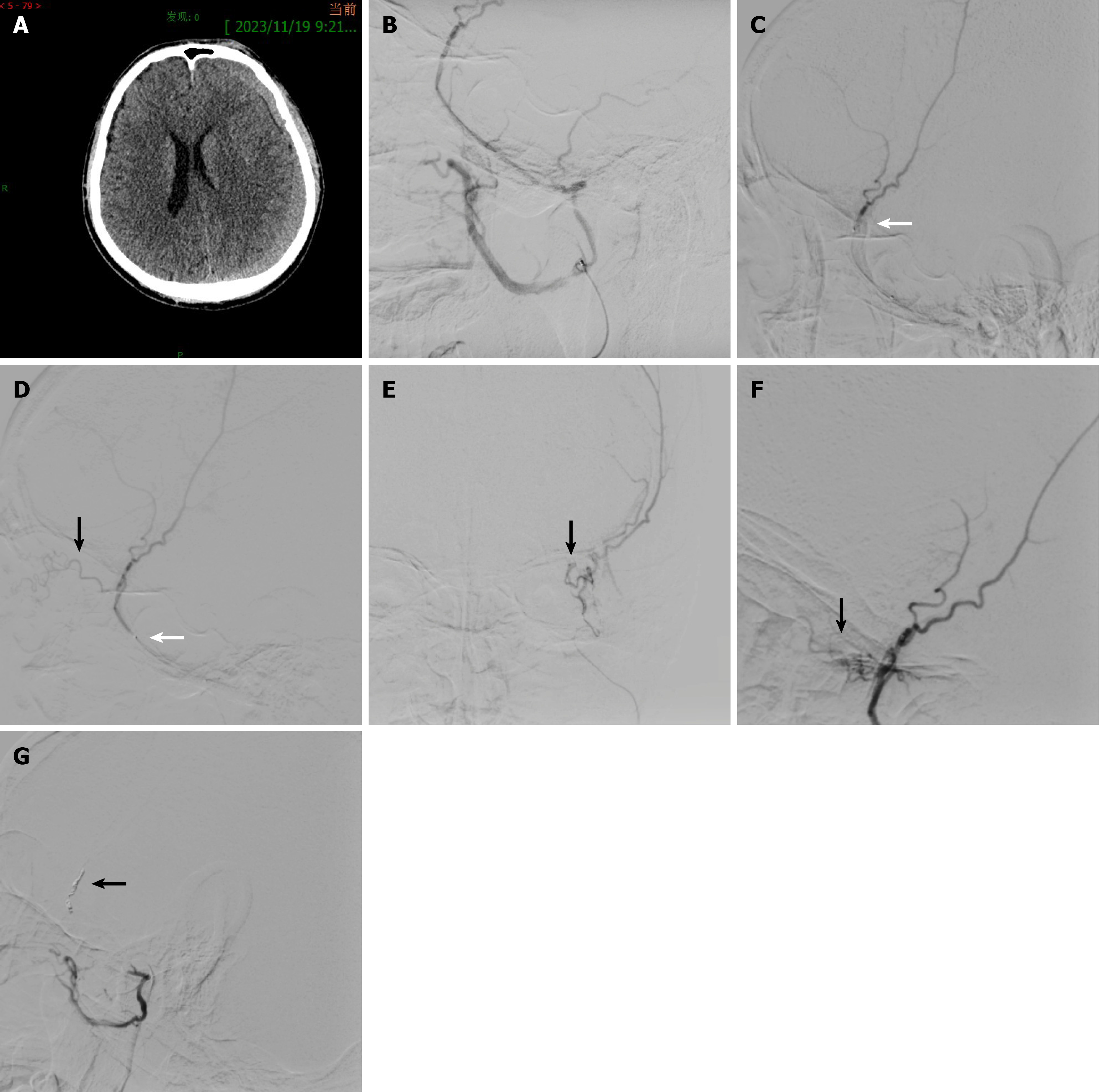
Cranial CT revealed a left-sided chronic subdural hematoma (Figure 1A), with midline shift of 5 mm to the right and a maximum hematoma thickness of 13 mm.
The patient was diagnosed with left-sided traumatic chronic subdural hematoma based on clinical history and imaging findings.
Given the favorable clinical condition and moderate hematoma volume, the patient underwent left MMAE under local anesthesia. Angiography of the left common carotid artery revealed that the ophthalmic artery originated from the internal carotid artery, while the middle meningeal artery (MMA) arose from the internal maxillary artery (Figure 1B). Pre-embolization three-dimensional angiography showed no definitive anastomotic artery between the internal and external carotid arteries. A microcatheter (Echelon-10; ev3 Neurovascular, Irvine, CA, United States) was advanced into the anterior branch of the MMA, and polyvinyl alcohol (PVA) particles (150–350 μm; Hangzhou Alicon Pharm SCI & TEC CO., LTD., China) were injected (Figure 1C). During PVA injection, patient movement caused the microcatheter tip to retract, revealing an anastomotic artery from the MMA to the orbit (Figure 1D and E). The microcatheter was repositioned above the anastomotic artery, but PVA refluxed into the anastomotic artery again (Figure 1F). Three coils were then deployed in the MMA near the anastomotic artery, followed by PVA embolization of the posterior branch until complete occlusion of the anterior and posterior branches was achieved (Figure 1G).
The patient developed diplopia immediately postoperatively, with impaired abduction of the left eye. No blindness, blurred vision, or facial sensory deficits were noted. The patient was treated with oral methylcobalamin (0.5 mg three times daily) combined with ocular motility rehabilitation training. Complete resolution of diplopia was achieved after 40 days of this therapeutic regimen. The headache resolved by postoperative day 7, and the hematoma completely resolved by postoperative day 108.
CSDH is one of the most common central nervous system disorders, with an annual incidence of 2–20 per 100000 individuals[3,4]. Its prevalence is increasing due to aging populations and the widespread use of antithrombotic agents[5]. Surgical evacuation, through burr-hole drainage or open craniotomy, and supportive medical care are the standard treatments for symptomatic chronic subdural hematoma[6]. But traditional treatments are associated with recurrence rates of 9%–33%[7]. In recent years, MMAE has emerged as a promising treatment for CSDH, targeting the middle meningeal artery (MMA), which plays a critical role in CSDH pathogenesis. This treatment has been proposed as a primary therapy, an adjunct to surgical drainage, and for recurrent CSDH [8-12]. However, the presence of anastomotic arteries poses significant risks during MMAE.
A feared complication of MMAE is the inadvertent embolization of the ophthalmic artery or facial nerve artery through anastomotic channels, potentially leading to blindness or facial paralysis[13-16]. Two anastomotic pathways exist: A short, straight meningolacrimal artery traversing the foramen of Hyrtl and a long, tortuous sphenoidal artery passing through the superior orbital fissure. In our patient, intraoperative imaging revealed a long, tortuous anastomotic artery supplying the lacrimal artery, consistent with a type II vascular pattern as classified by Hayreh[17]. We hypothesize that PVA particles embolized the blood supply to the lateral rectus muscle and its abducens nerve, resulting in abductor dysfunction.
This complication underscores the importance of detecting anastomotic arteries prior to embolization. Although pre-embolization angiography of the common carotid artery was performed, the anastomotic artery was not initially visualized. During the procedure, patient movement caused the microcatheter to retract, revealing the anastomotic artery upon PVA reinjection. Despite repositioning the microcatheter, PVA still refluxed into the anastomotic artery. Consequently, we ultimately employed coil embolization as the definitive treatment strategy. Shotar et al[1] reported two cases of transient diplopia secondary to abducens nerve palsy following MMAE. Notably, neither case demonstrated angiographic evidence of anastomoses between the MMA and ophthalmic artery or orbital branches. However, in one patient, the marginal tentorial artery originated from the MMA, which may have contributed to the neurological deficit. While the authors did not provide detailed procedural specifics regarding embolic materials, they suggested that coil embolization or distal selective embolization could mitigate risks associated with such vascular variations. Raviskanthan et al[2] described a case of bilateral abducens nerve palsies following MMAE using 300-500 μm embosphere particles, though the exact mechanism remained unclear. The authors postulated microvascular occlusion by embolic particles as a potential etiology. In contrast, our case provided direct intraprocedural evidence of particle migration into dangerous anastomoses. Although we selected smaller PVA particles (150-350 μm) to achieve more distal MMA branch occlusion, current evidence does not conclusively demonstrate that smaller particles increase the risk of anastomotic penetration. We emphasize that meticulous angiographic identification of potential dangerous anastomoses - particularly through superselective MMA branch catheterization - remains paramount for procedural safety. This case highlights the need to position the microcatheter distal to potential anastomotic sites and to employ segmental catheter withdrawal strategies to minimize reflux. If an anastomotic artery is identified, coil embolization or termination of the procedure should be considered.
Given that the diplopia resulted from compromised vascular supply to the lateral rectus muscle and its abducens nerve due to embolization - a condition with no specific pharmacological treatment - we initiated a therapeutic regimen combining oral methylcobalamin with ocular motor rehabilitation training. The patient achieved complete resolution of diplopia at 40-day follow-up. While spontaneous recovery can occur in partial abducens nerve palsy, the observed clinical improvement suggests methylcobalamin may have provided beneficial neurotrophic support during the recovery process.
Potential anastomotic arteries in the MMA can lead to serious complications. Superselective angiography of the MMA or its branches prior to embolization is essential. Embolization should be performed distal to potential anastomotic sites, and the presence of an anastomosis may warrant coil embolization or termination of the procedure.
| 1. | Shotar E, Premat K, Lenck S, Degos V, Marijon P, Pouvelle A, Pouliquen G, Mouyal S, Abi Jaoude S, Sourour NA, Mathon B, Clarençon F. Angiographic Anatomy of the Middle Meningeal Artery in Relation to Chronic Subdural Hematoma Embolization. Clin Neuroradiol. 2022;32:57-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 2. | Raviskanthan S, Mortensen PW, Zhang YJ, Lee AG. Bilateral Abducens Nerve Palsies After Middle Meningeal Artery Embolization for Chronic Subdural Hematoma. J Neuroophthalmol. 2022;42:e505-e507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Foelholm R, Waltimo O. Epidemiology of chronic subdural haematoma. Acta Neurochir (Wien). 1975;32:247-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 145] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Karibe H, Kameyama M, Kawase M, Hirano T, Kawaguchi T, Tominaga T. [Epidemiology of chronic subdural hematomas]. No Shinkei Geka. 2011;39:1149-1153. [PubMed] |
| 5. | Balser D, Farooq S, Mehmood T, Reyes M, Samadani U. Actual and projected incidence rates for chronic subdural hematomas in United States Veterans Administration and civilian populations. J Neurosurg. 2015;123:1209-1215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 225] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 6. | Liu J, Ni W, Zuo Q, Yang H, Peng Y, Lin Z, Li Z, Wang J, Zhen Y, Luo J, Lin Y, Chen J, Hua X, Lu H, Zhong M, Liu M, Zhang J, Wang Y, Wan J, Li Y, Li T, Mao G, Zhao W, Gao L, Li C, Chen E, Cheng X, Zhang P, Wang Z, Chen L, Zhang Y, Tian B, Shen F, Lei Y, Wu Y, Li Y, Duan G, Xu L, Lv N, Yu J, Xu X, Du Z, Zhang H, Hu J, Li Z, Yuan Q, Zhou Y, Wu G, Zhang L, Gao C, Dai D, Wu X, Zhang Y, Jiang H, Zhao R, Su J, Xu Y, Ospel JM, Majoie CBLM, Goyal M, Li Q, Yang P, Gu Y, Mao Y; MAGIC-MT Investigators. Middle Meningeal Artery Embolization for Nonacute Subdural Hematoma. N Engl J Med. 2024;391:1901-1912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 47] [Article Influence: 47.0] [Reference Citation Analysis (1)] |
| 7. | Takahashi S, Yamauchi T, Yamamura T, Ogishima T, Arai T. Proposal of Treatment Strategies for Bilateral Chronic Subdural Hematoma Based on Laterality of Treated Hematoma. Asian J Neurosurg. 2018;13:1134-1139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Ironside N, Nguyen C, Do Q, Ugiliweneza B, Chen CJ, Sieg EP, James RF, Ding D. Middle meningeal artery embolization for chronic subdural hematoma: a systematic review and meta-analysis. J Neurointerv Surg. 2021;13:951-957. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 135] [Article Influence: 33.8] [Reference Citation Analysis (0)] |
| 9. | Salah WK, Baker C, Scoville JP, Hunsaker JC, Ogilvy CS, Moore JM, Riina HA, Levy EI, Spiotta AM, Jankowitz BT, Michael Cawley C 3rd, Khalessi AA, Tanweer O, Hanel R, Gross BA, Kuybu O, Hoang AN, Baig AA, Khorasanizadeh MH, Mendez AA, Cortez G, Davies JM, Narayanan S, Howard BM, Lang MJ, Siddiqui AH, Thomas A, Kan P, Burkhardt JK, Salem MM, Grandhi R. Middle meningeal artery embolization as a perioperative adjunct to surgical evacuation of nonacute subdural hematomas: An multicenter analysis of safety and efficacy. Interv Neuroradiol. 2023;15910199231162665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 10. | Nia AM, Srinivasan VM, Siddiq F, Thomas A, Burkhardt JK, Lall RR, Kan P. Trends and Outcomes of Primary, Rescue, and Adjunct Middle Meningeal Artery Embolization for Chronic Subdural Hematomas. World Neurosurg. 2022;164:e568-e573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 11. | Ban SP, Hwang G, Byoun HS, Kim T, Lee SU, Bang JS, Han JH, Kim CY, Kwon OK, Oh CW. Middle Meningeal Artery Embolization for Chronic Subdural Hematoma. Radiology. 2018;286:992-999. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 273] [Article Influence: 34.1] [Reference Citation Analysis (0)] |
| 12. | Khorasanizadeh M, Maroufi SF, Mukherjee R, Sankaranarayanan M, Moore JM, Ogilvy CS. Middle Meningeal Artery Embolization in Adjunction to Surgical Evacuation for Treatment of Subdural Hematomas: A Nationwide Comparison of Outcomes With Isolated Surgical Evacuation. Neurosurgery. 2023;93:1082-1089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 19] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 13. | Turner T, Trobe JD, Deveikis JP. Sequential branch retinal artery occlusions following embolization of an intracranial meningioma. Arch Ophthalmol. 2002;120:857-860. [PubMed] |
| 14. | Rosen CL, Ammerman JM, Sekhar LN, Bank WO. Outcome analysis of preoperative embolization in cranial base surgery. Acta Neurochir (Wien). 2002;144:1157-1164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 100] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 15. | Gatto LAM, Saurin F, Koppe GL, Demartini Z Junior. Facial palsy after embolization of dural arteriovenous fistula: A case report and literature review. Surg Neurol Int. 2017;8:270. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Takanami T, Kondo K, Asakage T. Facial paralysis after superselective intra-arterial chemotherapy via the middle meningeal artery in maxillary cancer. Auris Nasus Larynx. 2009;36:479-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Hayreh SS. The ophthalmic artery: III. Branches. Br J Ophthalmol. 1962;46:212-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 182] [Article Influence: 11.4] [Reference Citation Analysis (0)] |