Published online Feb 26, 2024. doi: 10.12998/wjcc.v12.i6.1169
Peer-review started: November 13, 2023
First decision: January 9, 2024
Revised: January 12, 2024
Accepted: February 2, 2024
Article in press: February 2, 2024
Published online: February 26, 2024
Processing time: 98 Days and 11.4 Hours
Gigantic epidermal cysts (GECs) are rare benign skin appendicular tumours also known as keratinocysts. GECs have a high incidence and their wall is made up of epidermis. Epidermal cysts can occur in any part of the skin; clinical manifesta
Herein, we report a case involving a 56-year-old female with a GEC in the occi
Epidermal cysts are common cystic nodules on the surface of the body, the ae
Core Tip: The clinical manifestations of epidermal cysts are varied and the misdiagnosis rate is high. The disease occurs mostly in the head, face and upper torso of young men. Most patients usually have no symptoms, but epidermal cysts that are gigantic or located in important organs can press on the surrounding tissue structure and produce corresponding symptoms. However, gigantic epidermal cysts occurring in the occipital part of the brain in female patients are relatively rare. This report aims to strengthen the understanding of the disease and improve the accuracy of clinical diagnosis.
- Citation: Wei Y, Chen P, Wu H. Gigantic occipital epidermal cyst in a 56-year-old female: A case report. World J Clin Cases 2024; 12(6): 1169-1173
- URL: https://www.wjgnet.com/2307-8960/full/v12/i6/1169.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i6.1169
Epidermal cysts are among the most common benign skin tumours, but very few epidermal cysts can be secondary to malignant tumours, such as basal cell carcinoma and squamous cell carcinoma[1,2]. Epidermal cysts can occur in any part of the body, mainly under the skin, mostly in the head, face and upper torso of young men, and a small number of cysts can occur in the injured region or in deep tissues and organs, such as the cranium, abdominal cavity, mammary gland, etc. Epidermal cysts occur more than a single time; are multiple rare, usually asymptomatic, have a large volume or are located in important organs and can compress the surrounding tissue structure and produce corresponding symptoms. Most patients are treated because of secondary infection resulting in a rapid increase in volume, severe pain, and rupture.
Occipital phyma for 20 years.
The patient was found to have developed occipital phyma more than 20 years ago, without redness, swelling, or rupture, and no diagnosis or treatment was given. Recently, the patient self-reported that the scalp mass was larger than before without rupture; therefore, she came to the Department of Neurosurgery, the Second Affiliated Hospital of Xi’an Medical University for treatment.
The patient had a history of diabetes, heart disease, hypertension, hepatitis, tuberculosis and other infectious diseases; a history of trauma and surgery; and a history of drug allergy.
There was no family history of genetic disease.
The vital signs were as follows: Body temperature, 36.2 °C; blood pressure, 120/82 mmHg; heart rate, 79 beats per min; and respiratory rate, 17 breaths per min.
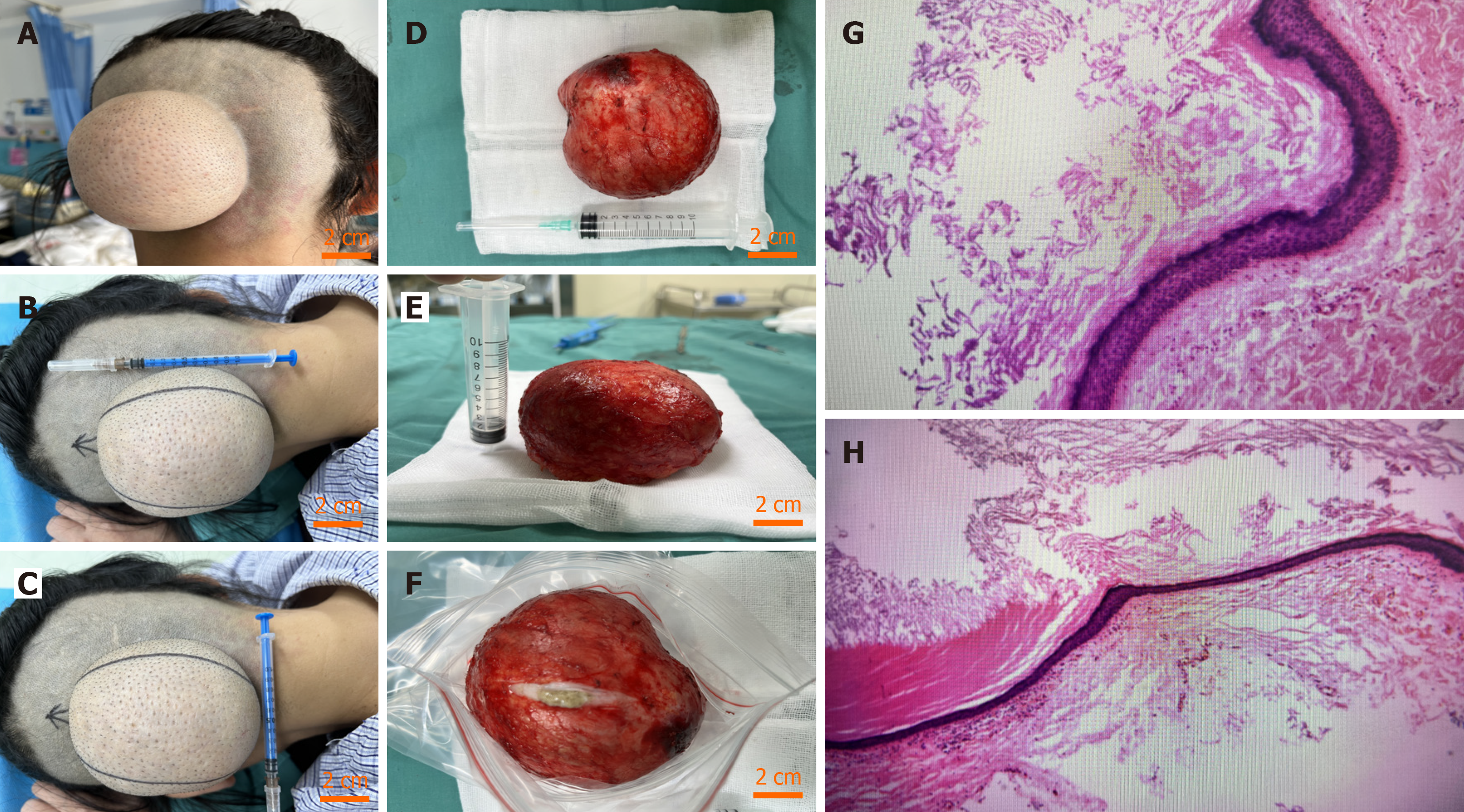
The physical examination revealed a 77 mm × 44 mm mass on the occipitalia with a clear border, tough texture, good mobility, and tenderness. The transillumination test was negative. There was no red or swollen skin or ulceration (Figure 1A-C).
There were no abnormalities in routine blood test results, blood biochemistry results, blood coagulation function, or routine stool or urine test results.
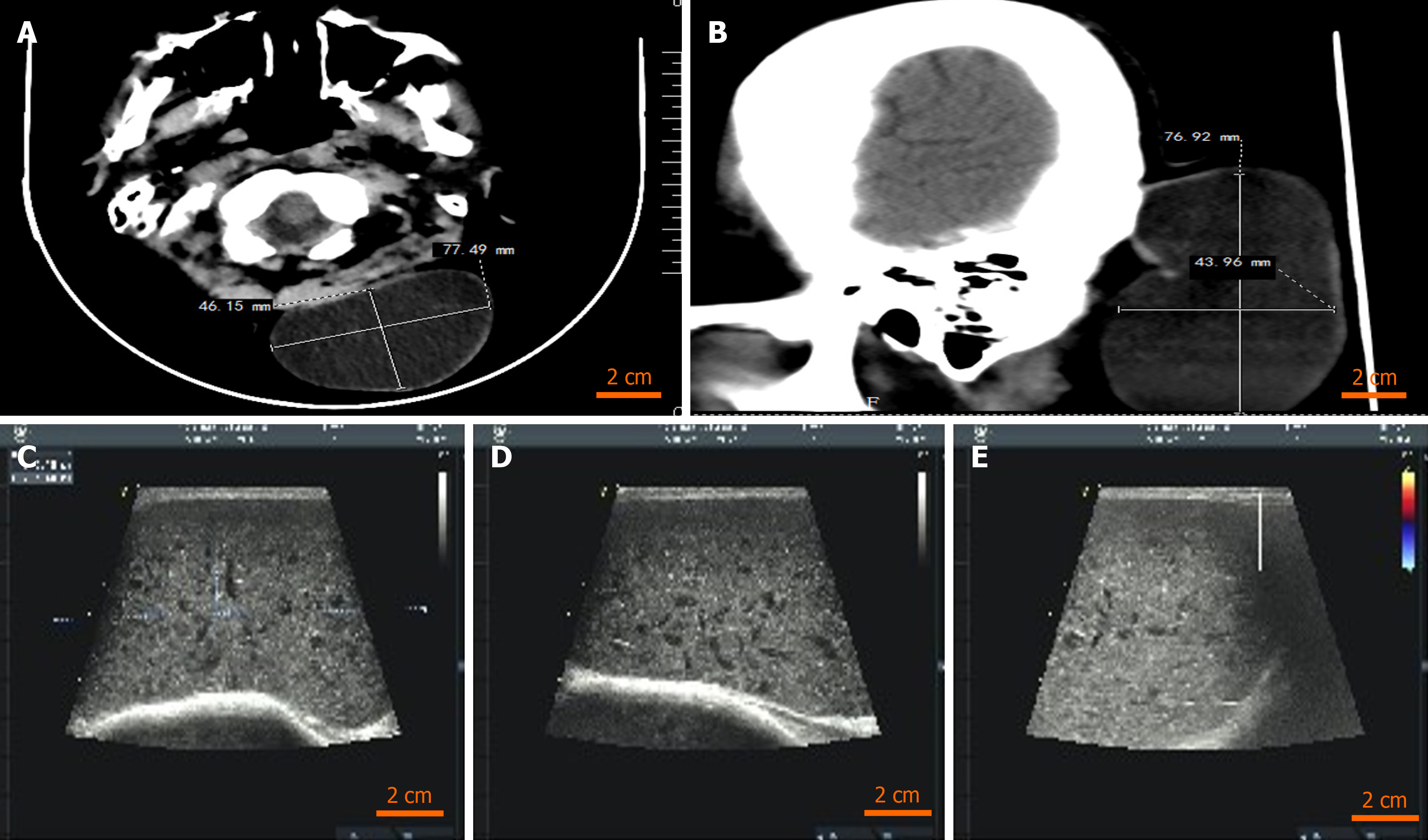
Craniocerebral computed tomography revealed a subcutaneous space-occupying lesion in the left occipital head, possibly a benign lesion (Figure 2A and B). Body surface colour ultrasound revealed a subcutaneous hypoechoic solid mass in the occipital region (Figure 2C-E).
Combined with the intraoperative findings (Figure 1D-F) and pathological examination, these findings revealed a large epidermal cyst (Figure 1G and H).
Resection of the tumour was performed under local anaesthesia.
After 3 months of follow-up, the wound had healed well, and there was no recurrence, no rupture, or fever.
However, the pathogenesis of epidermal cysts is still unclear. It is generally believed that epidermal cysts originate from the infundibular region of the hair follicle and are caused by progressive cystic dilation and destruction of the infun
Currently, histopathology is still the gold standard for diagnosing epidermal cysts. Some cysts have no epithelial wall structure. Skin cysts are divided into three main types according to the conditions of the cyst wall: (1) Skin cysts with lamellar squamous epithelium mainly consist of epidermal cysts, hair sheath cysts, lipocysts, vellus hair cysts, etc., which are common on the scalp, face, trunk and so on; (2) Nonlaminated squamous epithelial skin cysts, which mainly include apocrine sweat gland cysts, eccrine sweat gland cysts, branchial cleft cysts, and thyrohyoid cysts; these cysts are more common in the head and face; and (3) Skin cysts lacking epithelium mainly include mucous cysts, auricle pseudocysts, and tendon sheath cysts, which are mostly found in the oral mucosa, auricle, distal extension side of fingers, and near wrist joints. The pathological manifestations of epidermal cysts include the formation of intradermal cysts, a cyst wall composed of several layers of squamous epithelium, an upper cortex facing the cyst cavity, and keratinocytes constantly shed to form the contents of the cyst, which cause the tumour to grow continuously; additionally, the cyst is full of kera
Some studies have also shown that patients with unruptured epidermal cysts have larger diameters and thinner walls than those with ruptured epidermal cysts, which is consistent with most of the research findings: The larger the diameter is, the thinner the wall is, and the more likely the cyst is to rupture. Some scholars speculate that rupture may lead to an overall reduction in the size of the cyst, possibly caused by the body's foreign body reaction to the contents of the cyst and the release of various inflammatory factors, including growth factors. These factors promote the proliferation of cyst wall cells and subsequently thicken the cyst wall[10]. Several scholars have also shown that there is a positive correlation bet
Epidermal cysts are common cystic nodules on the surface of the body. The aetiology of these cysts is unclear, the clinical manifestations can vary, and the misdiagnosis rate is high. However, gigantic epidermal cysts are rare. In most cases, however, the prognosis is satisfactory. This paper analyses and summarizes the population, location, clinical and patho
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Yarmahmoodi F, Iran S-Editor: Li L L-Editor: A P-Editor: Xu ZH
| 1. | Park BS, Shin DH, Kim SH, Jung HJ, Son GM, Kim HS. Perineal squamous cell carcinoma arising from an epidermal cyst: a case report. World J Surg Oncol. 2018;16:155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Frank E, Macias D, Hondorp B, Kerstetter J, Inman JC. Incidental Squamous Cell Carcinoma in an Epidermal Inclusion Cyst: A Case Report and Review of the Literature. Case Rep Dermatol. 2018;10:61-68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 3. | Choi JE, Kwon IH, Seo SH, Kye YC, Ahn HH. Pathogenesis of Plantar Epidermal Cyst: Three-Dimensional Reconstruction Analysis. Ann Dermatol. 2016;28:133-135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Posthuma JJ, de Ruiter KJ, de Jong VM, Schepers T. Traumatic Epidermal Inclusion Cyst After Minimally Invasive Surgery of a Displaced Intra-Articular Calcaneal Fracture: A Case Report. J Foot Ankle Surg. 2018;57:1253-1255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Doorbar J, Egawa N, Griffin H, Kranjec C, Murakami I. Human papillomavirus molecular biology and disease association. Rev Med Virol. 2015;25:2-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 446] [Cited by in RCA: 587] [Article Influence: 58.7] [Reference Citation Analysis (0)] |
| 6. | Itoh Y, Ninomiya Y, Chishiki M, Ishibashi A. A gigantic epidermal cyst. Ann Plast Surg. 1999;42:572. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Egawa K, Egawa N, Honda Y. Human papillomavirus-associated plantar epidermoid cyst related to epidermoid metaplasia of the eccrine duct epithelium: a combined histological, immunohistochemical, DNA-DNA in situ hybridization and three-dimensional reconstruction analysis. Br J Dermatol. 2005;152:961-967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Lee KI, Namgoong S, You HJ, Jeon TS. Epidemiological characteristics and importance of lobulation of giant epidermal cysts: An 18-year retrospective review of 19 cases. Medicine (Baltimore). 2022;101:e29978. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 9. | Ito R, Fujiwara M, Kaneko S, Takagaki K, Nagasako R. Multilocular giant epidermal cysts. J Am Acad Dermatol. 2008;58:S120-S122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Park JS, Ko DK. A histopathologic study of epidermoid cysts in Korea: comparison between ruptured and unruptured epidermal cyst. Int J Clin Exp Pathol. 2013;6:242-248. [PubMed] |
| 11. | Min HJ, Lee JM, Han JK, Kim YJ. Influence Factor in Thickness of Cyst Wall of Epidermal Cysts. J Craniofac Surg. 2017;28:e369-e372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |