INTRODUCTION
Tinnitus, a common symptom often encountered in otolaryngology, refers to the perception of sounds in the ears without any external auditory stimuli[1,2]. A recent study revealed that over 740 million people worldwide experience tinnitus to varying degrees, with over 120 million suffer from severe tinnitus[3]. The prevalence of tinnitus increases with age, with rates reaching up to 40% in the elderly[4,5]. This trend is expected to persist as the world industrializes and ages[6]. Furthermore, 0.5%-2% of patients with tinnitus experience significant secondary symptoms of tinnitus, including insomnia, difficulty concentrating, and depression[7].
The pathophysiologic mechanisms underlying tinnitus remain incompletely understood[8,9]. Current treatment options for these conditions yield unsatisfactory outcomes[10,11], complicating the ability to determine the most suitable and promising treatment for individual patients. The limited number of evidence-based treatment options that have shown efficacy across all tinnitus types aim to reduce the disability associated with tinnitus itself rather than targeting the underlying cause or symptoms[12]. Auditory stimulation and cognitive behavioral therapy are the main management regimens used to modulate the mechanism of tinnitus[6,13]. Patients with tinnitus often explore various potential treatment options[14] and may seek out additional unstructured and non-standardized practices in their pursuit of effective treatment[15]. Furthermore, over 4 million off-label prescriptions for tinnitus relief are issued annually in Europe and the United States, although their efficacy remains questionable[6,13].
Given the economic burden that tinnitus imposes on patients and the healthcare system, minimizing the utilization of unnecessary, ineffective, and costly treatment strategies should be prioritized[9]. With the prevalence of tinnitus and the lack of standardized treatments, focusing more on complementary and alternative medicine treatments is advisable[16]. Korean medicine (KM) treatments for tinnitus have a rich history documented in KM or traditional Chinese medicine (TCM) classics, spanning thousands of years and providing historical evidence. Various interventions, including acupuncture (such as manual acupuncture, electroacupuncture, warm needling, moxibustion, pharmacopuncture, and so on.), herbal medicine, and Chuna therapy have been used alone or in combination to treat tinnitus, with reported effectiveness[16-20]. However, accumulated clinical evidence remains lacking. Therefore, we present a case of a patient with left-sided tinnitus persisting for > 10 years, concomitant with headache and neck pain without symptomatic improvement despite intermittent treatment with Western medications and four recent steroid tympanic membrane injections. Across 11 treatment sessions, significant improvement was observed in tinnitus, headache, and neck pain following two combined KM treatments. Subsequently, the intermittent tinnitus was resolved using temporomandibular joint (TMJ) balancing therapy, and all improvements were maintained.
TREATMENT
KM treatment methods
Overall, 11 treatment sessions were conducted, consistently employing acupuncture, herbal medicine, and Chuna therapy. Additionally, TMJ balancing therapy was introduced during the 8th session. With regard to acupuncture-related interventions, acupuncture treatment was performed on GB34, BL60, LR4, GB30, BL54, SI13, SI12, SI11, TE17, TE18, TE19, TE20, C3-4-5, and T3-4-5 Hyeopcheok points for 10 minutes according to the principles of the Juheng acupuncture method. For the thoracic spine region, acupuncture was complemented with electroacupuncture and electronic moxibustion. In this case, the patient was diagnosed with liver qi stagnation. To alleviate emotional tension, GB34 and LR4, acupoints on the gallbladder and liver meridians respectively, were selected. BL60, commonly used for treating stiffness in the neck and shoulder tension, was also added. To aid blood circulation in the reproductive system and address heavy menstrual bleeding with clots, GB30 and BL54 were incorporated. SI11, SI12, and SI13 were used to relieve headache and neck pain by promoting relaxation of the shoulder muscles. Finally, TE17, TE18, TE19, and TE20, acupoints commonly used for tinnitus, were included. Therefore, various symptoms presented by the patient were addressed by utilizing diverse acupoints. Additionally, dry cupping was performed on the entire back.
For the herbal medicine, gamisoyosan (GSS, Kamisoyosan), known as one of the three major prescriptions for women, was prescribed to treat dysmenorrhea, insomnia, and anxiety for 15 days. Kracie GSS Ext Fine Gran (Kyungbang Shinyak) was administered twice daily. Chuna treatment encompasses site-specific techniques, including fascia and joint distraction Chuna, which was administered to the cervical, thoracic, and lumbar spine. For residual symptoms, TMJ balancing therapy was performed to balance the cranial nervous system and adjust the yin and yang meridian. For TMJ balancing therapy[21], a cervical high-velocity low-amplitude thrust technique was performed with the initial TMJ measured at 49:32. Upon confirming symptoms alleviation on the 9th treatment day, oral size was measured, and Accurate Balancing Appliance size 5, a standard intraoral balancing appliance produced by Jinbiotech Company was prescribed, followed by pelvic balancing therapy and conventional KM treatment.
Assessment methods
The tinnitus handicap inventory (THI), a self-report questionnaire used to assess the impact of tinnitus on an individual’s daily life, is widely used in clinical and research settings as a tool to evaluate the effectiveness of tinnitus treatments and to measure changes in tinnitus severity over time[22]. The headache impact test-6 (HIT-6), which has proven useful in generating quantitative and relevant information about the impact of headache, is a six-item questionnaire with scores ranging from 36 to 78, with higher scores indicating greater impact on the respondent’s daily life[23]. The neck disability index (NDI) is the most commonly used neck-related patient-reported outcome measure and consists of a 10-item self-report questionnaire of neck pain-related disability[24]. In this study, tinnitus was assessed using the Korean version of the THI, while headache was evaluated using the Korean version of the HIT-6. Additionally, neck pain was assessed using the Korean version of the NDI.
OUTCOME AND FOLLOW-UP
On treatment day 1 (December 16), the THI score was 68, the HIT-6 score was 64, and the NDI score was 21. Acupuncture treatment, Chuna therapy, and an herbal medicine prescription were administered. Immediately following the acupuncture treatment, the patient reported relief, with the resolution of throbbing sensations and subjective heat around the left ear, accompanied by a tingling sensation comparable to the sensation when the anesthesia wears off. During the second treatment day (December 20), significant improvement in left-sided tinnitus was observed, with the ear ringing and heat sensation continuing to improve. However, left eye twitching, headache, and neck pain persisted at similar levels. Consequently, the same treatment protocol was applied. On treatment day 3 (December 22), the left-sided tinnitus had substantially decreased. Furthermore, the headache and neck pain had subsided (HIT-6 score 36, NDI score 0). However, the left-sided eye twitching persisted at a similar level. The same treatment regimen was continued.
One week later, during the 4th treatment session (December 29), the patient reported experiencing left-sided tinnitus alongside a constant headache. Moreover, the tinnitus, which typically did not occur, would intermittently manifest when consuming coffee, lasting for approximately 1 hour. Furthermore, she experienced a mild pulsating headache lasting approximately 30 minutes before dissipating, and her left eye twitching had decreased by 80%. Back neck pain had resolved, and bowel movements normalized and abdominal distension decreased, as reported by the patient. No chest pain was reported, which had previously occurred 1-2 times per week for the preceding week. The same treatment was implemented, and a further 10-day course of medication was prescribed. On the 5th treatment day (January 3, 2024), the patient reported that her left-sided tinnitus was manageable with one cup of coffee and resolved completely after consuming two cups. Additionally, her left-sided eye twitching had decreased by 80%, and the headache and back neck pain she experienced had resolved. During this period, she reported improvement in anger, with an estimated reduction of more than 50%. Furthermore, she was less irritable than usual with the medication. The same treatment regimen was administered. Two weeks later, during the 6th treatment day (January 17), the patient reported a recurrence of left-sided tinnitus, which had previously disappeared 8 days earlier. This resurgence was attributed to stress and prolonged computer use throughout the day. Moreover, the patient observed that the back neck pain had returned, while the left eye twitching had decreased by 80%. However, the headache persisted without change. The same treatment was continued.
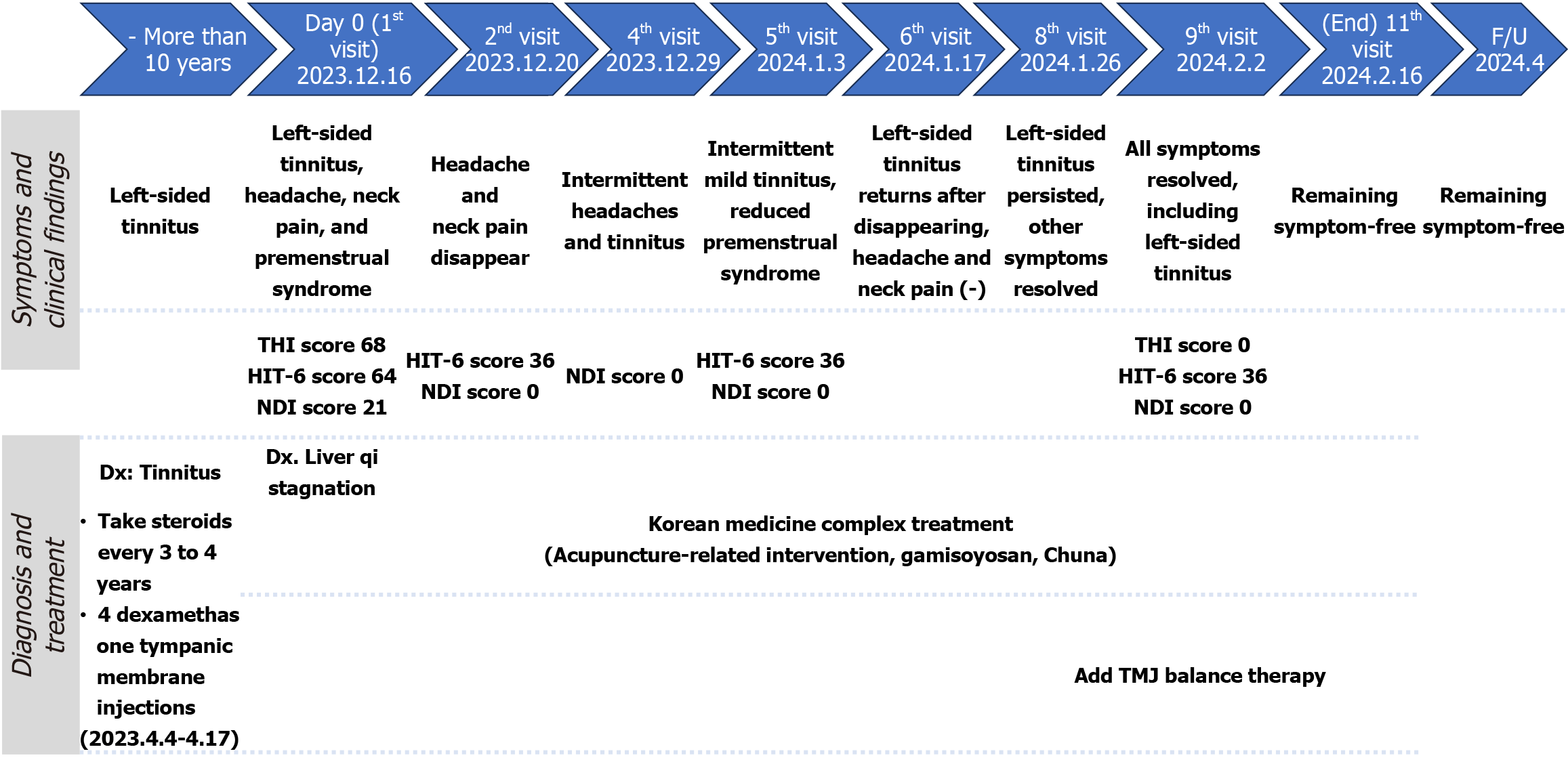
On the 8th treatment day (January 26), the left-sided tinnitus persisted while other symptoms had resolved. To address this, we opted to incorporate additional TMJ balancing therapy. The cervical high-velocity low-amplitude thrust technique was employed, with the initial TMJ height measured at 49:32. Additionally, we administered the same KM treatment as in the previous session. On the 9th treatment day (February 2, 2024), it was confirmed that the left-sided tinnitus had ceased and all other symptoms remained absent (THI score 0, HIT-6 score 36, and NDI score 0). The patient reported new bilateral knee pain following balance exercises a week earlier. To address this, we prescribed Accurate Balancing Appliance No. 5 for home use and included one session of pelvic balancing therapy as part of the TMJ balancing regimen. Moreover, the same KM treatment regimen was performed as before. On day 10 (February 7), symptomatic improvement persisted, with only residual knee pain observed on the right side, and the same treatment was administered. On the 11th treatment day (February 16), the patient remained stable and reported continued improvement in her anger management during her menstrual cycle in February. The same treatment regimen was repeated. There were no significant adverse events during the treatment period, and the patient expressed satisfaction with the treatment outcomes. Subsequent follow-up at two months confirmed sustained symptom resolution (Figure 1).
Figure 1 Timeline of case study.
F/U: Follow-up; Dx: Diagnosis; THI: Tinnitus handicap inventory; HIT: Headache impact test; NDI: Neck disability index; TMJ: Temporomandibular joint.
DISCUSSION
A study investigating the current treatment landscape for subjective tinnitus in Korea[25] revealed a lack of established treatment standards[26]. Several treatment approaches are used, including counseling (Cognitive behavioral therapy and tinnitus retraining therapy), sound therapy, music therapy, medication, intratympanic injection therapy, repetitive transcranial magnetic stimulation, electrostimulation, TMJ therapy, muscle therapy, myofascial trigger point injection therapy, hearing aids, reassurance and observation, and other therapies. Furthermore, most people attempt five or more different treatments. Tinnitus treatment in the study was categorized into four approaches. First, interventions aimed at blocking pathophysiological mechanisms in the inner ear (the peripheral auditory organ). Second, to aid patients in managing tinnitus-associated symptoms such as depression, anxiety, and insomnia, through psychological and spiritual support. Third, approaches focused on correcting abnormalities in the auditory center by leveraging brain plasticity. Finally, treatment targeting somatosensory tinnitus, which arises from factors unrelated to hearing, utilizes treatments based on the somatosensory system. Achieving consistently high treatment success rates is challenging when using a singular treatment approach for all tinnitus patients. Furthermore, the complexity of tinnitus etiology makes sustained therapeutic effects difficult to attain. The growing recognition of subjective tinnitus as a multifactorial condition, with diverse clinical presentations, has prompted efforts to optimize treatment efficacy through combined therapeutic approaches[25,26].
The patient in this case had a pre-existing diagnosis of tinnitus and had previously received oral steroid medication on three occasions and intratympanic steroid injections from local otolaryngologists. Intratympanic steroids have demonstrated efficacy in several studies for treating tinnitus[27], with a well-established safety profile across various inner ear conditions, including labyrinthine syphilis, Meniere’s disease, sudden sensorineural hearing loss, streptomycin poisoning, acoustic trauma, and head injury[28]. It can be administered to patients with diabetes and to those for whom oral glucocorticoids are contraindicated. Moreover, it serves as a salvage therapy option after the failure of initial treatment[29,30]. However, the lack of response in this patient indicated chronic tinnitus of multifactorial origin, necessitating a comprehensive treatment strategy. Consequently, a comprehensive approach combining acupuncture-related treatments, Chuna, and KM treatments was implemented. This approach aimed to improve structural abnormalities, regulate autonomic nerves, improve psychological symptoms, and regulate the yin-yang balance of the spinal joints and cranial nervous system. Treatment commenced by considering comorbid symptoms, and the patient experienced significant improvement in the symptoms after the first session, with almost all symptoms resolving after the second treatment, showing rapid improvement within a short time. Subsequently, the patient showed intermittent tinnitus symptoms of mild intensity. Therefore, TMJ balancing therapy was performed to sustain the absence of symptoms and improve the quality of life and satisfaction of the patients.
In KM and TCM, tinnitus is attributed to various causes, including imbalances in specific organs, such as liver fire, gallbladder fire, spleen-stomach weakness, heart blood deficiency, kidney essence insufficiency, and externally contracted wind-heat[31]. Treatment approaches encompass acupuncture, herbal medicine, counseling, Chuna, and qigong[17-19,32-34], and research has also shown that cervical-mandibular manual therapy effectively improves tinnitus[35]. The patient, in this case, was diagnosed with liver qi stagnation based on a combination of pulse diagnosis, tongue diagnosis, etc. Treatment involved a combination of acupuncture-related interventions (acupuncture, electroacupuncture, cupping, and electronic moxibustion) and herbal medicine.
Clinical and experimental studies have confirmed the significant role of acupuncture in regulating neurophysiology associated with the otolithic nucleus, non-classical ascending auditory pathways, neuroplasticity, and somatosensory systems[34]. Moreover, acupuncture has demonstrated efficacy in reducing tinnitus symptoms and improving quality of life[36,37]. Although Japanese and European tinnitus treatment guidelines do not recommend acupuncture[38,39], several systematic reviews have explored its efficacy in treating tinnitus[8,40,41]. A recent network analysis investigating acupuncture for tinnitus[16] highlighted its efficacy and found that a combination of warm needling and pharmacopuncture was most effective. Studies indicate that chronic tinnitus exerts a more significant influence on autonomic nervous disorders than acute tinnitus and that KM/TCM treatments, such as acupuncture, can regulate autonomic nervous function in patients with tinnitus[18]. In addition, a study revealed that acupuncture treatment for patients with chronic tinnitus affects dynamic functional connectivity in brain activity[42]. In this study, the Juheng acupuncture method (a traditional Korean acupuncture technique) was used, targeting various acupuncture points to achieve overall harmony in the human body. This approach involved treating acupuncture points along corresponding meridians based on the principle of holistic body treatment. Cupping, electro-acupuncture, and electronic moxibustion were also utilized as part of the treatment. These acupuncture-related treatments may have exerted therapeutic effects by regulating the meridians of the patients, strengthening vagus nerve function, and regulating the autonomic nervous system. Herbal medicines have traditionally been used to treat tinnitus, with the belief that they improve quality of life and treat associated comorbidities. GSS, a Japanese Kampo preparation known for its effectiveness in treating neuroses, insomnia, menopausal disorders, and dysmenorrhea, has shown promise in treating tinnitus[43,44]. In this study, we prescribed GSS.
Chuna - a KM manual technique - involves using the hands to help patients maintain homeostasis, restore disturbed equilibrium, and treat structural and functional issues. By relaxing tense muscles, correcting deformed skeletal systems, and regulating autonomic nervous system homeostasis, Chuna can contribute to the improvement of dysautonomia-associated symptoms[45]. A study investigating the effectiveness of Chuna for tinnitus revealed that combining Chuna therapy with acupuncture and herbal treatments significantly improved tinnitus symptoms[17]. In our study, employing a combination of Chuna therapy and acupuncture appeared to effectively improve tinnitus symptoms and associated neck pain and headache.
TMJ balancing therapy is a treatment method designed to restore systemic meridian yin-yang balance by addressing the yin-yang equilibrium of the spinal joint system and cranial nervous system. It facilitates the self-regulation and adaptive capacity of the body, thereby enhancing its inherent ability for health promotion and disease treatment. TMJ balancing therapy has been reported to improve spinal misalignment, alleviate symptoms of long-standing Tourette's disorder, and mitigate symptoms of chronic movement disorders[21,46,47]. A reduction in the depth of the TMJ is associated with an increased incidence of tinnitus[48]. In addition, tinnitus is more common in patients with TMJ disorders[49]. The use of a TMJ splint may reduce the severity of tinnitus[50]. In this study, we hypothesized that correcting asymmetrical TMJ heights to restore TMJ balance could alleviate residual symptoms through cranial nerve balancing and meridian yin-yang adjustment.
In this case, a patient with chronic tinnitus, accompanied by headaches, cervical pain, and premenstrual syndrome, received integrated Korean Medicine treatment. Acupuncture was employed to stimulate the pathways of the trigeminal, facial, glossopharyngeal, vagus, and parasympathetic nerves - nerves implicated in ear function - alongside surrounding muscles and soft tissues. Additionally, acupuncture, TMJ balancing therapy, and Chuna therapy were utilized to regulate homeostasis in the autonomic nervous system. Herbal medication was also administered to address psychological factors and gastrointestinal function. This case highlights the potential for maximizing treatment efficacy through the integrated application of diverse KM treatment modalities. Moreover, the clinician effectively mitigated the patient's daily discomfort within a short timeframe by integrating and adapting various treatments. The rapid improvement in symptoms highlights the potential of this integrated approach. The clinical implications of this case extend beyond this single patient. Although the single-case design of this study limits its representativeness, the rapid and sustained improvement observed suggests that such integrative strategies may be applicable to a broader population of tinnitus patients, especially those unresponsive to conventional Western therapies. Indeed, Western approaches, primarily focused on auditory stimulation and cognitive behavioral therapy, often prioritize symptom management rather than addressing underlying physiological dysfunction. Conversely, the integrative KM approach may offer a valuable complementary strategy by targeting both physiological and psychological aspects of chronic tinnitus.
However, potential limitations must be acknowledged. The retrospective design of the study and the inability to isolate the effects of each individual treatment raise concerns regarding confounding factors and selection bias. These limitations make it difficult to definitively characterize the effect of the KM interventions. Further research involving additional cases, well-designed prospective studies, and direct comparisons with Western medical treatments is needed. Such studies would help to validate the efficacy of KM therapies, reduce potential bias, and contribute to the development of tailored treatment protocols for chronic tinnitus.