Published online Jul 16, 2025. doi: 10.12998/wjcc.v13.i20.105606
Revised: February 24, 2025
Accepted: March 17, 2025
Published online: July 16, 2025
Processing time: 69 Days and 22.8 Hours
While existing literature on ischiofemoral impingement syndrome (IFI) predo
The patient underwent comprehensive physical and clinical examination, in
The study highlights the importance of a comprehensive approach to diagnosing and managing IFI, combining clinical assessment with imaging and implementing a multimodal rehabilitation program for optimal outcomes.
Core Tip: A tailored physical therapy program, including activity modification, stretching, strengthening, kinesiology taping, and dry needling effectively reduced her pain and improved her quality of life. The study highlights the importance of a comprehensive approach to diagnose and manage ischiofemoral impingement syndrome, combining clinical assessment with imaging and implementing a multi-modal rehabilitation program for optimal outcomes.
- Citation: Mohammed FA, Alotaibi AN, Hamdi MA, Alshoweir NA, Albarrati AM. Physical therapy management of ischiofemoral impingement syndrome: A case report. World J Clin Cases 2025; 13(20): 105606
- URL: https://www.wjgnet.com/2307-8960/full/v13/i20/105606.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i20.105606
Ischiofemoral impingement syndrome (IFI), a condition that is less frequently encountered by musculoskeletal clinicians, affects a significant portion of the population who experience hip pain, with prevalence increasing with age[1]. First described in 1977, IFI is an abnormal narrowing of the space between the ischium and the lesser trochanter that impinges the quadratus femoris muscle[2,3]. It is commonly seen in females due to various factors, including wider pelvic struc
Factors contributing to IFI may be congenital or acquired[6,7]. Congenital factors such as hip dysplasia and coxa valga are commonly reported anomalies in individuals with IFI. On the other hand, acquired factors such as weakness of hip abductors and extensors contribute to an increased risk of IFI[6,7]. Individuals with IFI often report posterior buttock pain radiating down the leg that mimics sciatica. This pain usually worsens with weight-bearing activities and is associated with snapping/clunking sensations in the hip joint and pain[6,8].
IFI remains a challenging diagnosis for many musculoskeletal clinicians due to the nonspecific nature of its clinical presentation and similarity with other prevalent conditions. Physical examination, clinical testing, and imaging can provide a definitive diagnosis[9].
Symptomatic individuals with a confirmed diagnosis of IFI may be treated conservatively or surgically[10-12]. Conservative management includes activity modification, pain medication, and physical therapy. This case report aims to evaluate the effectiveness of a structured and personalized physical therapy program in reducing pain, enhancing functional abilities, and improving the overall quality of life in a patient with IFI. Due to the rarity of IFI and the limited research on non-surgical treatment options, this study seeks to expand the current body of knowledge by emphasizing conservative management approaches for this condition.
While existing literature primarily focuses on surgical interventions, activity modification, pain relief strategies, and general physical therapy methods, there remains a significant gap in the body of knowledge regarding the specific impact of a structured and tailored rehabilitation program designed to address the biomechanical and functional deficits associated with IFI. This case report endeavours to fill this gap by offering clinical insights into the effectiveness of targeted rehabilitation techniques. The findings may contribute to future research and clinical practice, advancing evidence-based conservative management for IFI.
A young woman in her early 20 s complained of intermittent, severe pain in her right posterior hip.
The patient presented with no prior trauma and presented with chronic, intermittent right posterior hip pain characterized by a sharp, snapping sensation. The pain radiated distally along the posterior thigh to the level of the popliteal fossa and was exacerbated by prolonged weight-bearing activities, such as walking. Symptoms were notably alleviated with sitting. The onset of pain occurred during early adolescence, with recurrent episodes managed conservatively using non-steroidal anti-inflammatory drugs (NSAIDs), which provided partial relief.
The patient presented with an unremarkable past medical history, having no previously documented systemic illnesses, surgical interventions, or traumatic events.
The patient denies any family history of musculoskeletal disorders or hereditary conditions that could predispose her to her current clinical presentation.
The physical evaluation revealed an absence of any visible scars or signs of prior trauma in the affected region. On palpation, tenderness was localized to the right posterior gluteal area, specifically lateral to the ischial tuberosity, accompanied by an audible snap during hip movement. The patient rated her pain intensity as 9/10 on the numerical pain rating scale, denoting severe discomfort.
The range of motion of the hip was within normal limits; however, pain was elicited at the terminal positions of extension, adduction, and external rotation. Manual muscle testing demonstrated notable weakness in the hip abductors and external rotators, with both groups scoring 3/5. Gait analysis revealed an antalgic pattern, characterized by a shortened stride on the affected side.
Examination of the lumbar spine and neurovascular status was unremarkable. Furthermore, specialized provocative tests—including the long stride walking test, the IFI test, and the Trendelenburg sign—were all positive, reinforcing the clinical suspicion of IFI.
Routine laboratory investigations, including a complete blood count, erythrocyte sedimentation rate, C-reactive protein, and basic metabolic panel, were performed and yielded results within normal limits. These findings effectively excluded systemic inflammatory or infectious processes, thereby reinforcing the clinical diagnosis of IFI syndrome as an isolated musculoskeletal condition.
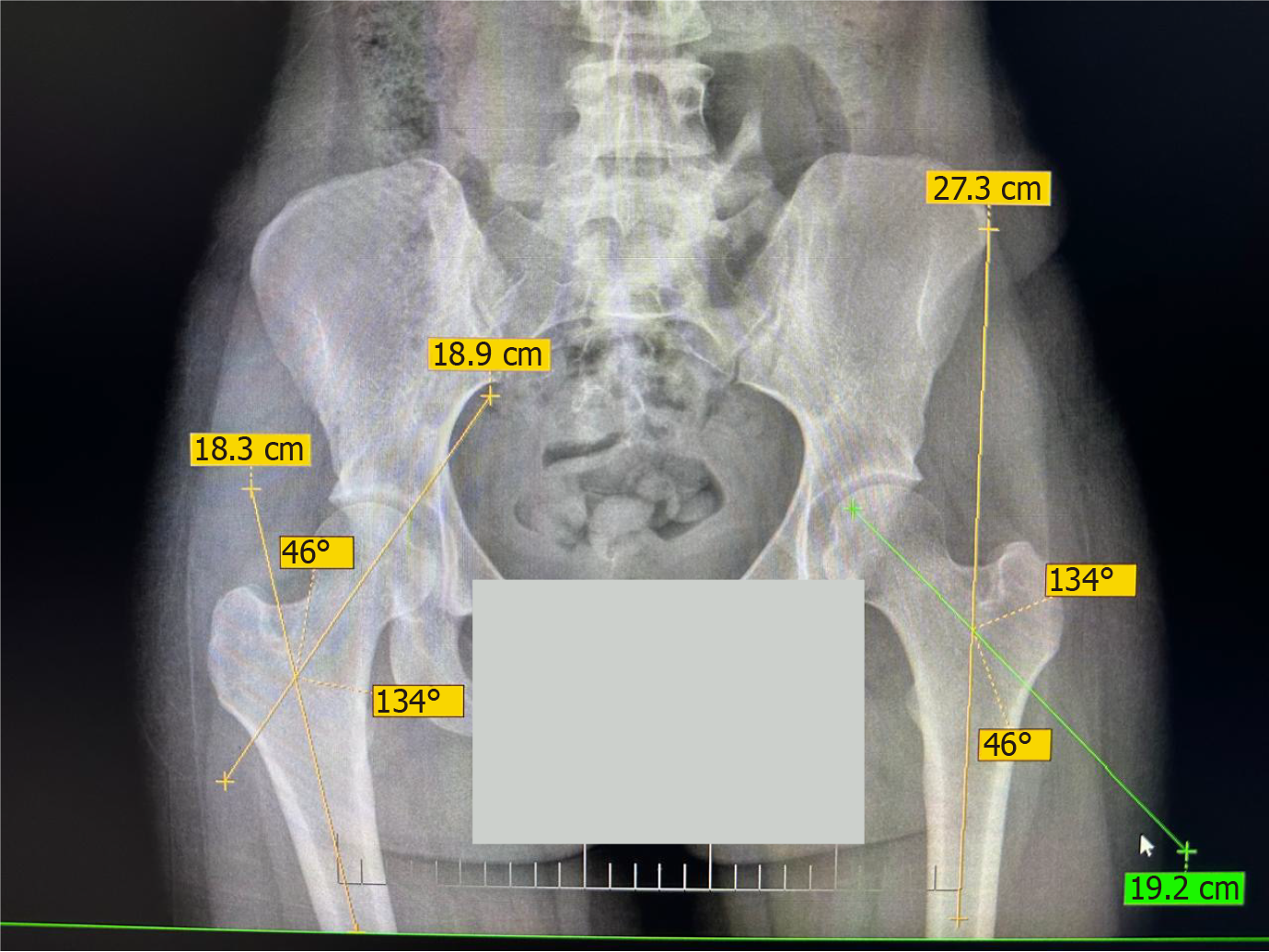
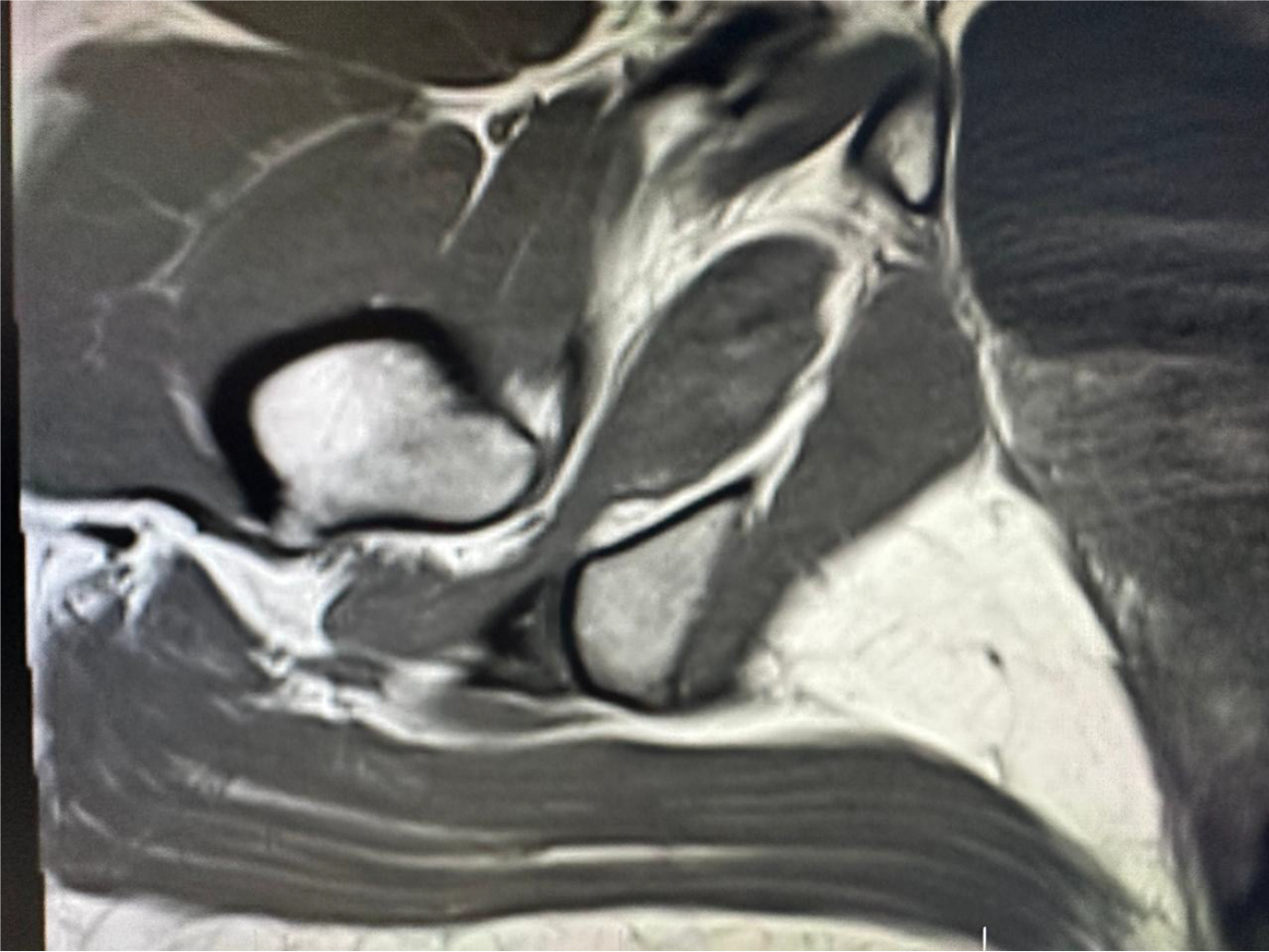
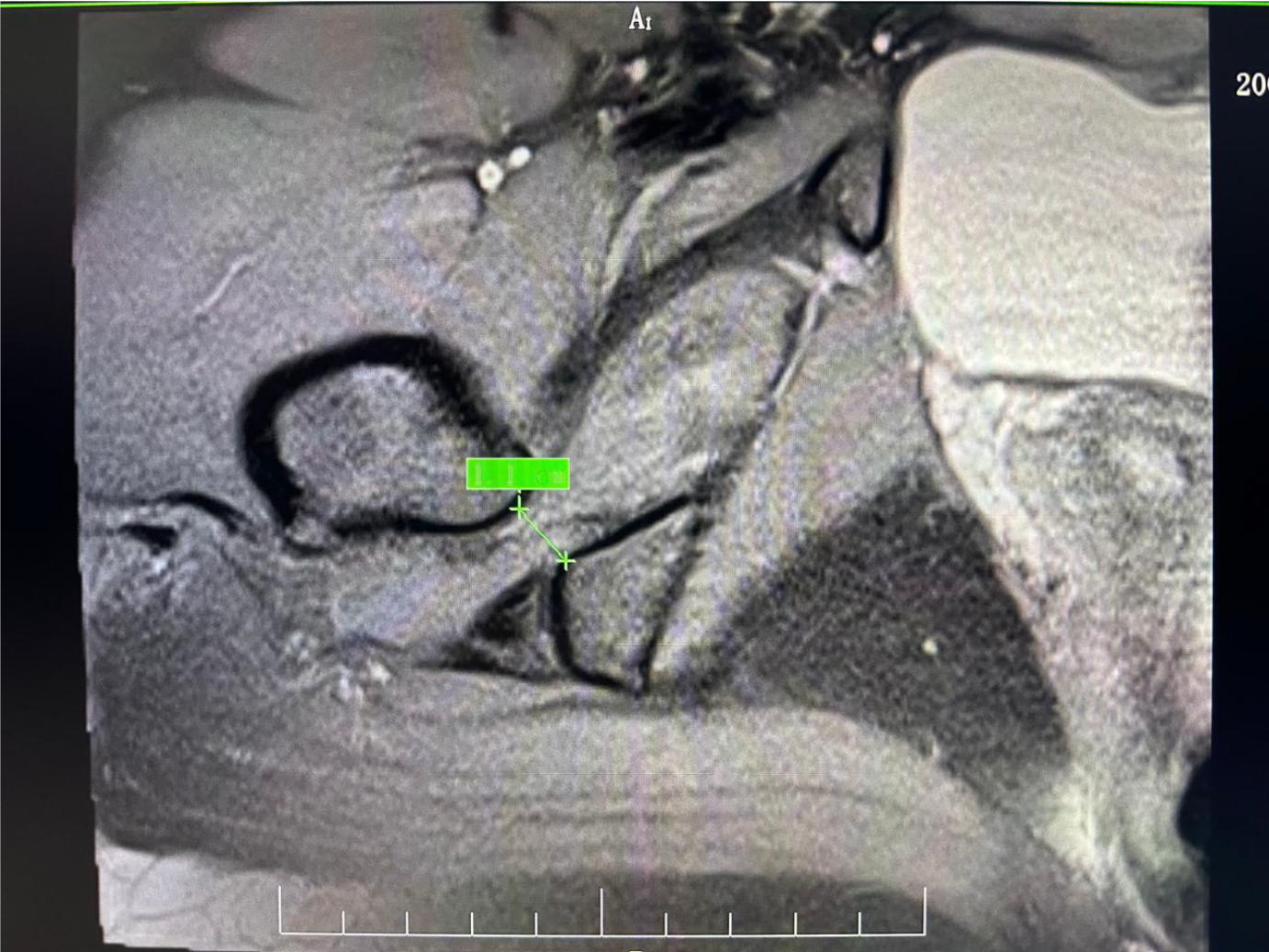
The patient underwent hip X-ray and magnetic resonance imaging (MRI) investigations. Hip X-ray showed no bony or articular changes. Both hips revealed symmetrical joint spaces and valgus alignment with femoral neck-shaft angles of 134° for both right and left hips (Figure 1). MRI revealed a reduced ischiofemoral space (IFS) measuring 11 mm, compared to the normal female value of 17 ± 5 mm, accompanied by muscular oedema (Figures 2 and 3). The MRI also demonstrated a preserved right hip joint alignment with no abnormal bone marrow signal intensity, labral tear, or joint effusion. There was preserved alignment of the bilateral sacroiliac joint with no subchondral bone marrow oedema, synovitis or enthesitis, or joint effusion (Supplementary Figures 1-3).
Consultation with the department of orthopeadics and musculoskeletal radiology.
IFI.
The patient completed an 8-week rehabilitation program with 24 sessions (3 sessions/week) (Table 1). Treatment sessions include:
| Sessions | Procedure |
| 1st session | Case evaluation |
| 2nd–8th sessions | Outpatient physical therapy sessions |
| 9th–24th sessions | telerehabilitation platform sessions |
| Final session | Re-examination |
Stretching exercise: A 3-set of 30 seconds of sustained stretching of the tight external hip rotator muscles was performed during the in-hospital session. Stretch intensity was guided by the patient’s verbal feedback of “mild discomfort”, equivalent to ≤ 2/10 on the numerical pain rating scale (NPRS). Table 1 outlines the management timeline.
Strengthening exercise: Machine-assisted exercises for the hip abductor and external rotator muscles were performed with an initial weight of 40% of her maximum repetition and progressed weekly by 10%. The exercise was prescribed as the following: 3 sets of 10 repetitions for each group of muscles. Resistance bands (TheraBand®) were prescribed for telerehabilitation sessions, with tension levels matched to clinic-based loads using established color-to-weight equivalencies. Strengthening exercise showed a significant improvement in symptoms and function.
Kinesiology tape: Kinesiology tape was applied during each session to activate hip abductors, indirectly increasing the IFS.
Dry needling: Dry needling was applied and directed toward the quadriceps femoris (QF) muscle to decrease its tension. Such a technique is described by Anandkumar.
Tele-rehabilitation: Tele-rehabilitation sessions replicated clinic-based protocols using synchronous video guidance. Challenges included the initial difficulty of assessing resistance band tension remotely, which was mitigated by providing in-session practice demonstrations matching a standardized tension chart. Compliance was monitored via a patient-maintained exercise log verified during clinical sessions.
Following a two-month intervention, the patient demonstrated a substantial reduction in pain, reflected by a significant decrease in the patient’s NPRS score from 9 to 3 points. This outcome signifies a positive clinical response. Additionally, the health-related quality of life had significantly improved according to the Musculoskeletal Health Questionnaire score, which increased from 12 to 48 points. Furthermore, we reexamined the patients using the previous special tests we did at the initial visit. The long stride walking test, IFI test, and Trendelenburg sign were negative.
This report describes detailed clinical features of an IFI case and proposes a tailored and structured rehabilitation program. We showed that a specific physical therapy intervention tailored for this case had significantly decreased the pain and improved the health-related quality of life.
The presented case reported episodes of pain in the right gluteal region with a snapping sensation. This pain extended down the posterior thigh towards the back of the knee. As described in previous reports, which presents with hip pain, snapping, and sciatic nerve irritation are common complaints[6,8]. Unlike previous studies, we used, in this case, a dry needling technique that targeted the quadratus femoris, which plays a key factor in causing the pain associated with IFS. Additionally, we applied a specific taping technique to facilitate the gluteal muscles, especially the gluteus medius.
This study includes a rehabilitation program with first-involved techniques. This specific program combines activity modification with adjustments to reduce strain on the affected area. Exercise, which Includes stretching and streng
Two key physical tests, the long stride walking test and the IFI test, are designed to reproduce typical pain associated with IFS. Gómez-Hoyos et al[8] reported the diagnostic accuracy of long-stride walking at 94% sensitivity and 85% specificity compared to MRI. Further, the IFI test revealed an 82% sensitivity and 85%9. Both were positive in our examination at this initial visit. However, repeating these tests at the end of the rehabilitation program were negative, indicating that the associated features with IFS remarkably improved.
Based on MRI measurements, several studies have established thresholds for normal and affected IFS dimensions. Torriani et al[5] reported average IFS values of 23 ± 8 mm in healthy subjects, compared to 13 ± 5 mm in individuals with IFI. Similarly, Khodair et al[18] found a mean IFS of 20.7 ± 1.4 mm in healthy individuals, respectively, compared to 15 ± 1.8 mm in those with IFI. A study by Bredella et al[10] also demonstrates significantly smaller IFS in patients with IFI compared to controls. We reported comparable findings as a reduction in the IFS. Beyond bone changes, IFI can also affect the quadratus femoris muscle. In Khodair et al's study, various muscle abnormalities were observed, including diffuse oedema (57%), focal oedema (21%), partial tears (14%), and diffuse atrophy (7.2%)[18]. In our study, we observed QF oedema similar to the previous result reported in a study conducted by Khodair et al[18] in patients with IFI syn
This case report demonstrates the clinical efficacy of a structured, tailored and multimodal physical therapy program for managing IFI in a young adult. Key interventions, including targeted strengthening of hip abductor and external rotator muscles, stretching of tight muscles, dry needling for quadratus femoris, and kinesiology taping to facilitate gluteal activation, collectively may contribute to a clinically significant reduction in pain and a substantial improvement in health-related quality of life. Integrating in-person and tele-rehabilitation sessions, a hybrid delivery model ensured continuity of care and mitigating challenges associated with in-person visits. Thus, using a hybrid rehabilitation model supports the feasibility of remote monitoring in musculoskeletal rehabilitation. These findings highlight the importance of addressing biomechanical deficits through personalized rehabilitation programs emphasizing hip stability and neuromuscular re-education. This case is consistent with emerging evidence suggesting that conservative management when tailored to address specific impairments such as muscle weakness and reduced IFS, can result in significant functional recovery and potentially obviate the need for surgical intervention in select IFI cases.
| 1. | Ahuja V, Thapa D, Patial S, Chander A, Ahuja A. Chronic hip pain in adults: Current knowledge and future prospective. J Anaesthesiol Clin Pharmacol. 2020;36:450-457. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | Stafford GH, Villar RN. Ischiofemoral impingement. J Bone Joint Surg Br. 2011;93:1300-1302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 100] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 3. | Taneja AK, Bredella MA, Torriani M. Ischiofemoral impingement. Magn Reson Imaging Clin N Am. 2013;21:65-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 4. | López-Royo MP, Valero-Tena E, Roca M. Anatomical analysis of the pelvis to identify any predisposing anatomical factors for ischiofemoral space pathology: a retrospective study. Br J Radiol. 2020;93:20190556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Torriani M, Souto SC, Thomas BJ, Ouellette H, Bredella MA. Ischiofemoral impingement syndrome: an entity with hip pain and abnormalities of the quadratus femoris muscle. AJR Am J Roentgenol. 2009;193:186-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 207] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 6. | Johnson K. Impingement of the lesser trochanter on the ischial ramus after total hip arthroplasty. Report of three cases. J Bone Joint Surg. 1977;59:268-269. [RCA] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 143] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 7. | Stenhouse G, Kaiser S, Kelley SP, Stimec J. Ischiofemoral Impingement in Children: Imaging With Clinical Correlation. AJR Am J Roentgenol. 2016;206:426-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Gómez-Hoyos J, Khoury A, Schröder R, Johnson E, Palmer IJ, Martin HD. The Hip-Spine Effect: A Biomechanical Study of Ischiofemoral Impingement Effect on Lumbar Facet Joints. Arthroscopy. 2017;33:101-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | Gómez-Hoyos J, Martin RL, Schröder R, Palmer IJ, Martin HD. Accuracy of 2 Clinical Tests for Ischiofemoral Impingement in Patients With Posterior Hip Pain and Endoscopically Confirmed Diagnosis. Arthroscopy. 2016;32:1279-1284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 49] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 10. | Bredella MA, Azevedo DC, Oliveira AL, Simeone FJ, Chang CY, Stubbs AJ, Torriani M. Pelvic morphology in ischiofemoral impingement. Skeletal Radiol. 2015;44:249-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 61] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 11. | Nakano N, Shoman H, Khanduja V. Treatment strategies for ischiofemoral impingement: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2020;28:2772-2787. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 12. | Alsobayel H, Alodaibi F, Albarrati A, Alsalamah N, Alhawas F, Alhowimel A. Does Telerehabilitation Help in Reducing Disability among People with Musculoskeletal Conditions? A Preliminary Study. Int J Environ Res Public Health. 2021;19:72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 13. | Lee S, Kim I, Lee SM, Lee J. Ischiofemoral impingement syndrome. Ann Rehabil Med. 2013;37:143-146. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 14. | Colado JC, Garcia-Masso X, Pellicer M, Alakhdar Y, Benavent J, Cabeza-Ruiz R. A comparison of elastic tubing and isotonic resistance exercises. Int J Sports Med. 2010;31:810-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 62] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 15. | Yanagishita CM, Falótico GG, Rosário DA, Pugina GG, Wever AA, Takata ET. Isthmus femoris impingement--a cause of hip pain: a case report. Rev Bras Ortop. 2012;47:780-783. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Zaworski K, Baj-Korpak J, Kręgiel-Rosiak A, Gawlik K. Effects of Kinesio Taping and Rigid Taping on Gluteus Medius Muscle Activation in Healthy Individuals: A Randomized Controlled Study. Int J Environ Res Public Health. 2022;19:14889. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Anandkumar S. Effect of dry needling on myofascial pain syndrome of the quadratus femoris: A case report. Physiother Theory Pract. 2018;34:157-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Khodair SA, Ghieda UE, Elsayed AS. Ischiofemoral impingement syndrome: Spectrum of MRI findings in comparison to normal subjects. Egypt J Radiol Nucl Med. 2014;45:819-824. [RCA] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |