Published online Aug 16, 2025. doi: 10.12998/wjcc.v13.i23.105671
Revised: April 9, 2025
Accepted: May 8, 2025
Published online: August 16, 2025
Processing time: 121 Days and 4.5 Hours
Aortoiliac artery stenting has been accepted as the preferred option for the treatment of aortoiliac artery disease because of lower morbidity and mortality compared with bypass surgery. However, acute stent occlusion is a troublesome complication due to the need for open surgery or the risk of distal embolization. Herein, we reported a novel approach to treat the acute thrombotic occlusion of an aortoiliac stent using both hemolytic and conventional mechanical thrombectomy coupled with a large diameter sheath.
A 64-year-old male patient presented with severe claudication of the right leg. The patient's history included multiple prior interventions for aortoiliac lesions. The preoperative computed tomography (CT) imaging showed a thrombotic occlusion of right aortoiliac stenting. An Angiojet Omni thrombectomy catheter (Boston Scientific, Marlborough, MA, United States) was used to remove the thrombus in a retrograde fashion after the successful placement of the large-diameter sheath in the right common femoral artery for prevention of distal embolization. The remnant organized thrombus was removed with an over-the-wire Fogarty catheter (Edwards Lifesciences, Irvine, CA, United States). Completion angiogram and postoperative CT imaging demonstrated complete removal of thrombus and no evidence of distal embolization.
This novel approach provides successful management of acute thrombotic occlusion of aortoiliac stent without distal embolization.
Core Tip: Acute aortoiliac stent occlusion is a troublesome complication due to the need for open surgery or the risk of distal embolization. After the placement of a large-dimeter sheath in the access site, retrograde application of rheolytic thrombectomy catheter can effectively remove the thrombus. And the conventional mechanical thrombectomy can remove the remnant organized thrombus. During both rheolytic and mechanical thrombectomy, the application of a large-diameter sheath can prevent distal embolization.
- Citation: Cho S, Joh JH. Retrograde approach of Angiojet catheter for the acute occlusion of aortoiliac artery stent: A case report. World J Clin Cases 2025; 13(23): 105671
- URL: https://www.wjgnet.com/2307-8960/full/v13/i23/105671.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i23.105671
Endovascular stent placement has been accepted as the preferred option for the treatment of aortoiliac artery disease because of lower morbidity and mortality when compared with open surgery[1]. With the advancement of endovascular devices and techniques, many studies have reported satisfactory outcomes with stent placement for TASC C and D aortoiliac artery diseases[2,3]. However, stent occlusion is a troublesome complication for this approach. Stent occlusion can occur up to 10% at 1 year and is more common at long-term follow-up[4]. Thrombotic occlusion of iliac artery stent can be more challenging to treat in an endovascular manner due to the high risk of distal embolization.
Angiojet™ thrombectomy system (Boston Scientific, MA, United States) is frequently used to treat the thrombotic lesion of a peripheral artery[5]. Here, we reported a case with thrombotic occlusion of aortoiliac stent using a retrograde approach of an Angiojet thrombectomy catheter and over-the-wire conventional thrombectomy catheter coupled with a large-diameter sheath to prevent distal embolization.
A 64-year-old man presented with severe claudication of the right leg.
Symptoms appeared 6 days before presentation.
The patient had hypertension managed with a single antihypertensive medication. He had multiple interventions for the treatment of aortoiliac lesions. Six years before presentation, the left iliac artery stenting was performed due to the occlusion of the left iliac artery. He underwent another stenting on both iliac arteries due to the progression of lesions two years before the presentation. Aortoiliac kissing stenting was done one year ago due to the proximal progression of lesions.
The patient had no specific family history of peripheral arterial disease.
During the physical examination, the patient’s vital signs were stable. A pulse was not palpable over the right common femoral, popliteal, and pedal arteries.
All blood cell tests were within the normal ranges except for a slightly increased erythrocyte sedimentation rate of 20 mm/h. Ankle brachial index (ABI) was measured as 0.67 on his right leg.
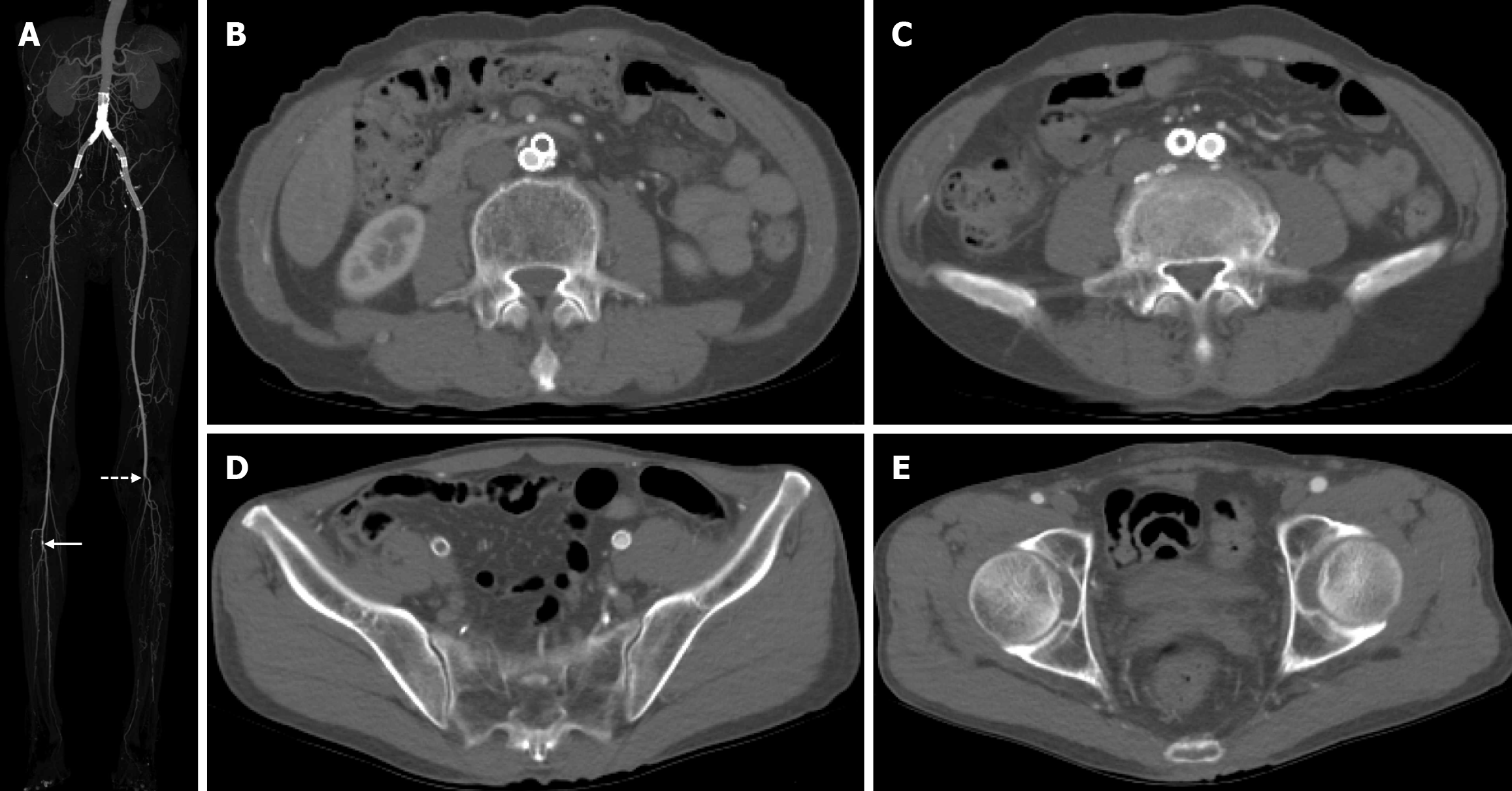
Contrast-enhanced lower extremity computed tomography (CT) revealed thrombotic occlusion of the right aortoiliac stent. The maximal intensity projection (MIP) image demonstrated the aorto-iliac stent placement, mild calcification of the right tibioperoneal trunk, and occlusion of the left popliteal and tibioperoneal arteries (Figure 1A). Serial axial section images showed the thrombotic occlusion of the right aortoiliac stent from the level of the abdominal aorta and right external iliac artery (Figure 1B-E).
The final diagnosis was a thrombotic occlusion of right aortoiliac stenting, mild calcification of right popliteal artery, and complete occlusion of left popliteal and tibioperoneal artery.
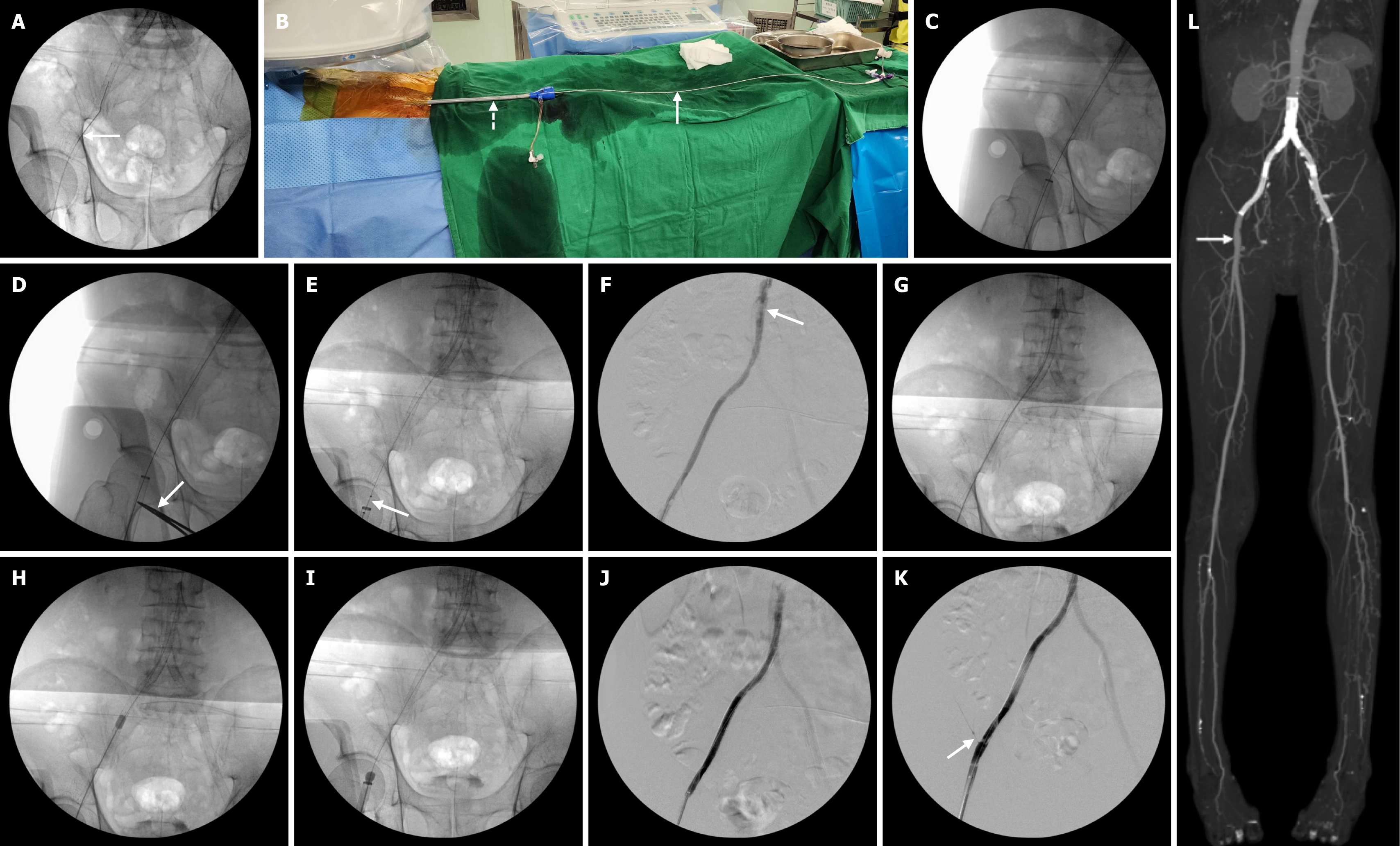
Under general anesthesia, the right common femoral artery was accessed using a micropuncture set under ultrasound guidance. An 035In straight-tip Terumo guidewire (Terumo Corporation, Japan) was inserted through the right common femoral artery (Figure 2A). After successful access, two 6F Proglides (Abbott Vascular, IL, United States) were applied for future closure using a preclose technique. Then, a 22 French Sentrant introducer sheath (Medtronic, Minneapolis, MN, United States) was inserted into the right common femoral artery to prevent distal embolization during the procedure. Then, an Angiojet Omni thrombectomy catheter (Boston Scientific, Marlborough, MA, United States) was introduced through this sheath (Figure 2B). Just before the thrombectomy, a fluoroscopic image showed the successful guidewire passage and placement of a large bore sheath (Figure 2C). A mosquito clamp was placed onto the access site (Figure 2D). It could be helpful to avoid the inadvertent pullout of a large bore sheath during the procedure. Aspirational thrombectomy was performed using an Angiojet Omni thrombectomy catheter in a retrograde fashion from the proximal portion of the abdominal stent down to the distal portion of the right iliac stenting (Figure 2E). After the aspiration thrombectomy, the angiogram demonstrated a nearly complete thrombectomy and residual organized thrombus at the proximal stent portion (Figure 2F). Conventional mechanical thrombectomy was done using a 5.5 Fr over-the-wire Fogarty catheter (Edwards Lifesciences, Irvine, CA, United States) from the proximal portion of the stent to the tip of the sheath (Figure 2G-I). Eventually, the organized thrombus was collected in the large bore sheath. Both aspiration thrombectomy and conventional mechanical thrombectomy were performed slowly and gently (see Video). The completion angiogram showed the complete removal of the thrombus and patent stenting site including the right circumflex iliac artery (Figure 2J and K). Postoperative MIP CT image showed no evidence of distal embolization and access site complication as well (Figure 2L).
After the procedure, the right-side ABI was increased to 1.06. Postoperative CT image showed no evidence of distal embolization and any access site complication (Figure 2L). In the postoperative one year, the stenting site was patent.
This case report demonstrated the detailed treatment of thrombotic occlusion for the aortoiliac stent using a retrograde Angiojet thrombectomy catheter and a large-bore sheath. The patient's history included multiple prior interventions for aortoiliac lesions. The successful application of the Angiojet thrombectomy system, which is frequently employed in treating peripheral arterial thrombotic lesions, showcases its efficacy in a complex aortoiliac setting. The use of a large-bore sheath was a crucial preventative measure against distal embolization, a significant risk in such procedures.
Angiojet thrombectomy system is used to treat the thrombotic lesion in the peripheral artery with an effective mechanical thrombectomy for removing thrombi, restoring and maintaining arterial patency, and alleviating symptoms[6]. This system is designed to remove thrombus with the Venturi-Bernoulli effect, with multiple high-velocity, high-pressure saline jets without the injury of the vessel wall[7]. In this case, there was no evidence of any damage of stent or the vessel wall. However, due to the treatment mechanism of high velocity and high negative pressure, the use of this system may cause hemoglobinuria and renal insufficiency[8]. Therefore, sufficient hydration is recommended with isotonic saline during and after the procedure and alkalizes urine with sodium bicarbonate[9].
One limitation of this system is that the organized thrombus cannot be removed. In this case, we could observe that the organized thrombus at the proximal portion of the stent was not removed after the use of this system. For the removal of this organized thrombus, 0.018″ wires are inserted through the stenting portion of the iliac artery to the abdominal aorta. And 5.5Fr over-the-wire Fogarty catheter is advanced, inflated, and pulled back to the sheath. This gentle procedure could be able to completely remove the organized thrombus.
During both aspiration thrombectomy and mechanical thrombectomy, distal embolization is a possible complication. The placement of an embolic protection device could not be used in this approach. Therefore, we used a large diameter sheath similar to the diameter of a native artery. This sheath has frequently been used for endovascular repair of abdominal aortic aneurysms or transfemoral aortic valve implantation[10]. In particular, during the mechanical thrombectomy using an over-the-wire Fogarty catheter, the balloon was inflated and pulled to the sheath to collect the thrombus inside the sheath without distal embolization. The preclose technique has commonly been used for percutaneous femoral closure after large sheath access[11]. Before the insertion of a large diameter sheath, two Proglide™ suture devices were applied. Eventually, we completed the procedure with total percutaneous application.
The chosen treatment strategy was effective in restoring blood flow to the affected limb, as evidenced by the post-procedure increase in the patient's ABI from 0.67 to 1.06. This improvement showed the significant clinical benefit achieved. The use of both aspiration thrombectomy and conventional mechanical thrombectomy demonstrates a comprehensive approach aimed at completely removing the acute and organized thromb within the stent coupled with the large diameter sheath for the prevention of distal embolization. This case provides valuable information on the management of acute thrombotic occlusion of aortoiliac stent and emphasizes the importance of careful patient selection and a multi-modal approach.
This case report effectively presents a successful management strategy for a complex case of aortoiliac stent occlusion. The detailed description of the procedure, along with the pre-and post-procedural imaging, provides successful management of acute thrombotic occlusion of aortoiliac stent. Future research should focus on larger studies comparing different treatment strategies for aortoiliac stent occlusion to determine optimal approaches and long-term outcomes.
| 1. | Mazzolai L, Teixido-Tura G, Lanzi S, Boc V, Bossone E, Brodmann M, Bura-Rivière A, De Backer J, Deglise S, Della Corte A, Heiss C, Kałużna-Oleksy M, Kurpas D, McEniery CM, Mirault T, Pasquet AA, Pitcher A, Schaubroeck HAI, Schlager O, Sirnes PA, Sprynger MG, Stabile E, Steinbach F, Thielmann M, van Kimmenade RRJ, Venermo M, Rodriguez-Palomares JF; ESC Scientific Document Group. 2024 ESC Guidelines for the management of peripheral arterial and aortic diseases. Eur Heart J. 2024;45:3538-3700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 182] [Article Influence: 182.0] [Reference Citation Analysis (0)] |
| 2. | Shen C, Zhang Y, Qu C, Fang J, Liu X, Teng L. Outcomes of Total Aortoiliac Revascularization for TASC-II C&D Lesion with Kissing Self-Expanding Covered Stents. Ann Vasc Surg. 2020;68:434-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Çakmak EÖ, Bayam E, Yilmaz F, Kahyaoğlu M, Çelik M, Öcal L, Çakir Ç, Karagöz A, Izgi IA. Midterm Outcomes on Primary Endovascular Treatment of 395 Aortoiliac Occlusive Disease Patients: A Single-Center Experience. Angiology. 2021;72:640-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Kudo T, Chandra FA, Ahn SS. Long-term outcomes and predictors of iliac angioplasty with selective stenting. J Vasc Surg. 2005;42:466-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 86] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 5. | Soares RA, Campos ABC, Portela MVV, Brienze CS, Brancher GQB, Sacilotto R. Pharmacomechanical thrombectomy with Angiojet in acute arterial occlusions: A prospective study among the results and outcomes. Vascular. 2025;33:42-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Ascher E, Kibrik P, Rizvi SA, Alsheekh A, Marks N, Hingorani A. Fast-track thrombolysis protocol for acute limb ischemia. J Vasc Surg. 2021;73:950-959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Lee MS, Singh V, Wilentz JR, Makkar RR. AngioJet thrombectomy. J Invasive Cardiol. 2004;16:587-591. [PubMed] |
| 8. | Esteras R, Cannata-Ortiz P, Del Palacio-Tamarit M, Guerrero-Hue M, García-Caballero C, Egido J, Gimeno J, Ortiz A, Gracia-Iguacel C, Moreno JA. Podocyte and tubular involvement in AngioJet-induced kidney injury. Clin Kidney J. 2021;14:424-428. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Meng XH, Xie XP, Liu YC, Huang CP, Wang LJ, Liu HY, Fang X, Zhang GH. Observation of the effect of angiojet to treat acute lower extremity arterial embolization. World J Clin Cases. 2023;11:3491-3501. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 10. | Dimitriadis Z, Scholtz W, Ensminger SM, Piper C, Bitter T, Wiemer M, Vlachojannis M, Börgermann J, Faber L, Horstkotte D, Gummert J, Scholtz S. Impact of sheath diameter of different sheath types on vascular complications and mortality in transfemoral TAVI approaches using the Proglide closure device. PLoS One. 2017;12:e0183658. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Lee WA, Brown MP, Nelson PR, Huber TS. Total percutaneous access for endovascular aortic aneurysm repair ("Preclose" technique). J Vasc Surg. 2007;45:1095-1101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 184] [Article Influence: 10.2] [Reference Citation Analysis (0)] |