Published online Jan 26, 2024. doi: 10.12998/wjcc.v12.i3.607
Peer-review started: October 12, 2023
First decision: December 6, 2023
Revised: December 9, 2023
Accepted: January 4, 2024
Article in press: January 4, 2024
Published online: January 26, 2024
Processing time: 91 Days and 18.1 Hours
Ischemic colitis (IC) is also known as colon ischemia and is caused by colon vascular occlusion or nonocclusion, which results in a reduced blood supply to the colon and is not significant enough to maintain the metabolic function of cells, leading to intestinal wall ischemia. Its main symptoms include abdominal pain, diarrhea, and bloody stool. In severe cases, intestinal gangrene, peritonitis, intestinal stenosis and even intestinal obstruction may occur. IC induced by long-term use of certain special drugs is relatively rare in clinical practice. This article describes the clinical diagnosis and treatment of a typical case and provides a new treatment idea for the treatment of IC.
The patient was admitted to the hospital with "abdominal pain for half a month and bloody stool with mucous and pus for 3 d" and was diagnosed with "IC". Symptomatic and supportive treatment, such as antibiotics (levofloxacin), acid inhibition and stomach protection, fluid replenishment, and intravenous nutrition, was given. The patient's colonic ulcers were considered to be related to the oral administration of platelet (PLT)-raising capsules; the patient was asked to stop PLT-raising drugs for selective review via colonoscopy, and antibiotics and mesalazine enteric-coated tablets were stopped. Under the guidance of hematology consultation, 60 mg of methylprednisolone was given in combination with PLT infusion to increase the PLT. After treatment, the patient's condition stabilized, the patient’s stool turned yellow, the patient’s symptoms improved, and the patient was allowed to leave the hospital.
PLT-raising capsules can lead to IC, so clinicians should have a full understanding of the application of these drugs in the treatment of various causes of thrombocytopenia, weigh the advantages and disadvantages, and observe patients closely.
Core Tip: Ischemic colitis (IC) caused by a platelet (PLT)-raising capsule is relatively rare in the clinic. We reported the clinical diagnosis and treatment of a patient with IC caused by the use of a PLT-raising capsule and summarized the clinical diagnosis and treatment characteristics of these patients by reviewing the relevant literature.
- Citation: Wang CL, Si ZK, Liu GH, Chen C, Zhao H, Li L. Ischemic colitis induced by a platelet-raising capsule: A case report. World J Clin Cases 2024; 12(3): 607-615
- URL: https://www.wjgnet.com/2307-8960/full/v12/i3/607.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i3.607
Ischemic colitis (IC) is also known as colon ischemia (CI) and is caused by colon vascular occlusion or nonocclusion, which results in a reduced blood supply to the colon; this process is not significant enough to maintain the metabolic function of cells, leading to intestinal wall ischemia[1]. Its main symptoms include abdominal pain, diarrhea, and bloody stool. In severe cases, intestinal gangrene, peritonitis, intestinal stenosis and even intestinal obstruction may occur[2,3]. The pathogenesis of this disease has not been extensively studied, but increased clotting ability has been recognized as an important factor in the pathogenesis of IC[4]. People older than 60 years (especially women) who suffer from certain underlying diseases, such as cardiovascular and cerebrovascular diseases, diabetes, and shock, are the most prone to colon IC. The lesions can involve any segment of the colon, among which the left half of the colon, such as the sigmoid colon, descending colon and spleen region, is the most common site of lesions. This is because the region south of the sigmoid colon is the "watershed region" of the colonic blood supply, where vascular dysplasia may easily cause ischemia. In addition, the left half of the colon is supplied by the inferior mesenteric artery, which is at an acute angle to the abdominal aorta and affects blood perfusion. The rectum is supplied by both the inferior mesenteric artery and the rectal artery, and ischemia is rare. Therefore, the IC lesions were mainly in the left colon, and most of them were of the first pass type. The disease is relatively mild and can be cured after conservative medical treatment, so the prognosis is favorable[5-7]. Once ischemia improves, the patient’s condition can recover in a relatively short time, and this condition can be distinguished from other types of enteritis[5-7], such as infectious colitis, inflammatory bowel disease, pseudomembranous enteritis, diverticulitis, colon cancer, and acute mesenteric ischemia. Clinically, ischemic colitis can be divided into gangrene and nongrene. The latter can also be subdivided into transient and chronic types.
Treatment for IC usually includes fasting, gastrointestinal decompression, intravenous nutritional support, improved circulation, fluid resuscitation, empirical use of antibiotics and other symptomatic supportive treatments, and attention should be given to the treatment of the primary disease. Most patients will experience improvements in clinical symp
Abdominal pain for half a month and bloody stool with mucous and pus for 3 d.
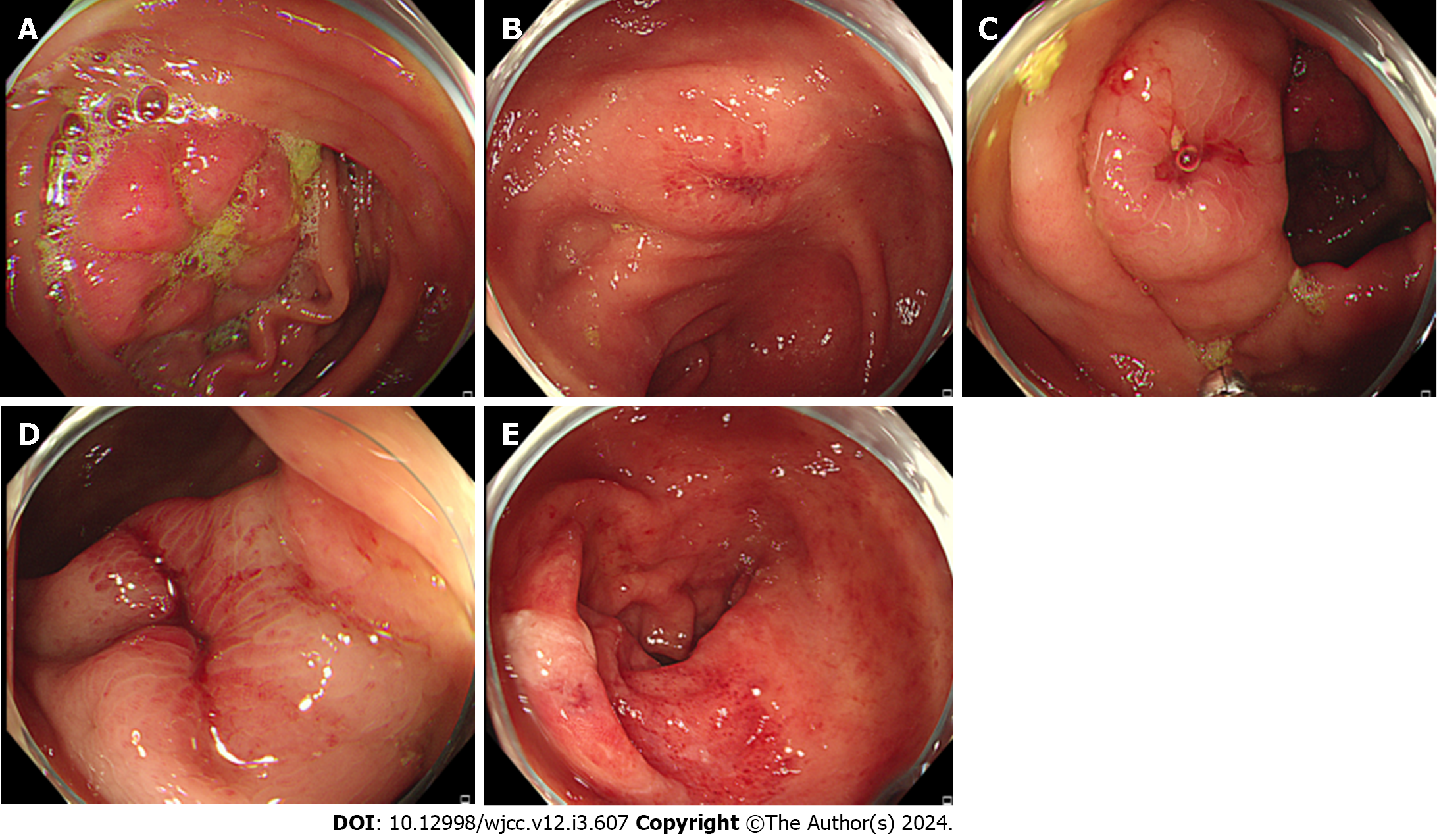
Half a month prior, the patient had abdominal pain, mainly located in the lower abdomen, which was paroxysmal. Abdominal pain was felt before the patient passed stool and was relieved after passing stool. The stool was yellow and loose and was passed 7 times a day. Twelve days prior, the patient visited the outpatient department of our hospital for further diagnosis and treatment and was treated with oral "cefixime". The frequency of stool was reduced to 2 times per day, and the abdominal pain did not significantly improve. Three days prior, the patient developed bloody stool with pus and mucous 2-3 times a day and still had paroxysmal abdominal pain, no nausea, vomiting, acid reflux, heartburn, fear of cold, fever, arthralgia, dry mouth, and dry eyes. The patient visited the outpatient department of our hospital on June 28, 2021. Gastroenteroscopy revealed chronic nonatrophic gastritis with erosion, duodenal bulbitis, and multiple colonic ulcers (Figure 1).
The patient had a history of "primary immune thrombocytopenia (ITP)" for more than 3 years and was treated with drugs such as "caffeic acid tablets and platelet (PLT)-raising capsules". Three years prior, the patient was admitted to the Department of Gastroenterology of our hospital because of "abdominal pain and blood in the stool for 12 h". The whole-abdomen computed tomography (CT) scan showed the following: (1) Thickening and edema of the colon wall and possible inflammatory changes, which were recommended to be further examined if necessary in combination with clinical evaluation; (2) calcification of the right lobe of the liver; and (3) a small amount of fluid was present in the abdominal cavity. Mesenteric CT angiography (CTA) showed the following: (1) No obvious abnormalities in the mesenteric arteries or veins; (2) changes in the colon wall consistent with ischemic enteritis, which was recommended to be interpreted within a clinical context; and (3) a possible small amount of ascites. Gastroscopy showed chronic su
Personal history: The patient was born in their original place, lived a long time in Shandong, and denied a history of contact with epidemic areas, infected water, special chemicals or radiation. The patient had a history of smoking and drinking. Marriage and childbearing history: The patient was married at the age of 22, with a healthy spouse and one son. Family history: Healthy parents, 1 brother and 1 sister, all healthy. The patient had a history of genetic disease, infectious disease or similar diseases.
The physical exam was as follows: Temperature 36.2 ℃, pulse: 97 beats/min, respiratory rate 18 breath cycles/min, blood pressure 110/90 mmHg, the patient is conscious, with normal mental status. The patient had no yellow staining of sclera, no palpebral conjunctival pallor, and no obvious abnormalities on cardiopulmonary physical examination. The patient had a flat and soft abdomen, no abdominal varicose veins and gastrointestinal type, and no tenderness or rebound pain. The liver and spleen were not palpable under the ribs, the patient had no masses, the patient had a negative Mofey's sign, there was no pain upon percussion in the areas of the liver and kidney, there were no voiced mobile sounds, and the bowel sounds were 4 times/min. No purpura or ecchymosis was observed.
Total bilirubin was 22.3 μmol/L, direct bilirubin was 7 μmol/L, high-density lipoprotein cholesterol was 1.99 mmol/L, and low-density lipoprotein cholesterol was 3.57 mmol/L. Routine blood tests showed the following: +Hypersensitive C-reactive protein: Lymphocyte percentage 18.5%, neutrophil percentage 76.4%, and PLT count 68 × 109/L. Coagulation function was 4 + D-dimer: D-dimer 0.81 mg/L. The patient’s Pure protein derivative (PPD) test was negative, and the patient’s antinuclear antibody was negative (Table 1).
| Date | Liver function kidney function blood lipid blood glucose electrolyte | Blood routine | Coagulation function four +D dimer | PPD test | Antinuclear antibody |
| 2021-06-29 | Total bilirubin 22.3 μmol/L, direct bilirubin 7 μmol/L, high-density lipoprotein cholesterol 1.99 mmol/L, low-density lipoprotein cholesterol 3.57 mmol/L | Lymphocyte percentage 18.5%, neutrophil percentage 76.4%, platelet count 68 × 109/L | D-dimer 0.81mg/L | ||
| 2021-07-03 | Negative | Negative | |||
| 2021-07-06 | Lymphocyte percentage 11%, neutrophil percentage 83.5%, absolute lymphocyte value 0.8 × 109/L, platelet count 23 × 109/L | ||||
| 2021-07-08 | Platelet count was 12 × 109/L | ||||
| 2021-07-12 | Absolute monocyte value 0.8 × 109/L, red blood cells 4.22 × 1012/L, hemoglobin 126 g/L, the mean hemoglobin concentration was 312 g/L, and the platelet count was 199 × 109/L | ||||
| 2021-07-14 | Platelet count 230 × 109/L | ||||
| 2021-07-20 | Platelet count was 81 × 109/L | ||||
| 2021-07-23 | Platelet count was 82 × 109/L |
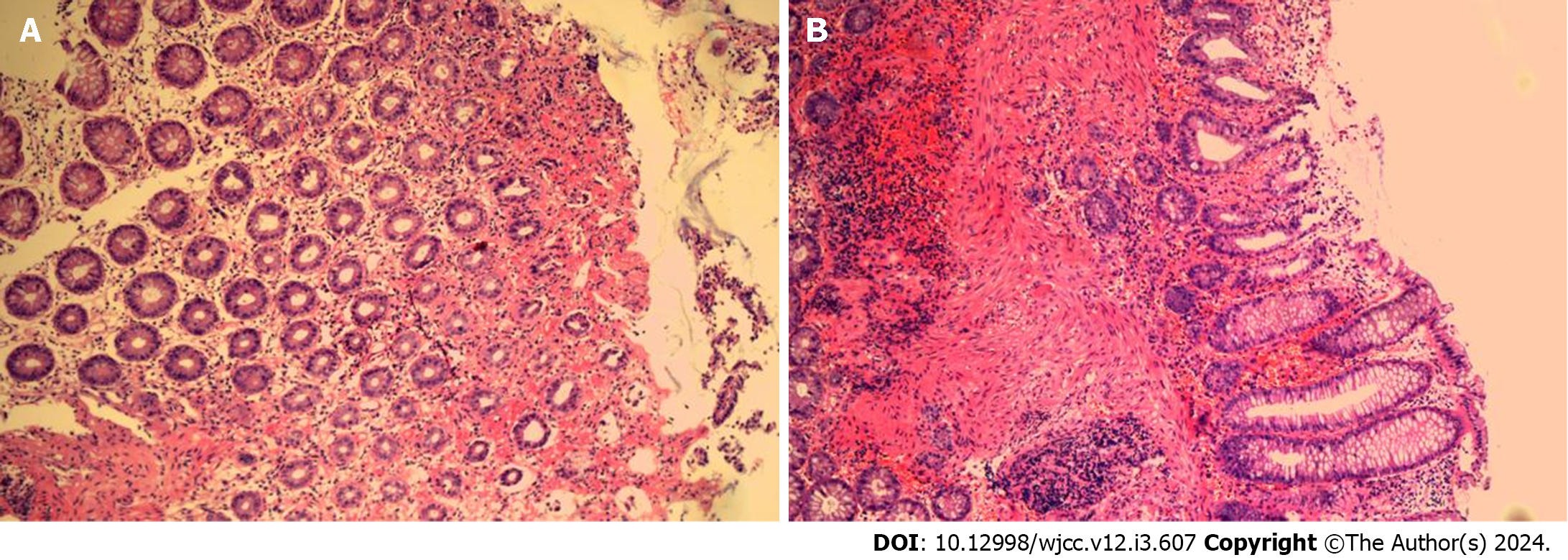
Pathology showed the following: (1) Chronic inflammation of the mucosa with superficial ulceration and eosinophils infiltrating the lamina propria; (2) (in the proximal ileocecal part of the ascending colon) mucosal chronic inflammation accompanied by acute inflammation, with scattered eosinophils infiltrating the lamina propria; (3) chronic mucosal inflammation accompanied by acute inflammation and superficial ulceration, with scattered eosinophils infiltrating the lamina propria; and (4) chronic inflammation of the mucosa (30 cm from the anus) 2021-06-28; (Table 2 and Figure 2A).
| Date | Whole abdomen CT | Mesenteric CTA | Gastroscopy | Colonoscopy | Pathology |
| 2018 | Thickening and edema of the colon wall, and possible inflammatory changes, to be furthered examined if necessary, in combination with clinical evaluation; Calcification of right lobe of liver; Small amount of fluid in abdominal cavity | No obvious abnormalitiesin mesenteric arteries and veins; Colon wall changes, consistent with ischemic enteritis, to be interpreted within clinical context; Small amount of ascites? | Chronic superficial gastritis | Multiple colonic ulcers pending investigation | (Descending colon) mucosal chronic inflammation with multiple ulcers; (ileocecal region) mucosal chronic inflammation with ulcers; (transverse colon) mucosal chronic inflammation with ulcers. Added: Acid-fast staining |
| 2021-06-28 | Chronic non-atrophic gastritis with erosion, duodenal bulbitis | Multiple colonic ulcers | Chronic inflammation of mucosa with superficial ulceration and eosinophils infiltrating the lamina propria; (in the proximal ileocecal part of the ascending colon) mucosal chronic inflammation accompanied by acute inflammation, with scattered eosinophils infiltrating the lamina propria; (65 cm from anus) chronic mucosal inflammation accompanied by acute inflammation and superficial ulceration, with scattered eosinophils infiltrating the lamina propria; chronic inflammation of mucosa (30 cm from anus) | ||
| 2021-07-19 | Colonic ulcer; Endoscopic forceps removal of colonic polyps | Tubular adenoma (50 cm from anal margin); Acute and chronic inflammation of mucosa with erosion (proximal ileocecal part of ascending colon) | |||
| 2022-08-01 | No obvious abnormality |
(1) IC was caused by PLT-raising capsule; (2) Colonic ulcers; (3) Colonic polyps; (4) Chronic nonatrophic gastritis with erosion; (5) Duodenoculitis; and (6) Primary ITP.
After admission, symptomatic and supportive treatments such as antibiotics (levofloxacin), acid inhibition and stomach protection, fluid replenishment, and intravenous nutrition were given.
The cause of the patient's multiple recurrent intestinal ulcers was unknown, and the pathology suggested ulcer formation with eosinophil infiltration. Eosinophilic gastroenteritis was further ruled out, and inflammatory bowel disease and other diseases were further ruled out. The patient was engaged in fox breeding, so it was necessary to further exclude the possibility of special types of infection. On July 3, 2021, the patient still had bloody stool with pus and mucous once a day, the patient’s PPD test was negative, and the patient’s antinuclear antibody test was negative. Mesalazine enteric-coated tablets were used for anti-inflammatory treatment, and Yunnan Baiyao was given orally for hemostasis. On July 7, 2021, the patient complained of 2-3 stools/d; the patient’s stool was watery and had mucus, pus and blood; and the patient had no other discomfort. Blood routine review + reticulocyte count revealed the following: Lymphocyte percentage, 11%; neutrophil percentage, 83.5%; absolute lymphocyte count, 0.8 × 109/L; and PLT count, 23 × 109/L. The PLT count was significantly low, and caffeic acid tablets and PLT-raising capsules were given for PLT-raising therapy. The patient had watery stool, the number of stools was increased, and oral montmorillonite powder was given to stop the diarrhea. The patient had multiple intestinal ulcers. We considered whether the "primary ITP" was related to intestinal ulcers. The possibility of multiple intestinal ulcers caused by ITP was unlikely to be considered during hematology consultation. On July, 2021, our department has organized discussions on these difficult cases. According to the Department of Immunology and Rheumatology, the patient's pathology suggested eosinophilia, which was caused by many factors, such as eosinophil granulomatous vasculitis. The patient had a normal eosinophil count and a normal blood profile, and lung (-), skin (-), and rheumatic disease results were not considered. The imaging department considered the patient's CT images to be unclear, the intestinal filling was not good, there were no enlarged lymph nodes, there was no fatty infiltration and no transmural inflammation, and there were no specific manifestations. Pathology revealed that the patient’s acid-fast test was negative, with no specific manifestations. The Department of Infectious disease said the patient had no evidence of infection (no fever, normal blood routine, negative bacterial culture, low immunoglobulin E, or uncommon parasitic infections). The chief physician advised the patient to receive ITP, oral PLT capsule treatment, and treatment with a PLT capsule containing green Dai, which can cause intestinal ulcers. Many hematological diseases are complicated by intestinal ulcers, and ITP can manifest as immune system-related ulcers. Treatment: The drug was stopped, and low-dose hormone therapy was given. At present, the patient's colonic ulcer was considered to be related to the oral administration of PLT-raising capsules, the patient was asked to stop PLT-raising drugs for selective review via colonoscopy, and antibiotics and mesalazine enteric-coated tablets were stopped. Under the guidance of hematology consultation, 60 mg of methylprednisolone was given in combination with PLT infusion to promote PLT therapy.
On July 9, 2021, the patient had no additional blood in her stool but did have pain and discomfort in her lower abdomen. Scattered hemorrhagic spots could be observed on the skin. July 12, 2021, the patient had no abdominal pain or abdominal distension, and the patient passed stool once a day with no mucus, pus or blood. Routine blood test results revealed the following: Absolute monocyte count = 0.8 × 109/L, red blood cell count = 4.22 × 1012/L, hemoglobin = 126 g/L, mean hemoglobin concentration = 312 g/L, and PLT count = 199 × 109/L. After treatment, the patient's symptoms were relieved, and there was no additional blood in the stool; the patient’s PLT count was greater than before, and the patient’s hormone concentration was reduced to 40 mg qd. On July 9, 2021, routine blood analysis revealed a PLT count of 230 × 109/L. The patient’s PLT count increased significantly after hormone treatment. No hematochezia was found after discontinuation of the PLT-raising capsule, and the dose of hormone was reduced to 20 mg qd.
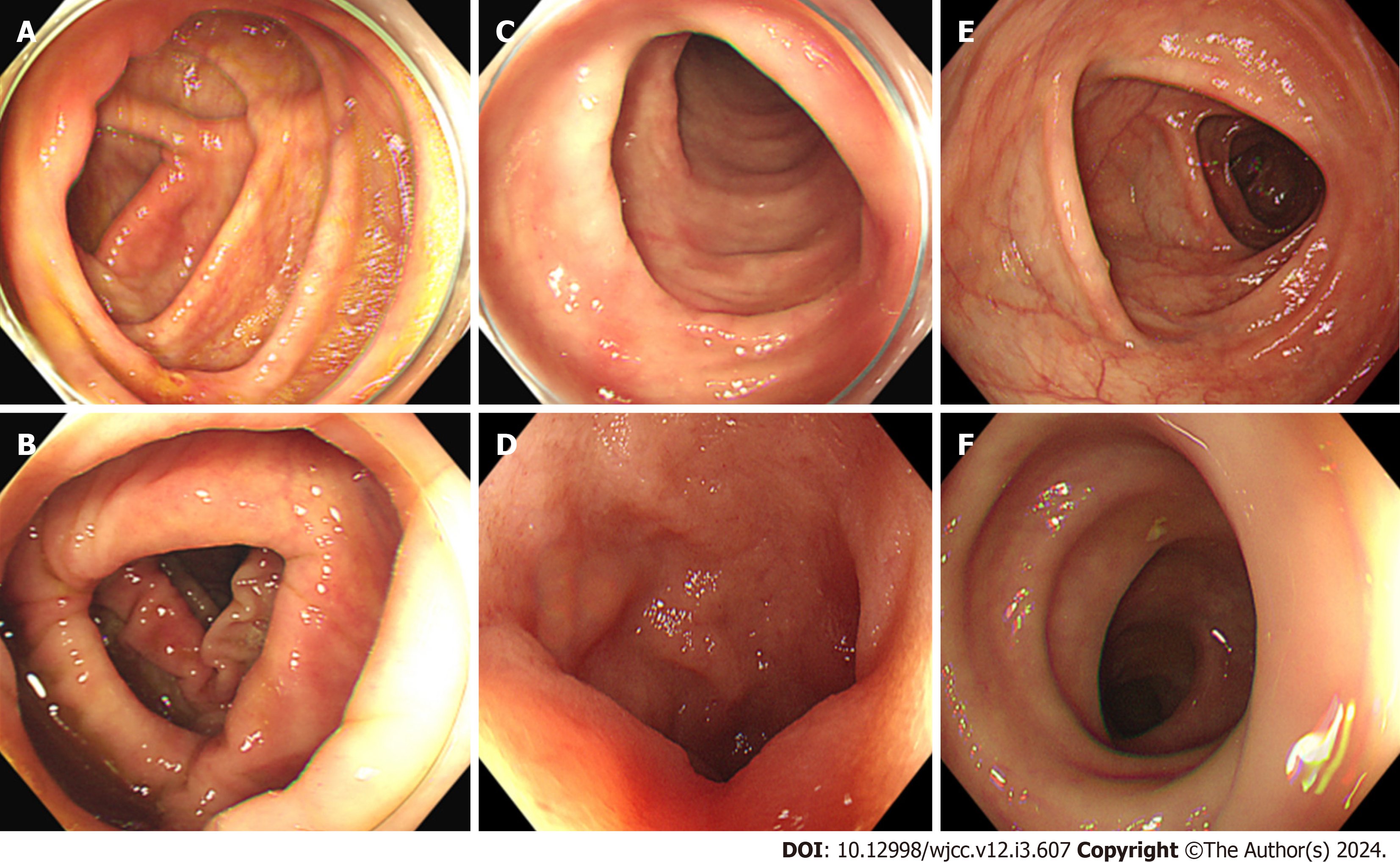
Endoscopic biopsy showed the following results: (1) Tubular adenoma (50 cm from the anal margin); and (2) acute and chronic inflammation of the mucosa with erosions (proximal ileocecal part of the ascending colon) was observed (2021-07-19; Figure 2B). On July 19, 2021, review colonoscopy showed the following: Colonic ulcer; endoscopic forceps removal of colonic polyps (Figure 3A-C). Reexamination colonoscopy of the patient showed significant improvement in the severity of the colonic ulcer, which was considered to be associated with the PLT-raising capsule. The patient's symptoms improved after symptomatic treatment, such as acid inhibition, nutritional support, hemostasis, PLT infusion, and hormone therapy, and the patient’s PLT count was greater than before. The patient was discharged. The patient was told to have the tests for blood routine and coagulation function rechecked 3 d after discharge, to return to the hematology department, to adjust the hormone dosage under the guidance of specialists, and to not reduce or stop the medication without consulting with the doctor. The patient was monitored for any changes in stool color, her gastroenteroscopy was reviewed regularly, and she had follow up for her discomfort.
After discharge, the patient did not use a PLT-raising capsule again and had no abdominal pain, diarrhea, blood in the stool or other symptoms. On August 1, 2022, a review of the colonoscopy of the patient at our hospital showed no obvious abnormalities (Figure 3D-F).
The onset of this patient was acute, with abdominal pain, diarrhea, and hematochezia. Colonoscopy revealed multiple ulcers in the colon. The clinical symptoms improved rapidly after the discontinuation of the PLT-raising capsule, while continued use of the drug led to worsening of the disease. The patient had a similar history 3 years prior, and whole-abdominal CT showed thickening and edema of the colon wall. Inflammatory changes were considered. Mesenteric CTA showed: (1) No obvious abnormalities in the mesenteric arteries or veins; and (2) changes in the colon and intestinal wall were consistent with ischemic enteritis. Colonoscopy revealed multiple ulcers in the colon. It was reported that ischemic colitis occurs in patients vaccinated with a second dose of the coronavirus disease 2019 inactivated vaccine[8]. The patient presented with abdominal pain after vaccine injection. It was considered whether this difference was related to vaccination. However, the patient had a similar medical history 3 years prior to admission, the patient’s clinical symptoms improved rapidly after the discontinuation of the PLT-raising capsule, and the patient did not use a PLT-raising capsule again after discharge. Reexamination via colonoscopy at our hospital on August 1, 2022 showed no obvious abnormalities. Considering the above factors, a diagnosis of IC caused by a PLT-raising capsule was established.
Drug-related IC can occur due to the use of disease-causing drugs, and the clinical symptoms and auxiliary findings are consistent with the characteristics of ischemic lesions in the colon[9]. Clinical symptoms can rapidly improve after the discontinuation of pathogenic drugs, while continuous use of these drugs leads to continuous progression of the disease, which is a unique clinical feature of drug-related IC. Recent studies have shown that the incidence of right colon lesions in patients receiving drug-related IC is greater than that in patients receiving IC[10]. Thus, patients with drug-related IC may have a greater incidence of general abdominal pain or right abdominal pain than patients with IC, which primarily occurs on the left side.
In terms of diagnosis, laboratory tests revealed elevated peripheral white blood cells, decreased hemoglobin to varying degrees, elevated blood amylase, elevated D-dimer, elevated lactate dehydrogenase, and decreased serum HCO3- levels. Stool cultures of Salmonella, Campylobacter Shigae and Escherichia, the latter of which has been implicated in causing CI, should be performed; parasitic or viral infections such as cytomegalovirus should also be ruled out[4]. Plain abdominal radiographs may reveal nonspecific findings, such as thumb marks, inflatable rings, thickening of the intestinal wall, and intestinal failure; these findings are effective for ruling out colon infarction and intestinal perforation. Abdominal CT can indicate the location of the diseased intestinal segment and the extent of involvement and can also reveal complications such as concomitant disease and perforation. The main manifestations are intestinal wall thickening, blurring of the periintestinal fat space, and occasional intestinal wall gas[11]. CT angiography is of little significance in the diagnosis of IC because IC is a nonocclusive and transient ischemic injury of small vessels. Because it cannot show tertiary blood vessels, it is of little clinical significance. Colonoscopy is considered the gold standard for the diagnosis of IC. Under the microscope, intestinal mucosal congestion, edema, ecchymosis, and submucosal bleeding were observed, the mucosa was dark red, the vascular network disappeared, and some mucosal necrosis occurred, followed by mucosal detachment and ulcer formation. The boundary between the lesion site and the normal intestinal segment was clear. Under the microscope, the bleeding nodules were the characteristic manifestations of IC and were caused by submucosal bleeding or edema[11]. Colonoscopy should be avoided when patients show signs of peritonitis. When an endoscopist finds gangrene, he or she should directly terminate the colonoscopy and perform emergency surgery[12]. Histopathological analysis revealed a large number of fibrinous thrombi and hemosiderin-containing cells in the submucosa. Compared with those in patients with IC, the incidence of eosinophilic infiltration in patients with drug-related IC was greater, and the incidence of ulcers and necrosis was lower.
The patient received an oral PLT-raising capsule to treat the ITP. According to traditional Chinese medicine, blood stasis, blood heat and qi deficiency are the main causes of ITP. Clearing heat, cooling blood and promoting blood stasis are the main principles for treating this disease. It clears heat, detoxifies, disperses stasis, eliminates spots, cools blood and stops bleeding. The main drug used to treat PLT-raising capsules is indigo naturalis, a pigment produced from the stems and leaves of Indigo, Persicaria tinctoria, and Indigotica tinctoria. Its main ingredients are indigo and indirubin. Modern pharmacological studies show that the active components indigo, indirubin and indigo can effectively inhibit the activity of bacteria and regulate immune function. Forsythia can have anti-inflammatory and antibacterial effects, reduce capillary permeability, and inhibit allergic reactions in the body. Studies have shown that PLT-raising capsules can not only reduce inflammation, inhibit bacteria and regulate the body's immune function but also increase the PLT and improve coagulation function. Studies[13,14] have shown that traditional Chinese medicines containing indigo naturalis components (such as Compound Qingdai Pill and PLT-raising capsules) can cause IC. The pathogenesis of IC induced by Indigo naturalis may be related to the following factors: (1) Indigo naturalis stimulates colon mucosa and damages the colonic mucosa; (2) indigo naturalis can cause diarrhea, and severe diarrhea can lead to a reduced systemic effective circulating blood volume, increased intestinal pressure, vasospasm, etc., resulting in insufficient blood supply to the colon wall; and (3) indigo naturalis has the effect of cooling blood and stopping bleeding and has obvious procoagulant effects, which can lead to intravascular cellulose thrombosis and blocking blood vessels, thus causing ischemic necrosis of the colonic mucosa[13-16]. Elderly patients may have intestinal arteriosclerosis, and the use of Qingdai is more likely to induce ischemic lesions[15].
ITP-induced bleeding refers to thrombocytopenia in the peripheral blood that results in skin, mucosa, and even internal bleeding, but spontaneous bleeding usually occurs when the PLT count is lower than 20 × 109/L. The gastrointestinal bleeding of this patient was not accompanied by skin petechiae or ecchymosis, which was inconsistent with the clinical characteristics of intestinal bleeding caused by ITP. In addition, when the patient had blood in the stool and was taking Chinese medicine containing Qingdai, the symptoms improved, and the patient did not experience recurrence after stopping the drug, suggesting that the patient's digestive tract lesions were closely related to the use of the drugs. However, it remains to be studied whether patients with ITP-based lesions have synergistic effects with Qingdai to further increase the risk of intestinal ischemia.
When patients develop drug-induced IC, disease-causing drugs should be stopped immediately, and similar treatments should be used for other causes of IC[17,18]. The treatment of IC is related to the severity of the patient's condition[1,19]. For severe patients, intravenous infusion, optimal hemodynamic status, intestinal rest, empirical use of antibiotics and avoidance of vasoconstrictor therapy were adopted, and most patients experienced improvement in clinical symptoms within 1-2 d. Patients with complications may need surgical intervention[18]. Medical treatment: Most patients with acute mild to moderate IC can receive conservative medical treatment, including routine fasting, gas
In conclusion, although traditional Chinese medicine containing Indigo naturalis is an effective drug for the clinical treatment of ITP, patients should be reminded to observe digestive tract symptoms and stool characteristics during its treatment. If abdominal pain, diarrhea, or blood in the stool are present, the clinician should consider the possibility of ischemic colitis, it should be recommended that the patient discontinue the drug immediately, and aggressive treatment should be prescribed to prevent serious complications. If a patient has had such an adverse reaction to previous medication, it is best not to use the drug again.
The patient developed IC after taking PLT-raising capsules; however, the symptoms improved rapidly after drug withdrawal, and there was no recurrence during follow-up, indicating that the occurrence of IC in the patient was closely related to the use of the PLT-raising capsules. PLT-raising capsules can lead to IC, so clinicians should have a full understanding of the application of these drugs in the treatment of various causes of thrombocytopenia, weigh the advantages and disadvantages, and observe closely. Once abdominal pain, diarrhea, or blood in the stool occur, the drug should be stopped immediately, active treatment should be administered, and further use of the pathogenic drug should be avoided.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Rezus E, Romania S-Editor: Qu XL L-Editor: A P-Editor: Chen YX
| 1. | Brandt LJ, Feuerstadt P, Longstreth GF, Boley SJ; American College of Gastroenterology. ACG clinical guideline: epidemiology, risk factors, patterns of presentation, diagnosis, and management of colon ischemia (CI). Am J Gastroenterol. 2015;110:18-44; quiz 45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 193] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 2. | Chen ZW, Yao F, Hu BW, Cao CX. Risk factors of ischemic colitis. Zhejiang Yixue. 2019;41:1426-1427. |
| 3. | Deng YB, Liu YL, He DX. Research progress of ischemic colitis. Zhongguo Linchuang Yanjiu. 2018;31:701-704. [DOI] [Full Text] |
| 4. | Theodoropoulou A, Koutroubakis IE. Ischemic colitis: clinical practice in diagnosis and treatment. World J Gastroenterol. 2008;14:7302-7308. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 159] [Cited by in RCA: 161] [Article Influence: 9.5] [Reference Citation Analysis (2)] |
| 5. | Ruan SL, Gu XJ, Guan QB. Domestic literature analysis of epidemiology and clinical features of ischemic colitis. Zhonghua Laonian Yixue Zazhi. 2015;34:565-569. |
| 6. | Chinese Expert Recommendations for the Diagnosis and Treatment of Ischemic Bowel Disease Writing Group; Chinese Geriatric Society of the Chinese Medical Association; Editorial Board of the Chinese Journal of Geriatrics. Chinese Expert Advice on the Diagnosis and Treatment of ischemic bowel disease in the elderly. Zhonghua Laonian Yixue Zazhi. 2011;30:1-6. [DOI] [Full Text] |
| 7. | Zhang LX, Chen FY. Focus on the diagnosis and treatment of ischemic colitis. Shijie Huaren Xiaohua Zazhi. 2016;24:3647-3656. [DOI] [Full Text] |
| 8. | Cui MH, Hou XL, Liu JY. Ischemic colitis after receiving the second dose of a COVID-19 inactivated vaccine: A case report. World J Clin Cases. 2022;10:3866-3871. |
| 9. | Li Y, Zu M, Ding SG. Advances in the study of drug-associated ischaemic colitis. Weichangb ingxue He Ganbingxue Zazhi. 2022;31:5-8. |
| 10. | Brechmann T, Günther K, Neid M, Schmiegel W, Tannapfel A. Triggers of histologically suspected drug-induced colitis. World J Gastroenterol. 2019;25:967-979. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Wu J, Tian ZB, Xu YH, Ding XL, Wang XW, Ren LL. A case of heavy ischaemic colitis due to platelet-raising capsules and review of the literature. Shijie Huaren Xiaohua Zazhi. 2017;25:3000-3004. |
| 12. | Doulberis M, Panagopoulos P, Scherz S, Dellaporta E, Kouklakis G. Update on ischemic colitis: from etiopathology to treatment including patients of intensive care unit. Scand J Gastroenterol. 2016;51:893-902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 13. | Song ZJ, Cao KS, Zhu YF, Yang MY. A case of ischaemic colitis caused by Compound Qingdai pill. Xinyao Yu Linchuang. 1991;126. |
| 14. | Wang CH, Jin D, Zhang HY, Cai JT, Du Q. A case of ischaemic enteritis caused by platelet-raising capsules. Zhonghua Xiaohua Zazhi. 2014;704-705. |
| 15. | Zhang L, Duan LP, Yang WH, Lv, YM, Lin SR. Clinical characteristics and possible pathogenic mechanisms of haematochezia caused by traditional Chinese medicines containing qingdai ingredients. Weichangbingxue He Ganbingxue Zazhi. 2004;13:161-164. |
| 16. | SuoBJ, Zhou LY, Ding SG, Lv YM, Gu F, Lin SR, Zheng YA. Endoscopic and clinical characterisation of qingdai-associated ischaemic colonic mucosal injury. Zhonghua Neike Zazhi. 2011;50:646-649. |
| 17. | Hamdeh S, Micic D, Hanauer S. Drug-Induced Colitis. Clin Gastroenterol Hepatol. 2021;19:1759-1779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 18. | Jessurun J. The Differential Diagnosis of Acute Colitis: Clues to a Specific Diagnosis. Surg Pathol Clin. 2017;10:863-885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 19. | Wang J, Huang JA. Progress in the early diagnosis and treatment of ischaemic colitis. Linchuang Neike Zazhi. 2019;36:440-443. |
| 20. | Yin MY, Xu CF. Analysis of the clinical characteristics of 50 patients with ischaemic colitis. Weichangbingxue He Ganbingxue Zazhi. 2020;29:305-308. |
| 21. | Zhang CY, Wang S, Wu JW, Sun BB, Sun B, Zhang X. Clinical analysis of ischaemic colitis with literature review. Zhongguo Linchuang Yisheng Zazhi. 2019;47:1196-1198. |
| 22. | Trotter JM, Hunt L, Peter MB. Ischaemic colitis. BM. 355:i6600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |