Published online Mar 26, 2024. doi: 10.12998/wjcc.v12.i9.1698
Peer-review started: January 6, 2024
First decision: January 17, 2024
Revised: February 22, 2024
Accepted: February 28, 2024
Article in press: February 28, 2024
Published online: March 26, 2024
Processing time: 79 Days and 1 Hours
This study aimed to explore the possible etiology and treatment of severe fetal tachycardia in the absence of organic disease and provide a reference for clinical management of severe fetal tachycardia.
A 29-year-old pregnant woman, with a gravidity 1 parity 0, presented with a fetal heart rate (FHR) of 243 beats per minute during a routine antenatal examination at 31 + 2 wk of gestation. Before termination of pregnancy at 38 wk of gestation, the FHR repeatedly showed serious abnormalities, lasting more than 30 min. However, the pregnant woman and the fetus had no clinical symptoms, and repeated examination revealed no organic lesions. The mother and the baby were regularly followed up.
This was a case of severe fetal tachycardia with no organic lesions and mana
Core Tip: Clinical manifestations and obstetric management of this case demonstrated that the abnormal fetal heart rate (FHR) of unknown etiology could be transiently controlled by varying doses of sotalol hydrochloride tablets. However, not all pregnant women experience favorable outcomes. Therefore, the treatment and obstetric management strategies for unexplained FHR abnormalities need investigation.
- Citation: Wang H, Duan RZ, Bai XJ, Zhang BT, Wang J, Song WX. Unexplained fetal tachycardia: A case report. World J Clin Cases 2024; 12(9): 1698-1703
- URL: https://www.wjgnet.com/2307-8960/full/v12/i9/1698.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i9.1698
Fetal arrhythmias are not common in clinical practice, and the probability of their detection during pregnancy is 0.6%–2%, especially unexplained fetal tachycardia. However, once sustained tachycardia occurs in the fetus during pregnancy, it may lead to fetal death, unexplained edema, and premature delivery, seriously threatening the health of the fetus and pregnant woman and requiring active identification and treatment by clinicians. We reported this case of fetal tachycardia (200 beats per minute) and positive outcomes of the mother and the infant after receiving placental therapy. Also, we comprehensively compared various treatment methods for fetal tachycardia in recent years to provide the basis for standardized diagnosis and treatment in the future.
The chief complaints were menopause for 31 + 2 wk and an abnormal fetal heart rate (FHR) for 1 d.
This was a 29-year-old patient with a gravidity 1 parity 0 (G1P0). The patient had regular menstrual cycles, with the last menstrual period on July 11, 2022. The expected date of confinement was April 18, 2023. The patient had no apparent signs of early pregnancy complications. Also, she had no history of radiation exposure or adverse medication use during early pregnancy to protect the fetus. Throughout the pregnancy, no significant abnormalities were observed in nuchal translucency value measurements, Down’s screening results, or four-dimensional color ultrasounds. The oral glucose tolerance test results indicated higher fasting blood glucose levels than normal, leading to a diagnosis of gestational diabetes. Symptomatic treatment was provided through dietary adjustments and appropriate exercise; however, blood glucose monitoring in later stages was not reported. The patient had no complaints of dizziness, blurred vision, or palpitations during pregnancy. At 31 + 2 wk of gestation, the fluctuations in FHR were detected during an outpatient visit. The patient was mentally and emotionally stable throughout her pregnancy without any sleep disturbances or changes in appetite. She did not experience fever or chills nor exhibited symptoms such as coughing or production of sputum. The weight gain was approximately 20 kg while maintaining normal bowel movements and urine output without discomfort related to excessive drinking/eating/urination patterns observed by the patient herself. The blood pressure readings were within normal range throughout this period.
The patient was previously healthy. She had normal body temperature and no history of pregnancy anemia, abnormal thyroid function, or arrhythmia.
The patient denied any family history of malignancy.
On physical examination, the vital signs were as follows: Body temperature: 36 ℃; blood pressure: 152/88 mmHg; heart rate: 100 bpm; and respiratory rate: 20 breaths per minute. The other system examinations revealed no abnormalities.
No abnormality was detected in routine blood and urine analyses.
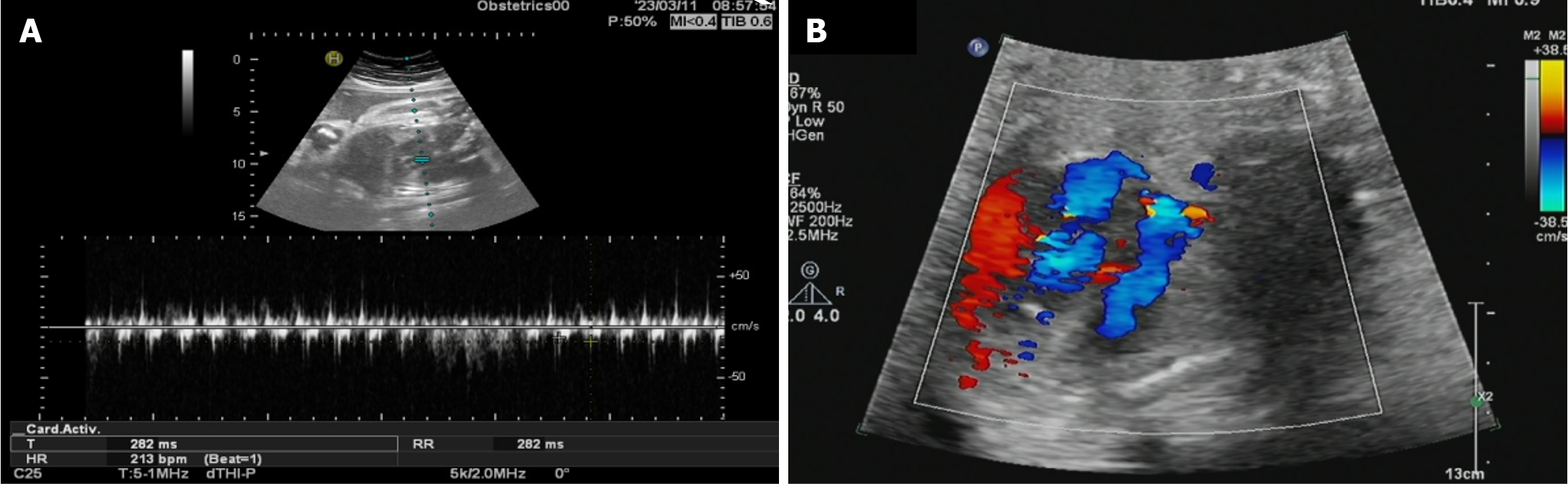
The obstetric ultrasound (February 25, 2023) revealed the following: (1) Intrauterine pregnancy single live fetus (cephalic, ultrasound gestational age about 32 WLD); (2) anterior placenta; (3) appropriate amniotic fluid; and (4) fetal tachycardia. Further examination was recommended. The obstetrical color ultrasound detected the FHR of 243 bpm. The fetal heart color ultrasound further confirmed the FHR of 243 bpm, and fetal cardiac structure showed no obvious abnormalities (Figure 1).
The final diagnosis was as follows: Abnormal fetal heart monitoring (fetal distress?), 31 + 2 wk G1P0, gestational diabetes, surgical history of teratoma, and pregnancy combined with obesity.
The possibility of fetal distress could not be ruled out. The patient was admitted to the hospital to receive symptomatic treatment such as oxygen inhalation, continuous fetal heart monitoring, fetal lung maturity promotion, and labetalol 100 mg po q8h. During hospitalization, the FHR reached 230–270 bpm. The patient’s vital signs were stable, without palpitation, abdominal distension, and vaginal water and bleeding. After referral to a higher-level hospital, sotalol hydrochloride tablets were given at a dose of 80 mg twice a day first, which was increased to 160 mg twice a day 3 d later. The patient was pregnant (33 + 6 wk), and the FHR was 133 bpm. The obstetric color ultrasound was performed at 34 + 6 wk of gestation, and the FHR was 213 bpm. The fetal heart color ultrasound was performed, revealing fetal tachycardia (FHR 231 bpm). No obvious abnormalities were found in the fetal cardiac structure (Figure 2). The dose of sotalol hydrochloride tablets was adjusted to 240 mg twice a day. The FHR was 143 bpm at 35 + 6 wk.
The pregnancy was terminated at 38 wk of gestation. The newborn weighed 3300 g. No arrhythmia was found in the pregnant woman or the newborn until 4 wk after delivery.
If fetal tachycardia occurs, the cause should be actively sought. Most cases of fetal tachycardia have a heart rate of less than 200 bpm, which usually does not require treatment but requires close follow-up[1,2]. Approximately 10%–20% of cases of fetal tachycardia require referral to a fetal cardiologist for further evaluation, and persistent fetal tachycardia with congestive cardiac dysfunction or fetal edema requires intrauterine or postpartum treatment[3,4]. One report of FHR > 224 bpm indicated that the persistence of fetal tachycardia was not necessarily caused by fetal hypoxia, and the heart rate was controlled by metoprolol treatment after transfer to a higher-grade hospital[5]. Another study indicated that fetuses without sustained tachycardia and without edema were usually treated with expectation, and the natural course of development was good. The fetus with nonedematous persistent tachycardia had a good effect of drug therapy on conversion, whereas the fetus with severe edema had a poor effect of drug therapy[6]. However, Strasburger et al[7] pointed out that fetal arrhythmias were usually managed during the second or third trimester of pregnancy, and it was emphasized that fetal echocardiography and magnetocardiography were the two primary means of diagnosing fetal arrhythmias. Transient or hidden arrhythmias, such as bundle branch block, long QT syndrome, and tip torsion, may lead to cardiomyopathy and sudden unexplained fetal death, and may also require medications. Therefore, no matter whether fetal tachycardia is benign or not, it may cause fetal edema or cardiac insufficiency. Recent studies have reported that prenatal maternal administration of digoxin, flucaine, sotalol, and amiodarone can control fetal tachycardia, but these drugs may cause serious adverse reactions. Therefore, currently, the standardized treatment for fetal tachyarrhythmia has not been established in clinical practice. It requires multi-institutional evaluation and follow-up, followed by determination and adjustment of initial treatment and dose, while considering pharmacokinetic factors, and close monitoring of maternal adverse reactions. A study on the prenatal treatment of supraventricular fetal arrhythmias indicated that tachyarrhythmia might still recur in the first 2 wk after birth[8].
Fetal tachycardia is a type of fetal arrhythmia. The FHR in the present case was severely abnormal, with intermittent repeated attacks of 230–270 bpm, lasting from several hours to several days. This was an extremely rare and severe fetal tachycardia. The case was actively referred to a higher-level hospital after discovery. After the oral administration of sotalol (32–38 wk of gestation), FHR was initially controlled. Despite an occasional increase in FHR, the fetal outcome was good. In recent years, the diagnosis of fetal tachycardia basically relies on continuous fetal heart monitoring chart and fetal heart color ultrasound to preliminarily exclude fetal organic lesions, and the management of fetal tachycardia is still in the stage of empirical research. Li Xiulan reported a case of FHR of 227–242 bpm, with biphase blood flow in the foramen ovale. Oral digoxin treatment was given considering the possibility of abnormal cardiac conduction in the fetus. The FHR returned to normal on the fourth day of medication, and the foramen ovale returned to normal after treatment[9]. Munoz et al[10] provided a unique treatment method: Intrauterine intramuscular injection of digoxin alleviated refractory fetal supraventricular tachycardia accompanied by fetal edema, which could be completely resolved by one-time injection. Yuan et al[11] administered sotalol orally to 10 mothers with fetal tachycardia (atrial fibrillation) for 7 d. Eight of these mothers had a conversion back to normal sinus rhythm, and one died after the dosage was increased. This indicated that sotalol was more efficient in treating fetal atrial fibrillation but less effective for other arrhythmias, especially for the fetus with supraventricular tachycardia, where the fatality rate was higher[12]. However, Purkayastha et al[13] pointed out that the management of fetal supraventricular tachycardia with flucanide or sotalol as monotherapy or in combination with digoxin might be the main approach, but this needs to be further evaluated in a practical setting. O'Leary et al[14] examined 57 cases of fetal persistent tachycardia at 13–37 wk under the control of digoxin, flucanide, sotalol, and amiodarone. They showed that the risk of fetal death in the uterus was minimal after placental therapy for persistent fetal tachycardia with normal cardiac structure. In another multicenter analysis of the prenatal treatment of 49 cases of supraventricular tachycardia, 44 cases of fetal tachyarrhythmias were controlled after treatment with digoxin, sotalol, and flucanide. One mother and four fetuses experienced severe adverse events (two of which were fetal death mainly due to heart failure), and tachyarrhythmia occurred in 15 neonates within 2 wk after birth[15]. Refaat et al[15] reported two cases of persistent fetal supraventricular tachycardia: One case was treated with flucanica–sotalol and the other with sotalol–digoxin, which effectively controlled fetal tachycardia, laying a foundation for the empirical treatment of first and second-line drugs. In the present case, severe fetal tachycardia was detected in a routine birth examination. No obvious abnormality was found in fetal cardiac color Doppler ultrasound, maternal electrocardiogram, maternal cardiac color Doppler ultrasound, and other examination results. Subsequent birth examination revealed multiple fetal tachycardia, and the maternal fetal outcome was good after sotalol treatment. In this case, although the fetus had no organic disease, the long-term rapid heart rate of the fetus increased the risk of fetal heart failure, intrauterine distress, and even intrauterine death. The symptoms were relieved after systematic treatment, and no obvious complications were found after the outcome of childbirth. When similar cases are encountered clinically, we should actively intervene and follow up closely. This approach holds positive significance for the health of both pregnant women and fetuses. However, the limitation of the present case was that the choice of drugs, initial dosing, and so forth for the management of unexplained fetal arrhythmia remained unclear.
The management of FHR abnormalities aims at reducing fetal hypoxia and improving fetal prognosis. When the cause of the abnormal FHR cannot be determined or no significant improvement is found in the FHR after conservative treatment, preparation for pregnancy termination should be done at the same time. For unexplained severe fetal tachycardia, only maternal factors can be excluded in clinical practice. At the same time, fetal heart color ultrasound is used to evaluate fetal heart structure abnormalities, edema, and fetal movement. During this period, only fetal heart monitoring is performed, and the mother and the child are observed to determine the next treatment. This case report discussed the clinical diagnosis and treatment of severe fetal tachycardia without organic lesions to provide a relevant basis for the standardized treatment of severe fetal tachycardia, ultimately reducing the perinatal adverse outcome rate for infants.
Thanks for the patient’s consent and cooperation in the follow-up. I would like to give my heartfelt thanks to all the people who have ever helped me in this paper.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tangsuwanaruk T, Thailand S-Editor: Zhang L L-Editor: A P-Editor: Chen YX
| 1. | Malhamé I, Gandhi C, Tarabulsi G, Esposito M, Lombardi K, Chu A, Chen KK. Maternal monitoring and safety considerations during antiarrhythmic treatment for fetal supraventricular tachycardia. Obstet Med. 2019;12:66-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 2. | Yuan SM. Fetal arrhythmias: Surveillance and management. Hellenic J Cardiol. 2019;60:72-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 3. | Katsura D, Tsuji S, Tokoro S, Hoshiyama T, Hoshino S, Furukawa O, Murakami T. Atypical fetal junctional ectopic tachycardia: A case report and literature review. BMC Pregnancy Childbirth. 2022;22:311. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Wacker-Gussmann A, Strasburger JF, Cuneo BF, Wakai RT. Diagnosis and treatment of fetal arrhythmia. Am J Perinatol. 2014;31:617-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 63] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 5. | Shi C, Wang F, Tong A, Zhang XQ, Song HM, Liu ZY, Lyu W, Liu YH, Xia WB. NFKB2 mutation in common variable immunodeficiency and isolated adrenocorticotropic hormone deficiency: A case report and review of literature. Medicine (Baltimore). 2016;95:e5081. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 48] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 6. | Hepatic Surgery Group; Surgery Branch of Chinese Medical Association; Digital Medical Branch of Chinese Medical Association; Digital Intelligent Surgery Committee of Chinese Research Hospital Association; Liver Cancer Committee of Chinese Medical Doctor Association. [Chinese expert consensus on laparoscopic hepatic segmentectomy and subsegmentectomy navigated by augmented and mixed reality technology combined with indocyanine green fluorescence(2023)]. Zhonghua Wai Ke Za Zhi. 2023;61:929-936. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Strasburger JF, Eckstein G, Butler M, Noffke P, Wacker-Gussmann A. Fetal Arrhythmia Diagnosis and Pharmacologic Management. J Clin Pharmacol. 2022;62 Suppl 1:S53-S66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 8. | Miyoshi T, Maeno Y, Hamasaki T, Inamura N, Yasukochi S, Kawataki M, Horigome H, Yoda H, Taketazu M, Nii M, Hagiwara A, Kato H, Shimizu W, Shiraishi I, Sakaguchi H, Ueda K, Katsuragi S, Yamamoto H, Sago H, Ikeda T; Japan Fetal Arrhythmia Group. Antenatal Therapy for Fetal Supraventricular Tachyarrhythmias: Multicenter Trial. J Am Coll Cardiol. 2019;74:874-885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 50] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 9. | Mills M. Treatment of fetal supraventricular tachycardia with flecainide acetate after digoxin failure. Am J Obstet Gynecol. 1992;166:1863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 10. | Munoz JL, Lewis AL, Song J, Ramsey PS. Fetal Intervention for Refractory Supraventricular Tachycardia Complicated by Hydrops Fetalis. Case Rep Obstet Gynecol. 2022;2022:5148250. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Yuan ZM. Treatment of fetal arrhythmia with sotalol. Xin Yi Xue. 2001;02:110. [DOI] [Full Text] |
| 12. | Oudijk MA, Michon MM, Kleinman CS, Kapusta L, Stoutenbeek P, Visser GH, Meijboom EJ. Sotalol in the treatment of fetal dysrhythmias. Circulation. 2000;101:2721-2726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 91] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 13. | Purkayastha S, Weinreich M, Fontes JD, Lau JF, Wolfe DS, Bortnick AE. Fetal Supraventricular Tachycardia: What the Adult Cardiologist Needs to Know. Cardiol Rev. 2022;30:31-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | O'Leary ET, Alexander ME, Bezzerides VJ, Drogosz M, Economy KE, Friedman KG, Pickard SS, Tworetzky W, Mah DY. Low mortality in fetal supraventricular tachycardia: Outcomes in a 30-year single-institution experience. J Cardiovasc Electrophysiol. 2020;31:1105-1113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 15. | Refaat M, El Dick J, Sabra M, Bitar F, Tayeh C, Abutaqa M, Arabi M. Sotalol as an effective adjunct therapy in the management of supraventricular tachycardia induced fetal hydrops fetalis. J Neonatal Perinatal Med. 2020;13:267-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |