Published online Mar 16, 2024. doi: 10.12998/wjcc.v12.i8.1504
Peer-review started: December 8, 2023
First decision: January 15, 2024
Revised: January 19, 2024
Accepted: February 25, 2024
Article in press: February 25, 2024
Published online: March 16, 2024
Processing time: 94 Days and 8.4 Hours
Congenital enteric duplication cysts are tubular or cystic structures that normally lie alongside the gastrointestinal (GI) tract. Enteric duplication cysts are typically solitary lesions that occur anywhere near the GI tract from the neck to the rectum, but having multiple duplication cysts is rare, and presentation within the pancreas is extremely rare.
We herein demonstrate a case of esophageal, gastric, and gastric-type duplication cyst of the pancreas in a seventeen-month-old girl who presented with failure to thrive, abdominal pain, vomiting, hematemesis, and melena since the age of three months. The cysts were excised by thoracoscopy and laparoscopy in the same setting. To our knowledge, no such case has been published.
Enteric duplications can occur throughout the entire alimentary tract. When they occur in the pancreas, they present a formidable challenge in both diagnosis and treatment. Due to the risk of complications and malignant transformation, surgical removal is the recommended treatment of all duplication cysts.
Core Tip: Gastrointestinal duplications are infrequent developmental abnormalities that can manifest diversely, including variations in presentation, size, location, and symptoms. The occurrence of multiple enteric duplication cysts is uncommon, and their presence within the pancreas is exceptionally rare. This case evolved of esophageal, gastric, and gastric-type duplication cyst of the pancreas in a 17-month-old girl who was managed surgically by thoracoscopy and laparoscopy in the same setting.
- Citation: Alsinan TA, Altokhais TI. Multiple thoracic and abdominal foregut duplication cysts: A case report. World J Clin Cases 2024; 12(8): 1504-1509
- URL: https://www.wjgnet.com/2307-8960/full/v12/i8/1504.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i8.1504
Gastrointestinal (GI) duplications are infrequent developmental abnormalities that can manifest diversely, including variations in presentation, size, location, and symptoms[1]. Initially referred to as GI duplications, these malformations were first introduced by Ladd[2]. Gastric duplication cysts (GDCs) represent 2%-7% of all alimentary tract duplications[3]. The clinical presentation of GDCs depends on their size and position[4]. GDCs are commonly situated along the greater curvature of the stomach and typically lack any connection with the gastric lumen[3]. This study presents a rare case of multiple foregut duplication cysts.
A 17-month-old girl was admitted for recurrent abdominal pain and vomiting, followed by hematemesis and melena since she was 3 months old.
On admission, she was afebrile. On physical examination, she had a weight of 9 kg. She was pale but not jaundiced.
Unremarkable.
No remarkable family history and no similar history in the family.
The child’s weight was 9 kg (below 25th percentile for age). She was pale but not jaundiced. The rest of the examination was unremarkable.
The blood test showed a picture of anemia with a hemoglobin level of 6.6 g/dL. Her liver and pancreatic enzymes were normal.
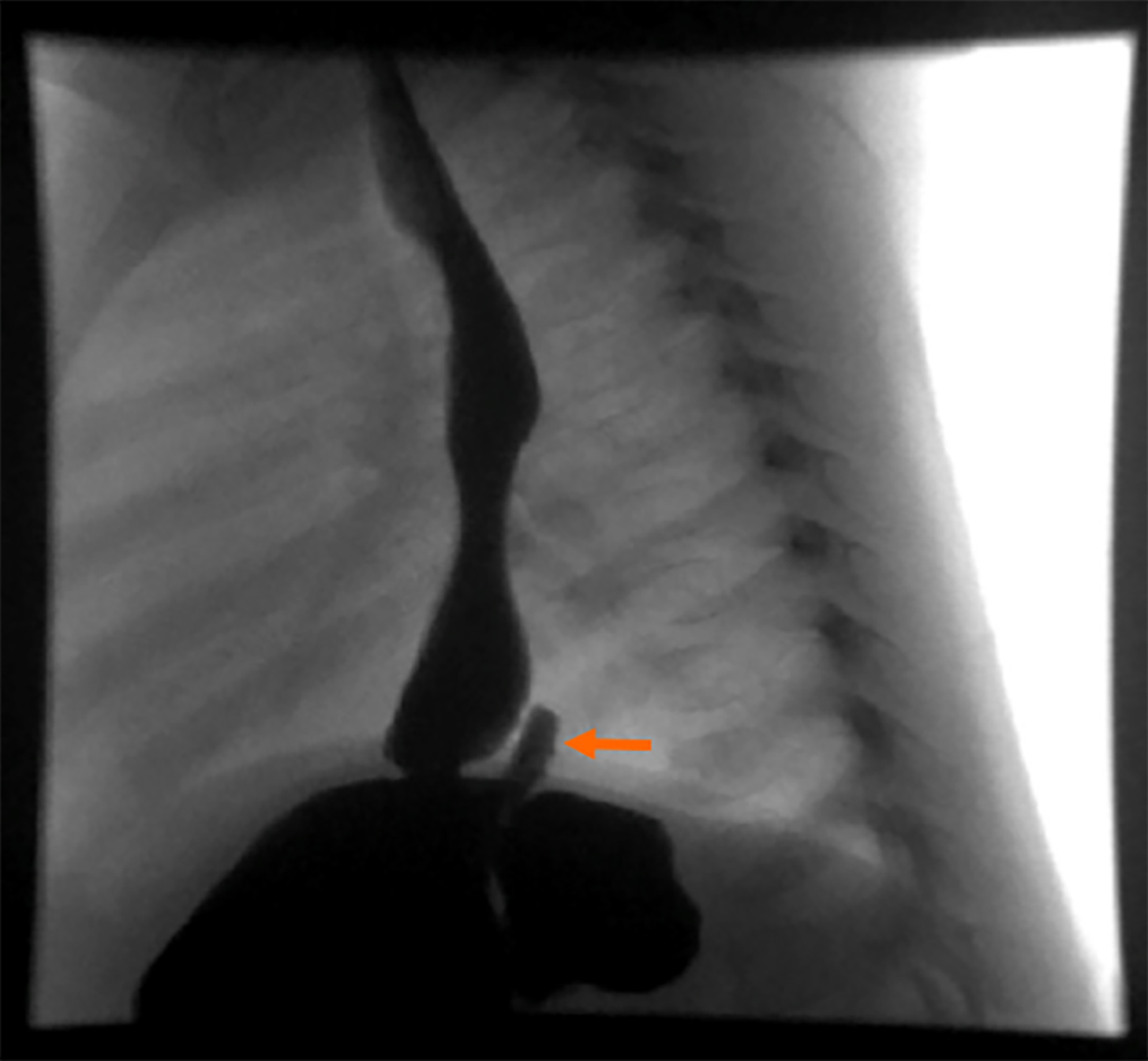
Imaging studies revealed a cystic mass on the mid-esophagus that was not communicated with the esophagus (Figure 1). Another mass located at the diaphragm hiatus with communication with the fundus of the stomach (Figure 2).
The child underwent thoracoscopy and excision of the esophageal cyst, which was not communicating with the esophagus, then laparoscopy and excision of the gastric fundal cyst, which was communicating with the stomach. After the excision of the gastric fundal cyst, a diagnostic laparoscopy was done to rule out other cysts.
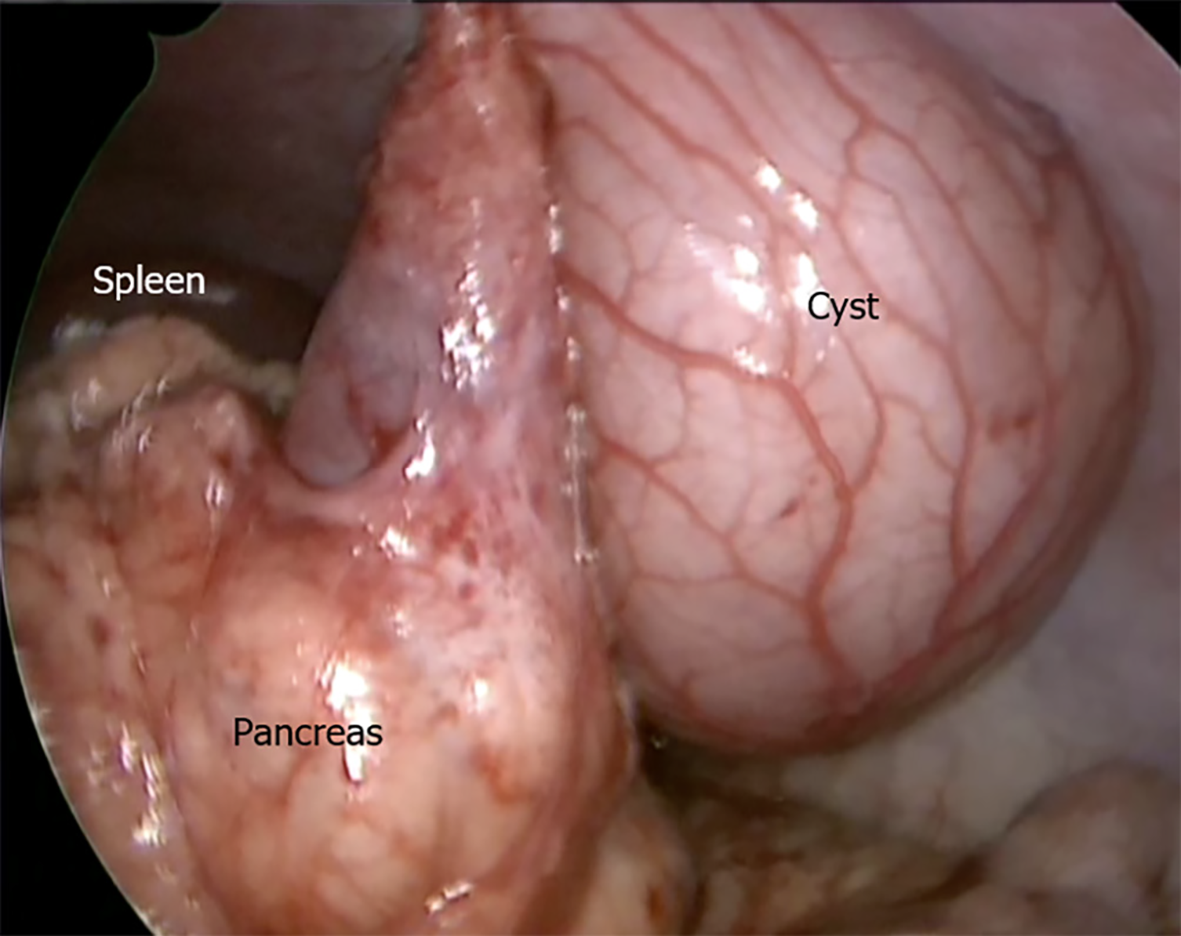
The bowel was run from the duodenojejunal junction to the rectum and an incidental cyst was found originating from the body of the pancreas with no attachment to the stomach (Figure 3).
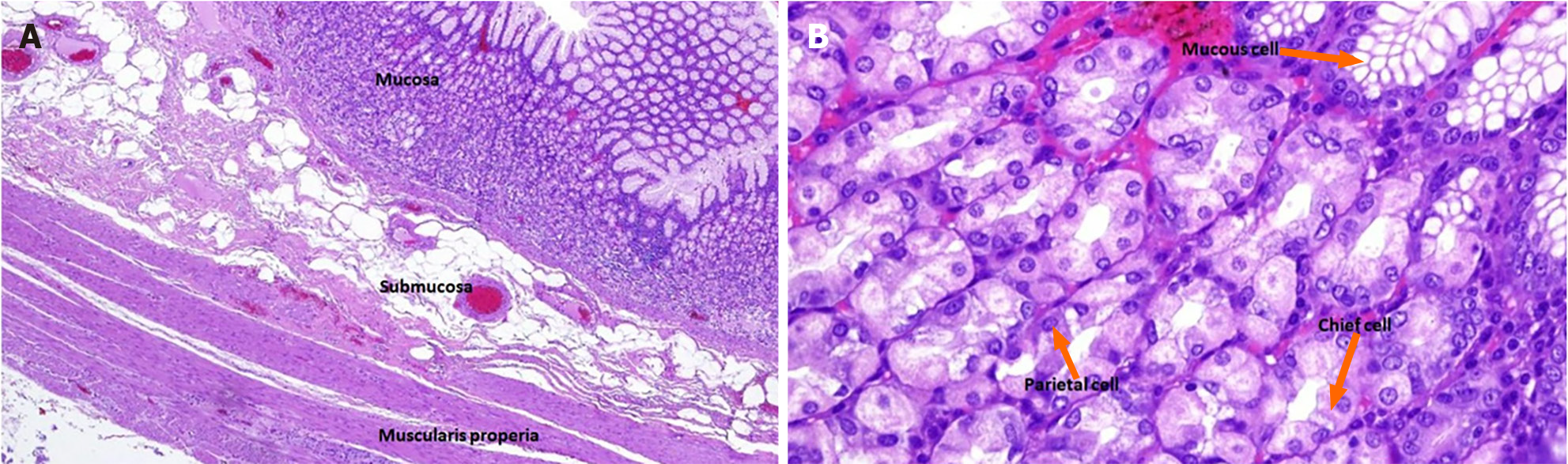
Upon microscopic examination, esophageal and gastric fundal lesions were bronchogenic-type cysts. Low power of the pancreatic cyst showed all the layers of a normal stomach namely, mucosa, submucosa, and muscularis propria. The mucosa composition primarily exhibited gastric body characteristics, encompassing parietal, chief, and mucus cells (Figure 4). The findings were consistent with gastric duplication cyst.
The findings were consistent with GDC. The child had an uneventful post-operative course.
Surgical excision of the cyst.
She gained weight and reached 13.5 kg at two years old (at 75th percentile for age). Her weight remained within the 75th percentile for age, and the resolution of her symptoms was confirmed during the follow-up five years later.
GI duplications are relatively rare abnormalities that can occur at various locations along the digestive system, ranging from the mouth to the rectum. The most common site for these duplications is the ileum. They have been referred to by different names, including enterocystomas, enterogenous cysts, supernumerary accessory organs, ileum duplex, giant diverticula, and unusual Meckel’s diverticula. Among all types of duplications, GDCs are the least frequently encountered, accounting for approximately 2%-7% of GI duplications. They typically present with symptoms such as GI obstruction, ulceration, and painless bleeding, often observed in early childhood. GDCs are commonly situated along the greater curvature of the stomach and typically lack any connection with the gastric lumen[5].
Duplications are frequently diagnosed incidentally, although most patients experience a combination of pain and obstructive symptoms. These symptoms can arise from either the distention of the duplication itself or the compression of neighboring organs and blood vessels. Obstructive manifestations of gastric duplications often include postprandial epigastric pain, discomfort, nausea, vomiting, and the presence of an abdominal mass. Rare presentations may include hematemesis, GI bleeding, recurrent pancreatitis, and perforation leading to peritonitis[6,7]. In our case, the patient presented with abdominal pain, vomiting, and GI bleeding. Malignancies originating from duplication cysts often tend to be diagnosed at advanced stages due to their atypical symptoms and challenging diagnostic processes[3].
Pancreatic-associated enteric duplications are exceptionally rare and can exhibit distinct clinical characteristics, including severe pancreatitis. These cysts present unique surgical complexities, and their diagnosis can be challenging, often leading to confusion with pancreatic pseudocysts or neoplasms. Diagnostic imaging techniques such as abdominal ultrasound, contrast GI studies, computed tomography scans, and magnetic resonance imaging play a crucial role in identifying these cysts. In our case, the cyst was unexpectedly discovered during surgery and was not detected through radiological examinations.
The necessary macroscopic and microscopic criteria for diagnosing a GDC are as follows: (1) The cyst’s wall is connected to the stomach wall; (2) the cyst is enveloped by smooth muscle that seamlessly transitions into the stomach’s muscle layer; and (3) the cyst wall is lined with epithelium derived from gastric or other types of GI mucosa. In our current cases, these criteria were met, effectively ruling out alternative diagnoses[8].
Surgical removal is the recommended treatment for all duplication cysts due to the risk of complications and potential malignant transformation. The approach depends on the location of the cyst, its relation to adjacent organs and vessels[5]. Holcomb et al[9], provided guidelines for managing duplication cysts based on factors such as the patient’s age and condition, lesion location, communication with the intestinal lumen, and the extent of the anatomical involvement. During cyst excision, it is crucial to prioritize the protection of vital structures like bile ducts and vessels. Non-communicating GDCs are typically treated by completely removing the cyst and resecting the shared wall between the stomach and the duplication cyst. Asymptomatic communicating GDCs generally do not require intervention if both gastric lumens are open[10].
Enteric duplications occur throughout the entire alimentary tract. Cases involving the pancreas are challenging in terms of diagnosis and treatment. Due to the risk of complications and malignant transformation, surgical removal is the recommended treatment for all duplication cysts.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Saudi Arabia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Liu T, China S-Editor: Luo ML L-Editor: A P-Editor: Yu HG
| 1. | Yang MC, Duh YC, Lai HS, Chen WJ, Chen CC, Hung WT. Alimentary tract duplications. J Formos Med Assoc. 1996;95:406-409. [PubMed] |
| 2. | Ladd WE. Duplications of the alimentary tract. South Med J. 1937;30:363-371. |
| 3. | Johnston J, Wheatley GH 3rd, El Sayed HF, Marsh WB, Ellison EC, Bloomston M. Gastric duplication cysts expressing carcinoembryonic antigen mimicking cystic pancreatic neoplasms in two adults. Am Surg. 2008;74: 91-94. [PubMed] |
| 4. | Berrocal T, Torres I, Gutiérrez J, Prieto C, del Hoyo ML, Lamas M. Congenital anomalies of the upper gastrointestinal tract. Radiographics. 1999;19:855-872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 61] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Besner GE. Alimentary tract duplications [Internet]. [cited May 1, 2012]. Available from: http://emedicine.medscape.Com/article/933427-overview. |
| 6. | Master V, Woods RH, Morris LL, Freeman J. Gastric duplication cyst causing gastric outlet obstruction. Pediatr Radiol. 2004;34:574-576. [PubMed] |
| 7. | Oak SN, Kumar S, Joshi M, Vishwanath N, Akhtar T. Neonatal lingual gastric duplication cyst: A rare case report. J Indian Assoc Pediatr Surg. 2006;11:97-98. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Mardi K, Kaushal V, Gupta S. Foregut duplication cysts of stomach masquerading as leiomyoma. Indian J Pathol Microbiol. 2010;53:160-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Holcomb GW 3rd, Gheissari A, O'Neill JA Jr, Shorter NA, Bishop HC. Surgical management of alimentary tract duplications. Ann Surg. 1989;209:167-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 199] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 10. | D'Journo XB, Moutardier V, Turrini O, Guiramand J, Lelong B, Pesenti C, Monges G, Giovannini M, Delpero JR. Gastric duplication in an adult mimicking mucinous cystadenoma of the pancreas. J Clin Pathol. 2004;57:1215-1218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 50] [Article Influence: 2.4] [Reference Citation Analysis (0)] |