Published online Aug 16, 2025. doi: 10.12998/wjcc.v13.i23.105003
Revised: April 6, 2025
Accepted: April 23, 2025
Published online: August 16, 2025
Processing time: 146 Days and 23.9 Hours
Bioabsorbable interference screws are a widely used option for graft fixation in anterior cruciate ligament (ACL) reconstruction. Their ability to degrade over time and avoid secondary hardware removal makes them advantageous. However, complications such as breakage and intra-articular migration of screws can cause significant clinical issues, including joint pain, swelling, and cartilage damage. Early diagnosis and management are critical in such cases.
A 26-year-old male presented with knee pain and swelling one year after ACL reconstruction using a hamstring graft and bioabsorbable tibial interference screw. The patient had been engaged in rigorous physical activity as part of military training. Clinical examination revealed mild effusion without instability, and imaging showed screw breakage with intra-articular migration. Therapeutic arthroscopy confirmed intact graft tension, and broken screw fragments were removed successfully. The patient resumed normal activity two weeks after surgery.
This case highlights the potential complications associated with bioabsorbable screws, emphasizing the need for meticulous surgical technique, postoperative monitoring, and timely intervention. A comprehensive review of the literature illustrates the mechanisms, risk factors, and preventive strategies associated with screw-related complications.
Core Tip: This case report highlights the rare complication of bioabsorbable tibial interference screw breakage and intra-articular migration following anterior cruciate ligament (ACL) reconstruction. It underscores the importance of meticulous surgical technique, vigilant postoperative monitoring, and timely intervention to manage such complications effectively. Therapeutic arthroscopy ensured intact graft function and successful removal of screw fragments, enabling the patient to resume normal activities. A comprehensive literature review elaborates on risk factors, mechanisms, and preventive strategies for complications associated with bioabsorbable screws, contributing valuable insights to improve patient outcomes in ACL reconstruction procedures.
- Citation: Roy M, Bhikshavarthi Math SA, Das D, Dwidmuthe S. Broken bioabsorbable tibial interference screw post-arthroscopic anterior cruciate ligament reconstruction: A case report. World J Clin Cases 2025; 13(23): 105003
- URL: https://www.wjgnet.com/2307-8960/full/v13/i23/105003.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i23.105003
Anterior cruciate ligament (ACL) injuries are among the most common ligament injuries of the knee, particularly in young and active individuals. These injuries are often associated with sports activities, including soccer, basketball, and skiing, which involve rapid changes in direction, pivoting, or high-impact landings. In India, the incidence of ACL injuries is estimated at 68.6 per 100000 individuals annually, with an increasing trend due to higher awareness and participation in athletics[1]. The ACL plays a critical role in maintaining knee stability, and its injury often leads to significant functional impairment, necessitating surgical reconstruction in symptomatic cases.
ACL reconstruction surgery has evolved significantly, with graft fixation methods being a key area of innovation. Autologous grafts, such as hamstring and patellar tendon grafts, remain the gold standard for reconstruction. Among fixation devices, bioabsorbable interference screws have gained popularity due to their ability to provide adequate initial fixation strength while gradually degrading and being replaced by native bone[2]. Compared to metallic screws, bioabsorbable screws offer distinct advantages, including the elimination of permanent hardware, easier revision surgeries, and reduced imaging artifacts during postoperative evaluations[3].
Despite these advantages, complications associated with bioabsorbable screws have been reported. These include delayed degradation, breakage, and migration, leading to pain, swelling, and mechanical symptoms. The degradation process is influenced by multiple factors, such as material composition, mechanical stress, and the local environment of the screw. Poly-lactic acid, the most commonly used material for bioabsorbable screws, degrades through hydrolysis, a process that can extend over several years[4]. When exposed to synovial fluid, degradation slows significantly, increasing the risk of fragmentation and intra-articular complications.
This case report explores the clinical presentation, imaging findings, and surgical management of a fractured bioabsorbable tibial interference screw one year post-ACL reconstruction. A comprehensive review of similar cases in the literature provides insights into the mechanisms, risk factors, and preventive strategies for these complications, emphasizing the importance of surgical precision and early intervention.
The patient presented with persistent pain and swelling over the proximal tibial region of the operated knee, especially during weight-bearing activities.
A 30-year-old male presented six months post-ACL reconstruction with complaints of anterior knee pain and a palpable hard swelling over the proximal tibial region. He had been previously asymptomatic after surgery until the last 2 months when he began noticing discomfort during activity, along with intermittent pain over the tibial tunnel site.
The patient had undergone arthroscopic ACL reconstruction using a hamstring autograft with bioabsorbable interference screws (both femoral and tibial) at a tertiary hospital. The procedure was uneventful, and he was on a standard post-operative rehabilitation protocol.
There was no significant personal or family history of systemic illness, metabolic bone disease, or genetic disorders. The patient was a non-smoker and had no known drug allergies.
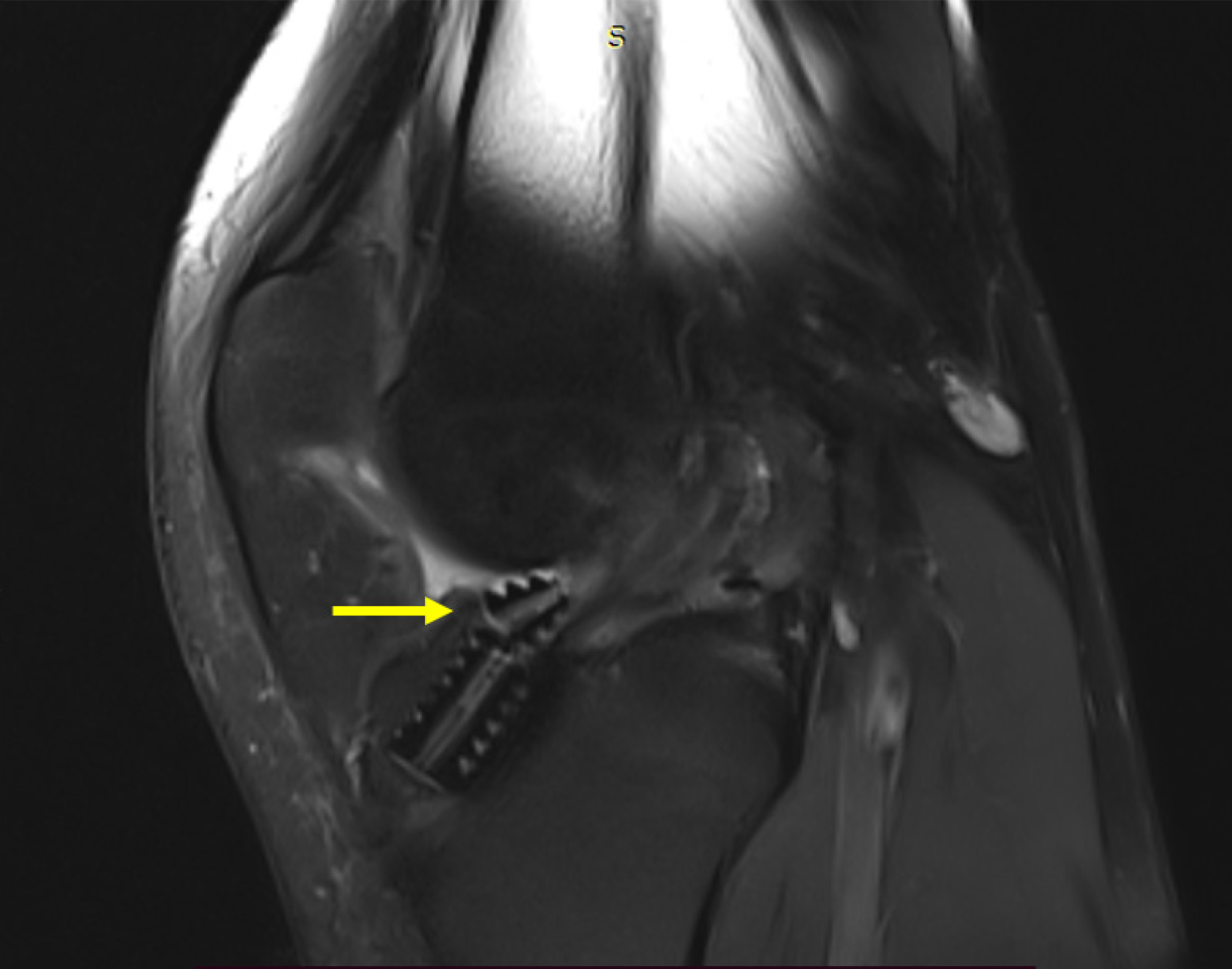
On examination, the patient had mild effusion in the right knee, with a full range of motion except for terminal flexion, which was associated with discomfort. Stability tests, including Lachman, anterior drawer, and pivot-shift tests, were negative, indicating no graft laxity. Tenderness was absent over the medial and lateral joint lines, and there were no signs of patellar instability or maltracking (Figure 1).
Routine blood investigations including complete blood count, erythrocyte sedimentation rate, and C-reactive protein were within normal limits, ruling out any ongoing infection.
Radiographs of the knee revealed a fragmented broken bioabsorbable screw in the tibial tunnel region, with adjacent osteolysis and localized periosteal reaction. Magnetic resonance imaging confirmed the presence of screw fragments with associated tunnel widening but no graft compromise (Figure 2).
Symptomatic broken tibial bioabsorbable interference screw with local osteolysis post-arthroscopic ACL reconstruction.
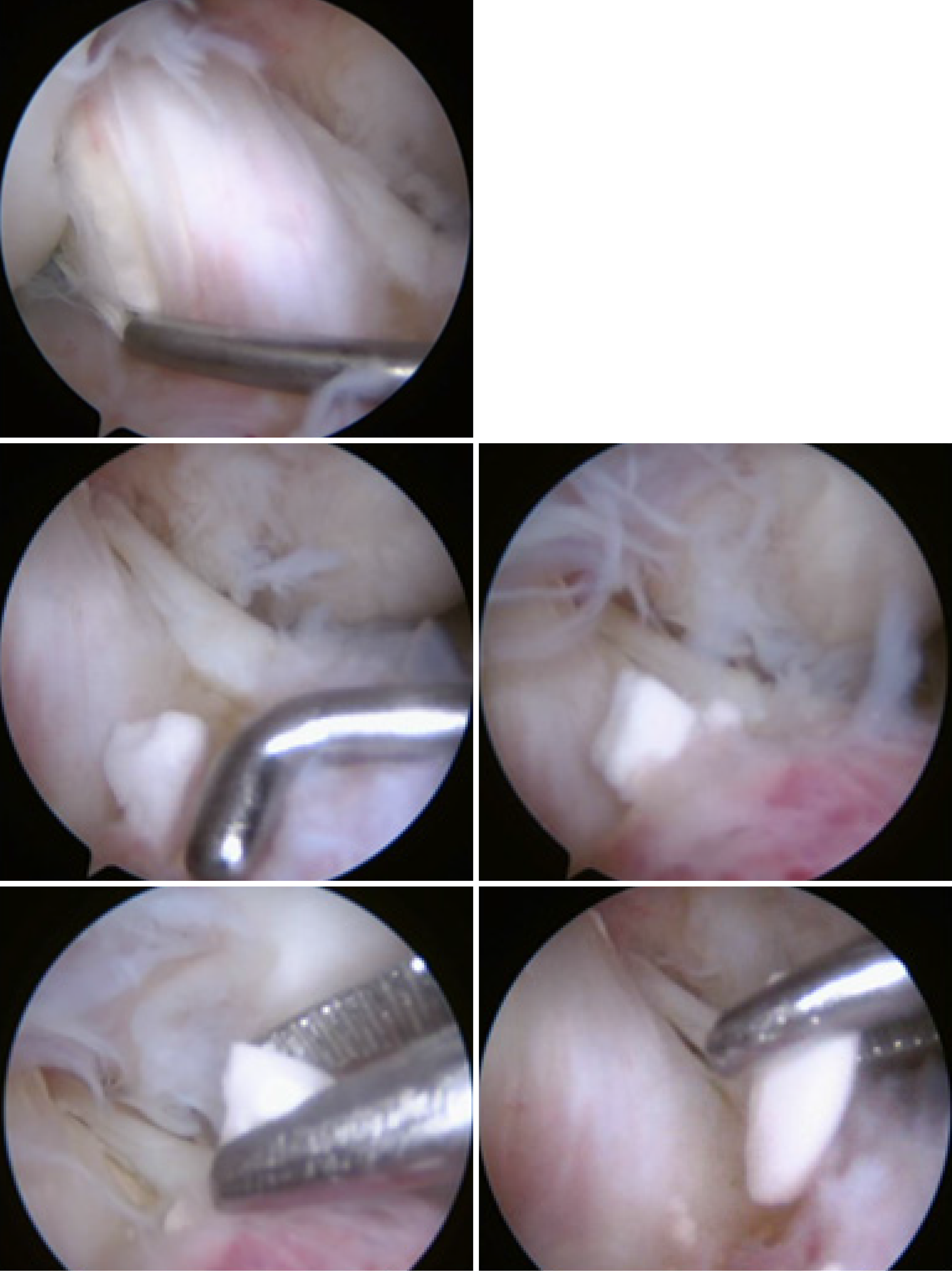
Surgical exploration was performed through the standard arthroscopic antero-lateral and antero-medial portals (Figure 3). Broken screw fragments were identified within the tibial tunnel and surrounding soft tissue and were completely removed (Figure 4). The tunnel was debrided, and local curettage was performed. As the ACL graft remained intact and functional, no revision grafting was required.
The patient had an uneventful post-operative recovery. At 6 months follow-up, he reported complete resolution of symptoms with no residual swelling or instability. Repeat radiographs showed no further osteolysis. He returned to routine physical activities and light sports participation without complaints.
Bioabsorbable interference screws are widely used in ACL reconstruction for their ability to integrate into bone and degrade over time. However, complications such as screw breakage, migration, and delayed degradation can lead to significant clinical issues[5]. In the present case, the high mechanical demands of military training likely exacerbated stress on the screw, leading to its breakage and migration into the joint. This complication is consistent with previous reports in the literature.
Appelt and Baier[6] reported a similar case of screw migration four months post-surgery, causing recurrent knee locking. Arthroscopic retrieval of the broken screw fragments relieved the symptoms. Hall et al[5] described early screw fractures leading to chondral injury due to prolonged irritation by the fragments. Morgan et al[7] provided histological evidence of uneven degradation and synovial inflammation associated with bioabsorbable screws. These cases highlight the importance of screw placement and early recognition of complications.
The degradation of bioabsorbable screws is influenced by their material composition and the environment in which they are placed[8]. Martinek et al[9] found that screws embedded in cancellous bone degrade predictably within five years, while those exposed to synovial fluid degrade more slowly, increasing the risk of fragmentation and migration. This underscores the importance of ensuring that screws are flush with or recessed within the bone to minimize exposure to joint fluid.
Additionally, patient-specific factors such as bone mineral density, biomechanics, and activity level may contribute to implant failure. In high-demand populations such as military personnel, mechanical fatigue and micromotion at the graft-screw interface can predispose screws to breakage. Shen et al[4] conducted a meta-analysis of randomized controlled trials that showed no statistically significant difference in clinical outcomes between bioabsorbable and metallic interference screws. However, bioabsorbable screws were more frequently associated with adverse events such as inflammatory reactions and screw breakage[4].
Preventive measures include meticulous screw placement during surgery, ensuring that the tip does not protrude into the joint. Routine postoperative arthroscopy can help identify malpositioned screws early, allowing for timely correction. Advances in biomaterials, including screws with predictable degradation profiles, may further reduce the risk of complications[10].
Recent studies also highlight the potential of natural compounds in bone healing. For instance, Liu et al[11] demonstrated that Epimedium water extract modulates neuropeptide signaling and improves bone metabolism in an ovariectomized rat model. Compounds like icariin have been shown to suppress pro-inflammatory markers and enhance bone formation, offering potential adjunctive support in implant-related bone healing[11].
Alternative fixation techniques such as cortical button systems, cross-pins, and hybrid methods offer biomechanical advantages in specific scenarios. Kousa et al[12] compared six devices and found cortical button fixation to provide superior strength in hamstring graft fixation.
Technological advances in surgical instrumentation may also contribute to improved outcomes. Chenet al[13] showed that the V-blade tip needle scalpel significantly reduced operation time in ultrasound-guided percutaneous A1 pulley release. Similar precision tools could enhance the efficiency and accuracy of ACL reconstruction procedures[13].
Future research should include experimental models such as patient-derived xenografts or large animal trials to validate biomechanical and degradation performance. Moreover, high-throughput methods like clustered regularly interspaced short palindromic repeats (CRISPR) screening can help identify genes involved in immune modulation and implant degradation. Liu et al[14] demonstrated how CRISPR and half-maximal inhibitory concentration data could uncover resistance mechanisms, suggesting a translational application in biomaterials research.
This case highlights the potential complications of bioabsorbable tibial interference screws in ACL reconstruction, emphasizing the importance of meticulous surgical technique, routine postoperative monitoring, and early intervention. While bioabsorbable screws offer significant advantages, their risks must be carefully managed to optimize patient outcomes. A detailed understanding of the mechanisms and preventive strategies associated with screw-related complications is essential for improving the success of ACL reconstruction surgeries.
| 1. | Khatri NP, Bharali I, Khan I, Borgohain GS. Arthroscopic Single-Bundle Anterior Cruciate Ligament Reconstruction Using the Quadrupled Hamstring Tendon Graft: A Single-Institution Experience From North-Eastern India. Cureus. 2023;15:e40547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Kousa P, Järvinen TL, Vihavainen M, Kannus P, Järvinen M. The fixation strength of six hamstring tendon graft fixation devices in anterior cruciate ligament reconstruction. Part II: tibial site. Am J Sports Med. 2003;31:182-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 186] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 3. | Brand JC Jr, Nyland J, Caborn DN, Johnson DL. Soft-tissue interference fixation: bioabsorbable screw versus metal screw. Arthroscopy. 2005;21:911-916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 42] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 4. | Shen C, Jiang SD, Jiang LS, Dai LY. Bioabsorbable versus metallic interference screw fixation in anterior cruciate ligament reconstruction: a meta-analysis of randomized controlled trials. Arthroscopy. 2010;26:705-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Hall MP, Hergan DM, Sherman OH. Early Fracture of a Bioabsorbable Tibial Interference Screw After ACL Reconstruction With Subsequent Chondral Injury. Orthopedics. 2009;32:1-3. [DOI] [Full Text] |
| 6. | Appelt A, Baier M. Recurrent locking of knee joint caused by intraarticular migration of bioabsorbable tibial interference screw after arthroscopic ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2007;15:378-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Morgan CD, Gehrmann RM, Jayo MJ, Johnson CS. Histologic findings with a bioabsorbable anterior cruciate ligament interference screw explant after 2.5 years in vivo. Arthroscopy. 2002;18:E47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Bergsma JE, de Bruijn WC, Rozema FR, Bos RR, Boering G. Late degradation tissue response to poly(L-lactide) bone plates and screws. Biomaterials. 1995;16:25-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 632] [Cited by in RCA: 541] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 9. | Martinek V, Seil R, Lattermann C, Watkins SC, Fu FH. The fate of the poly-L-lactic acid interference screw after anterior cruciate ligament reconstruction. Arthroscopy. 2001;17:73-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 45] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Weiler A, Hoffmann RF, Stähelin AC, Helling HJ, Südkamp NP. Biodegradable implants in sports medicine: the biological base. Arthroscopy. 2000;16:305-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 151] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 11. | Liu H, Xiong Y, Wang H, Yang L, Wang C, Liu X, Wu Z, Li X, Ou L, Zhang R, Zhu X. Effects of water extract from epimedium on neuropeptide signaling in an ovariectomized osteoporosis rat model. J Ethnopharmacol. 2018;221:126-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 59] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 12. | Kousa P, Järvinen TL, Vihavainen M, Kannus P, Järvinen M. The fixation strength of six hamstring tendon graft fixation devices in anterior cruciate ligament reconstruction. Part I: femoral site. Am J Sports Med. 2003;31:174-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 263] [Cited by in RCA: 225] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 13. | Chen M, Li B, Liu H. V-blade tip needle scalpel reducing surgery time in ultrasonography-guided percutaneous A1 pulley release. Asian J Surg. 2025;48:950-951. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Liu H, Wang P. CRISPR screening and cell line IC50 data reveal novel key genes for trametinib resistance. Clin Exp Med. 2024;25:21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 15.0] [Reference Citation Analysis (0)] |