Published online Jan 26, 2024. doi: 10.12998/wjcc.v12.i3.517
Peer-review started: September 17, 2023
First decision: December 18, 2023
Revised: December 21, 2023
Accepted: January 3, 2024
Article in press: January 3, 2024
Published online: January 26, 2024
Processing time: 123 Days and 0.1 Hours
Studies on varicose veins have focused its effects on physical function; however, whether nonsurgical treatments alter muscle oxygenation or physical function remains unclear. Moreover, the differences in such functions between individuals with varicose veins and healthy individuals remain unclear.
To investigate changes in physical function and the quality of life (QOL) following nonsurgical treatment of patients with varicose veins and determine the changes in their muscle oxygenation during activity.
We enrolled 37 participants (those with varicose veins, n = 17; healthy individuals, n = 20). We performed the following measurements pre- and post-nonsurgical treatment in the varicose vein patients and healthy individuals: Calf muscle oxygenation during the two-minute step test, open eyes one-leg stance, 30 s sit-to-stand test, visual analog scale (VAS) for pain, Pittsburgh sleep quality index, physical activity assessment, and QOL assessment.
Varicose veins patients and healthy individuals differ in most variables (physical function, sleep quality, and QOL). Varicose veins patients showed significant differences between pre- and post-nonsurgical treatment— results in the 30 sit-to-stand test [14.41 (2.45) to 16.35 (4.11), P = 0.018), two-minute step test [162.29 (25.98) to 170.65 (23.80), P = 0.037], VAS for pain [5.35 (1.90) to 3.88 (1.73), P = 0.004], and QOL [39.34 (19.98) to 26.69 (17.02), P = 0.005]; however, no significant difference was observed for muscle oxygenation.
Nonsurgical treatment improved lower extremity function and QOL in varicose veins patients, bringing their condition close to that of healthy individuals. Future studies should include patients with severe varicose veins requiring surgery to confirm our findings.
Core Tip: Nonsurgical treatment improved lower extremity function and quality of life in patients with varicose veins, bringing their condition close to that of healthy individuals. However, this study found no significant difference in muscle oxygenation. We posit that significant changes may be observed in more severely ill patients or long-term follow-up.
- Citation: Kim GM, Kim B, Jang M, Park JH, Bae M, Lee CW, Kim JW, Huh U. Benefit in physical function and quality of life to nonsurgical treatment of varicose veins: Pilot study. World J Clin Cases 2024; 12(3): 517-524
- URL: https://www.wjgnet.com/2307-8960/full/v12/i3/517.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i3.517
Varicose veins are a prevalent vascular condition worldwide, with have a prevalence of 10% in the population; further, the prevalence ranges from 5%-15% in men and 2%-29% in women[1]. Varicose veins are veins that are tortuous and elongated, which are dilated to at least 3 mm in diameter and evaluated when patients are in a standing position[1]. Severe conditions such as deep vein thrombosis (DVT) and pulmonary embolism may arise if varicose veins are left untreated[2,3]. Patients with varicose veins can receive either conservative or surgical treatment options depending on their clinical condition and personal preferences[4-6].
Varicose is a chronic venous disease that mainly affects the lining of veins at the bottom of the calf muscles. It causes the accumulation of blood flow and swelling in the leg due to an increase in venous pressure. Weakened valves of the veins are also an important factor in the development of varicose disease. They may be characterized by a decrease in collagen and elasticity, resulting in skin pigmentation, texture, and diseases, among others, that negatively impact the quality of life (QOL)[7,8].
Moreover, there was a risk of reduced physical function due to disease progression in varicose vein[9]. Varicose veins can result in decreased physical function and lower QOL owing to impaired leg function, such as decreased lower extremity strength and limited mobility caused by feelings of leg heaviness or tightness from varicosities[10]. Further, impaired leg function can lead to varicose veins owing to reduced contraction of leg muscles that are crucial for venous return[11]. Studies have unveiled a complex interplay in this condition wherein reduced blood circulation and heightened pressure within varicose veins contribute to diminished oxygen content in the surrounding muscles. Techniques such as near-infrared spectroscopy (NIRS) can be used to investigate this phenomenon further[12].
Although varicose veins have been studied with a focus on physical function, whether nonsurgical treatments for varicose veins can alter muscle oxygenation or physical function remains unclear. Moreover, the difference in such functions between individuals with varicose veins and healthy individuals remains unclear. Thus, this study aimed to investigate changes in physical function and QOL and determine changes in muscle oxygenation during activity in patients with varicose veins following nonsurgical treatment.
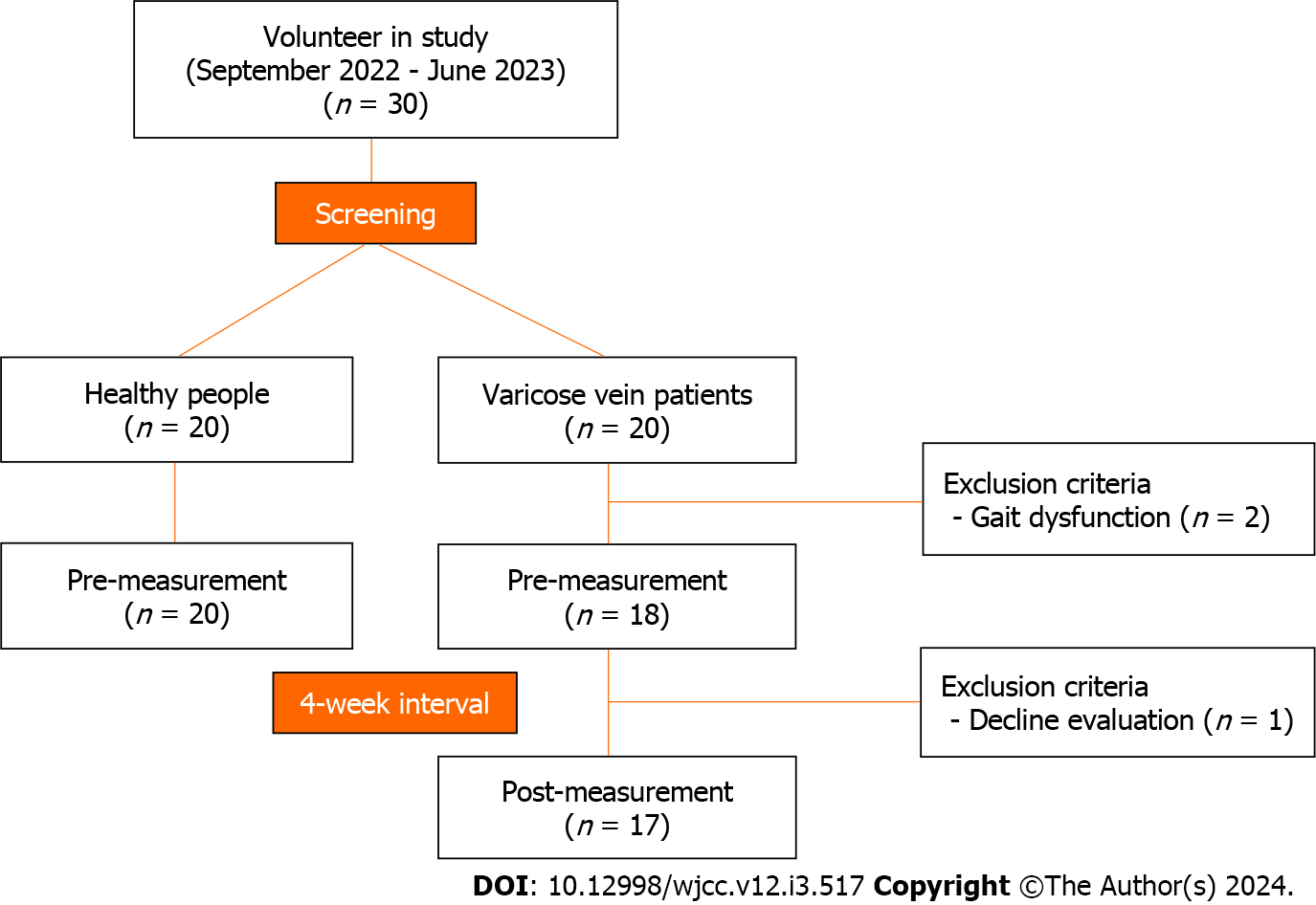
Between September 2022 and June 2023, participants were enrolled in this study as shown in Figure 1. Of the 40 participants in the Pusan National University Hospital, three were excluded for the following reasons: (1) Gait dysfunction (n = 2); and (2) decline evaluation (n = 1). Finally, 37 participants (17 patients with varicose veins and 20 healthy adults) were enrolled. Ultrasound was performed to measure leg veins. The treatment group was followed up after 4 wk of treatment initiation. This study was approved by the Research Ethics Committee of Pusan National University Hospital (2203-034-112). All participants were provided a detailed description of the experiment, and written informed consent was obtained before participation, in accordance with the ethical standards of the Declaration of Helsinki. All methods were performed in accordance with the approved study plan, as well as with relevant guidelines and regulations.
Based on the patient’s medical history and clinical presentation, a duplex ultrasound assessment was performed on suspected outpatients with varicose veins. After positioning each leg on the stair and floor, an ultrasound was used to locate the target vein of each leg, and the assessment region was pressed to confirm reflux. Varicose vein was diagnosed in case of reflux > 1 s in the deep vein and > 0.5 s in the superficial vein. For analysis, only outpatients classified with C0 and C1 Lower limb lesions were included. Patients with C2 or higher lower limb lesions were excluded from analysis and underwent to surgical treatment. Additionally, patients with a history of deep vein thrombosis were also excluded.
Patients were instructed to stand barefoot, elevating one leg approximately 10 cm above the ground such that the raised foot was close to, but not in contact with, the supporting leg on the ground; they were asked to focus at a fixed point on the wall at eye level for the open eyes one-leg stance test, measured in seconds[13]. The participant was instructed to execute as many steps as possible (reaching the predetermined height) within the allotted 2 min. For the 30s Sit-to-Stand Test, participants were instructed to cross their arms over their chest and sit and stand 30 s as quickly as possible; the elapsed time was measured[14]. The objective of the 2-min step test was to establish the number of steps performed in situ in 2 min. Following the ‘start’ signal, the participant commenced marching in situ, raising their knees to the specified height, defined as the midpoint between the patella and the iliac crest[15]. The Moxy Monitor (Fortiori Design LLC) is a NIRS device that provides precise measurements useful for applications in sports. The device’s detectors are located at 12.5 and 25 mm from the emitter. Measured by muscle oxygen saturation (SmO2 and total hemoglobin (tHB)[16]. We applied NIRS to the soleus muscle during the bipedal 2-minute step test to determine muscle oxygenation during activity.
A pain score using a 10 cm visual analog scale (VAS) (0 is defined as no pain, and 10 is defined as the worst possible pain) was administered by the principal investigator or a trained nurse[17]. The Pittsburgh sleep quality index (PSQI) is a questionnaire used to assess global sleep quality. The score considers the following seven components: sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, medication use, and daytime dysfunction. These questions are rated on a 4-point Likert scale in terms of frequency or severity of the problem (e.g., 0 = not in the past month, 1 = less than once a week, 2 = once or twice a week, 3 = three or more times a week). The total of the individual scores gives a global PSQI score ranging from 0 to 21, with higher scores indicating poorer sleep quality[18]. Physical activity was assessed using the Korean version of the international physical activity questionnaire-short version (IPAQ-S)[19]. IPAQ-S questions physical activity time and sedentary time. The structured items in the IPAQ-S provide separate scores on sedentary, walking, moderate-intensity, and vigorous-intensity activity, and we used the item for moderate to vigorous physical activity. QOL was assessed using the chronic venous insufficiency questionnaire 2 (CIVIQ2)[20], which has a total of 24 items in 5 domains: discomfort, pain, physical, psychological, and social. Response to each question was rated on a scale of 1-5 (0 is defined as a minimal negative effect on daily activities or well-being, and 5 is defined as the represented maximal negative effect). Duration of edema was rated on a scale of 1-3. The combined scores of the five dimensions were used to calculate the total score, with higher scores indicating poorer QOL.
Statistical analysis was performed using the SPSS program for Windows (version 25, SPSS Inc., Chicago, IL, United States). The characteristics of the study population are presented as mean ± SD for continuous variables and as frequencies and proportions for categorical variables. The chi-square test was used for hypothesis testing. Pearson’s correlation coefficient was used to evaluate the degree of correlation between the two variables. Student’s t-test of variance was performed to compare measures and sarcopenia differences among the varicose vein patients and healthy individuals. A paired t-test was used to compare pre- and post-nonsurgical treatment differences for the treatment of varicose veins. P values < 0.05 were considered significant.
Table 1 shows the comparison of healthy individuals and varicose veins patients. The mean (SD) age of the healthy individuals and varicose veins patients was 52.60 (6.50) years and 60.06 (10.69) years, respectively (P = 1.000), with 70.0% and 70.6% (P = 0.074) of participants, respectively, were female. The mean physical function for the open eyes one-leg stance (left and right), FTTS test, and 2-min step test were 90.43 (34.61) s, 34.92 (28.48) s, 101.39 (29.30) s, 39.26 (28.57) s, 20.70 (5.42) count, 14.41 (2.45) count, 186.50 (19.09) count, and 162.29 (25.98) count, respectively (P values: < 0.001, < 0.001, 0.005 and 0.017 respectively). Questionnaire variables for VAS, PSQI, QOL were 1.00 (1.05) point, 5.35 (1.90) point, 4.10 (2.18) point, 9.35 (3.43) point, and 8.63 (8.55) point 39.34 (1.98) point, respectively (P values: < 0.001, all variables). For other variables, no significant differences were observed between healthy individuals and patients with varicose veins.
| Variables | Healthy people (n = 20) | Varicose vein (n = 17) | P value |
| Female (%) | 14 (70.0) | 12 (70.6) | 1.000 |
| Age (yr) | 57.60 ± 6.50 | 60.06 ± 10.69 | 0.396 |
| Open eyes one leg stance, left (s) | 90.43 ± 34.61 | 34.92 ± 28.48 | < 0.001 |
| Open eyes one leg stance, right (s) | 101.39 ± 29.30 | 39.26 ± 28.57 | < 0.001 |
| 30 s-cahir standing test (count) | 20.70 ± 5.42 | 14.41 ± 2.45 | 0.005 |
| Two-minute step test (count) | 186.50 ± 19.09 | 162.29 ± 25.98 | 0.017 |
| Visual analogue scale (point) | 1.00 ± 1.05 | 5.35 ± 1.90 | < 0.001 |
| PSQI (point) | 4.10 ± 2.18 | 9.35 ± 3.43 | < 0.001 |
| MVPA (point) | 219.00 ± 214.50 | 113.24 ± 170.03 | 0.169 |
| Quality of life (point) | 8.63 ± 8.55 | 39.34 ± 19.98 | < 0.001 |
| SmO2, left | 30.80 ± 15.54 | 23.88 ± 8.20 | 0.140 |
| tHb, left | 14.07 ± 5.99 | 12.70 ± 0.97 | 0.492 |
| SmO2, right | 25.08 ± 13.47 | 26.06 ± 6.68 | 0.833 |
| tHb, right | 12.23 ± 0.29 | 12.42 ± 0.46 | 0.270 |
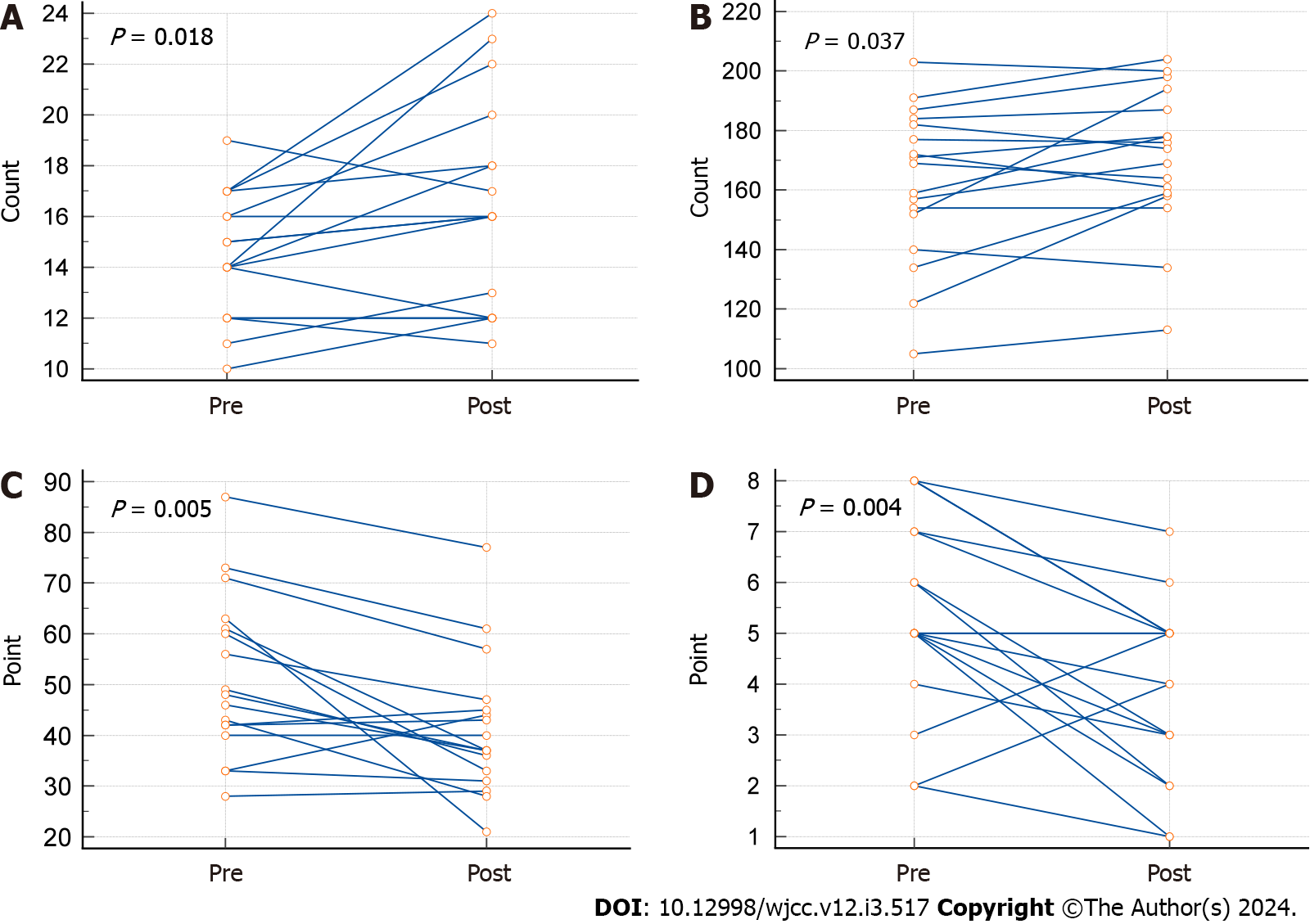
The comparison of pre- and post-nonsurgical treatment in patients with varicose veins is shown in Table 2 and Figure 2. The results were significantly different between pre- and post-nonsurgical treatment in the FTTS test [14.41 (2.45) to 16.35 (4.11), P = 0.018], 2-minute step test [162.29 (25.98) to 170.65 [(23.80), P = 0.037], VAS [5.35 (1.90) to 3.88 (1.73), P = 0.004), and QOL [39.34 (19.98) to 26.69 (17.02), P = 0.005]. No significant differences were observed between the pre- and post-nonsurgical treatment test results for other variables.
| Variables | Pre | Post | P value |
| Open eyes one leg stance, left (s) | 34.92 ± 28.48 | 45.46 ± 39.57 | 0.066 |
| Open eyes one leg stance, right (s) | 39.26 ± 28.57 | 42.72 ± 35.79 | 0.476 |
| 30s-cahir standing time (count) | 14.41 ± 2.45 | 16.35 ± 4.11 | 0.018 |
| Two-minute step test (count) | 162.29 ± 25.98 | 170.65 ± 23.80 | 0.037 |
| Visual analogue scale (point) | 5.35 ± 1.90 | 3.88 ± 1.73 | 0.004 |
| PSQI (point) | 9.35 ± 3.43 | 8.35 ± 3.57 | 0.176 |
| MVPA (min) | 113.24 ± 170.03 | 182.94 ± 320.64 | 0.411 |
| Quality of life (point) | 39.34 ± 19.98 | 26.69 ± 17.02 | 0.005 |
| SmO2, left | 23.88 ± 8.20 | 26.44 ± 8.52 | 0.154 |
| tHb, left | 12.70 ± 0.97 | 12.52 ± 0.41 | 0.410 |
| SmO2, right | 26.06 ± 6.68 | 25.88 ± 7.62 | 0.914 |
| tHb, right | 12.42 ± 0.46 | 12.36 ± 0.33 | 0.407 |
We found a difference in physical function and muscle oxygenation between healthy individuals and those with varicose veins. In addition, individuals who received nonsurgical treatment showed improved physical function and QOL; however, there was no significant difference in muscle oxygen saturation. Therefore, nonsurgical treatment of varicose veins has the advantage of reducing limitations and improving daily activities.
Varicose vein patients showed a lower open eyes on-leg stance, FTTS test, and 2-minute step test results, indicating lower physical function and physical activity (Table 1). Deterioration of lower limb function in varicose veins is attributed to several factors, including venous valve dysfunction and venous insufficiency, resulting from weakened or damaged valves, disrupted efficient blood flow, causing blood to pool in the veins[21]. This leads to swelling, discomfort, and impaired mobility[22]. Increased pressure within the affected veins contributes to their enlargement and adversely affects surrounding tissues, further interfering with normal function[23]. Inflammation in varicose veins exacerbates tissue damage and reduces muscle function in the lower limbs[24]. In particular, lifestyle factors such as prolonged standing or sitting, lower physical activity, and higher sedentary time can worsen symptoms and impair lower limb function[11].
PSQI scores were also high in patients with varicose veins, suggesting that the pain index was high, indicating that sleep quality was impaired by pain (Table 1). Previous studies suggest that poor sleep quality may be a problem in individuals with leg pain associated with varicose veins[25]. Leg pain can reduce sleep quality and further disrupt sleep, creating a recurring pattern of pain and sleep disturbances[26]. As a result, the QOL deteriorates.
Further, besides leg pain (vas), the 30s Sit-to-Stand Test, two-minute step, and QOL were improved by nonsurgical treatment (Table 2 and Figure 1). It has been confirmed that nonsurgical treatment of varicose veins without exercise or other interventions improves physical function and quality of life in middle-aged adults but not young adults. However, whether decreased physical activity or varicose veins occurs first remains unknown[27]. Increased physical activity, reduced pain, and improved physical function after nonsurgical treatment of varicose veins may be important outcomes when selecting a treatment method. It is necessary to further enhance the recovery of physical function with appropriate exercise after treatment.
Our study had some limitations. First, the sample size was small and limited to patients undergoing nonsurgical treatment. Follow-up studies should be conducted with large sample sizes and comparisons including surgical treatment. Second, this study found no significant difference in muscle oxygenation (Table 2), whereas previous studies have shown changes in muscle oxygen saturation in patients with varicose veins using NIRS[12]. This might have been caused by the short follow-up period (4 wk); significant changes may be observed in more severely ill patients. Besides, since the functions of the venous and lymphatic systems are closely related, many vascular disorders may not be attributed solely to either the venous system or lymphatic ducts[28,29]. Therefore, future studies need to compare the functional differences observed in patients with the involvement of both the venous and lymphatic systems.
In conclusion, nonsurgical treatment improved lower extremity function and QOL in patients with varicose veins, bringing their condition close to that of healthy individuals. Future studies should include a large number of patients with varicose veins requiring surgery to confirm the conclusions of this study.
Varicose vein has a negative impact on both quality of life (QOL) and physical function, resulting in reduced lower extremity strength and mobility. Impaired circulation leads to reduced muscle oxygenation, which contributes to these effects. However, it is unclear how nonsurgical treatments affect muscle oxygenation and physical function.
Few studies have looked at changes in physical function, quality of life and muscle oxygenation following non-surgical management of varicose vein disease.
Assess the effect of non-surgical treatment on the physical function and quality of life of patients with varicose veins. Additionally, evaluate alterations in muscle oxygenation during activity.
A total of 37 participants were enrolled in the study, including 17 with varicose veins and 20 healthy adults. Physical function, QOL, and muscle oxygenation were assessed before and after treatment initiation in the varicose vein group (Healthy adult group only pre-measured).
Physical function, pain index, and quality of life improved in patients with varicose veins before and after non-surgical treatment. However, no significant change in muscle oxygenation was observed.
Non-surgical treatments can return patients with varicose veins to a level of function and quality of life comparable to healthy adults.
Future studies should observe changes in physical function and muscle oxygen saturation in patients with varicose veins requiring surgery to extend the conclusions of this study.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Health care sciences and services
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Yoshida S, Japan S-Editor: Liu JH L-Editor: A P-Editor: Yuan YY
| 1. | Medical Advisory Secretariat. Endovascular radiofrequency ablation for varicose veins: an evidence-based analysis. Ont Health Technol Assess Ser. 2011;11:1-93. [PubMed] |
| 2. | Lin F, Zhang S, Sun Y, Ren S, Liu P. The management of varicose veins. Int Surg. 2015;100:185-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 3. | Raetz J, Wilson M, Collins K. Varicose Veins: Diagnosis and Treatment. Am Fam Physician. 2019;99:682-688. [PubMed] |
| 4. | Li X, Yang B, Li X, Ren S. Prospective Comparison of Effect of Ligation and Foam Sclerotherapy with Foam Sclerotherapy Alone for Varicose Veins. Ann Vasc Surg. 2018;49:75-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Sun Y, Li X, Chen Z, Ren S. Feasibility and safety of foam sclerotherapy followed by a multiple subcutaneously interrupt ligation under local anaesthesia for outpatients with varicose veins. Int J Surg. 2017;42:49-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Li X, Fan L, Ren S, Li X. Outcomes of Foam Sclerotherapy plus Ligation versus Foam Sclerotherapy Alone for Venous Ulcers in Lower Extremities. Ann Vasc Surg. 2017;45:160-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Tew GA, Gumber A, McIntosh E, Kesterton S, King B, Michaels JA, Klonizakis M. Effects of supervised exercise training on lower-limb cutaneous microvascular reactivity in adults with venous ulcers. Eur J Appl Physiol. 2018;118:321-329. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Moses SL. A comparative study between aerobic exercise and onshore exercise on severity of pain and quality of life in women with varicose veins. IJMAES. 2021;. [DOI] [Full Text] |
| 9. | Tabata A, Kanai M, Horimatsu T, Tsuboyama T, Matsushima K, Kato T. Changes in upper extremity function, ADL, and HRQoL in colorectal cancer patients after the first chemotherapy cycle with oxaliplatin: a prospective single-center observational study. Support Care Cancer. 2018;26:2397-2405. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Wrona M, Jöckel KH, Pannier F, Bock E, Hoffmann B, Rabe E. Association of Venous Disorders with Leg Symptoms: Results from the Bonn Vein Study 1. Eur J Vasc Endovasc Surg. 2015;50:360-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 92] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 11. | Beebe-Dimmer JL, Pfeifer JR, Engle JS, Schottenfeld D. The epidemiology of chronic venous insufficiency and varicose veins. Ann Epidemiol. 2005;15:175-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 575] [Cited by in RCA: 605] [Article Influence: 30.3] [Reference Citation Analysis (0)] |
| 12. | Nicolaides AN, Allegra C, Bergan J, Bradbury A, Cairols M, Carpentier P, Comerota A, Delis C, Eklof B, Fassiadis N, Georgiou N, Geroulakos G, Hoffmann U, Jantet G, Jawien A, Kakkos S, Kalodiki E, Labropoulos N, Neglen P, Pappas P, Partsch H, Perrin M, Rabe E, Ramelet AA, Vayssaira M, Ioannidou E, Taft A. Management of chronic venous disorders of the lower limbs: guidelines according to scientific evidence. Int Angiol. 2008;27:1-59. [PubMed] |
| 13. | Lima M, Silva B, Rocha-Rodrigues S, Bezerra P. The impact of an 8-week Pilates-based physical training program on functional mobility: data from a septuagenarian group. BHK. 2021;1:11-19. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Zhang Q, Li YX, Li XL, Yin Y, Li RL, Qiao X, Li W, Ma HF, Ma WH, Han YF, Zeng GQ, Wang QY, Kang J, Hou G. A comparative study of the five-repetition sit-to-stand test and the 30-second sit-to-stand test to assess exercise tolerance in COPD patients. Int J Chron Obstruct Pulmon Dis. 2018;13:2833-2839. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 58] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 15. | Rikli RE, Jones CJ. Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist. 2013;53:255-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 450] [Cited by in RCA: 635] [Article Influence: 48.8] [Reference Citation Analysis (1)] |
| 16. | Feldmann A, Schmitz R, Erlacher D. Near-infrared spectroscopy-derived muscle oxygen saturation on a 0% to 100% scale: reliability and validity of the Moxy Monitor. J Biomed Opt. 2019;24:1-11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 81] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 17. | Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8080] [Cited by in RCA: 8098] [Article Influence: 158.8] [Reference Citation Analysis (0)] |
| 18. | Zhang C, Zhang H, Zhao M, Li Z, Cook CE, Buysse DJ, Zhao Y, Yao Y. Reliability, Validity, and Factor Structure of Pittsburgh Sleep Quality Index in Community-Based Centenarians. Front Psychiatry. 2020;11:573530. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 87] [Cited by in RCA: 75] [Article Influence: 15.0] [Reference Citation Analysis (1)] |
| 19. | Chun MY. Validity and reliability of korean version of international physical activity questionnaire short form in the elderly. Korean J Fam Med. 2012;33:144-151. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 228] [Cited by in RCA: 262] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 20. | Launois R, Mansilha A, Jantet G. International psychometric validation of the Chronic Venous Disease quality of life Questionnaire (CIVIQ-20). Eur J Vasc Endovasc Surg. 2010;40:783-789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 85] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 21. | Callam MJ. Epidemiology of varicose veins. Br J Surg. 1994;81:167-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 451] [Cited by in RCA: 422] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 22. | Eberhardt RT, Raffetto JD. Chronic venous insufficiency. Circulation. 2014;130:333-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 304] [Cited by in RCA: 418] [Article Influence: 38.0] [Reference Citation Analysis (0)] |
| 23. | Labropoulos N, Volteas N, Leon M, Sowade O, Rulo A, Giannoukas AD, Nicolaides AN. The role of venous outflow obstruction in patients with chronic venous dysfunction. Arch Surg. 1997;132:46-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 77] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 24. | Eklöf B, Rutherford RB, Bergan JJ, Carpentier PH, Gloviczki P, Kistner RL, Meissner MH, Moneta GL, Myers K, Padberg FT, Perrin M, Ruckley CV, Smith PC, Wakefield TW; American Venous Forum International Ad Hoc Committee for Revision of the CEAP Classification. Revision of the CEAP classification for chronic venous disorders: consensus statement. J Vasc Surg. 2004;40:1248-1252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1295] [Cited by in RCA: 1157] [Article Influence: 57.9] [Reference Citation Analysis (0)] |
| 25. | Marshansky S, Mayer P, Rizzo D, Baltzan M, Denis R, Lavigne GJ. Sleep, chronic pain, and opioid risk for apnea. Prog Neuropsychopharmacol Biol Psychiatry. 2018;87:234-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 42] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 26. | Ibrahim A, Zeynep Vildan Okudan A, Mehmet A, Vildan Y. Sleep quality and Laboratory Findings in Patients with Varicose Vein Leg Pain. J Neurosci Neurol Disord. 2023;7:022-026. [DOI] [Full Text] |
| 27. | Mok Y, Ishigami J, Sang Y, Kucharska-Newton AM, Salameh M, Schrack JA, Palta P, Coresh J, Windham BG, Lutsey PL, Folsom AR, Matsushita K. Clinically Recognized Varicose Veins and Physical Function in Older Individuals: The ARIC Study. J Gerontol A Biol Sci Med Sci. 2022;77:1637-1643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 28. | Yoshida S, Koshima I, Imai H, Uchiki T, Sasaki A, Fujioka Y, Nagamatsu S, Yokota K, Harima M, Yamashita S. Combined Lymphovenous Anastomosis and Great Saphenous Vein Stripping for Comorbid Lymphedema and Varicose Veins. Lymphat Res Biol. 2022;20:213-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 29. | Yoshida S, Koshima I, Imai H, Sasaki A, Fujioka Y, Nagamatsu S, Yokota K. Lymphatic flow restoration after stripping surgery for varicose veins: A case report. SAGE Open Med Case Rep. 2019;7:2050313X19849265. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |